Imagine being told you have lupus, then months later your doctor says you also have scleroderma-and then your lungs start acting up. You’re not alone. About one in four people with an autoimmune connective tissue disease will eventually develop symptoms of another. These aren’t just coincidences. They’re autoimmune overlap syndromes, where the body’s immune system attacks multiple systems at once, blurring the lines between well-known diseases like lupus, scleroderma, and myositis.
What Exactly Are Autoimmune Overlap Syndromes?
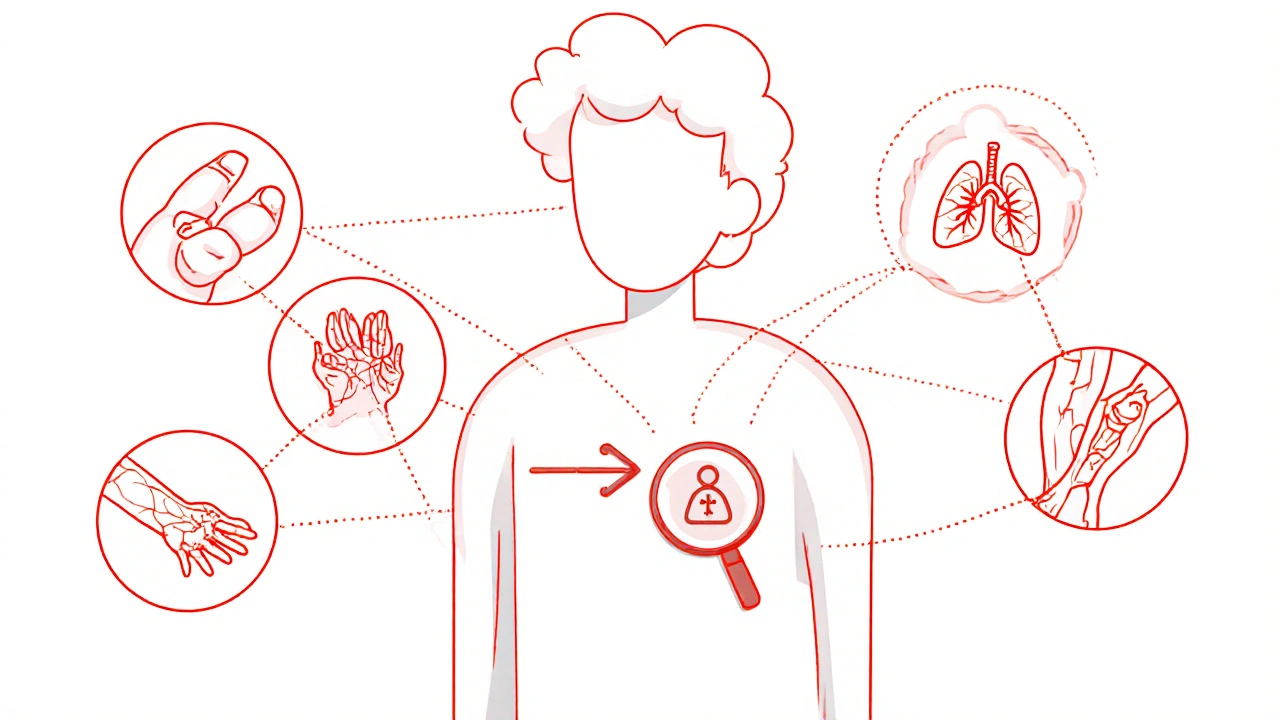
Autoimmune overlap syndromes happen when a person meets diagnostic criteria for two or more distinct connective tissue diseases (CTDs) at the same time or one after the other. The five classic CTDs involved are systemic lupus erythematosus (SLE), scleroderma, polymyositis/dermatomyositis, rheumatoid arthritis, and Sjögren’s syndrome. When these conditions mix, they don’t just add up-they create new, complex patterns that confuse even experienced doctors. One of the most studied examples is mixed connective tissue disease (MCTD). It’s defined by high levels of anti-U1-RNP antibodies-often above 1:10,000-and a mix of symptoms from lupus (like fatigue and joint pain), scleroderma (puffy fingers, skin thickening), and myositis (muscle weakness). Up to 95% of MCTD patients have Raynaud’s phenomenon, where fingers turn white or blue in the cold. Another common form is antisynthetase syndrome, marked by anti-Jo-1 antibodies. These patients often get severe muscle inflammation, interstitial lung disease (scarring in the lungs), and distinctive “mechanic’s hands”-cracked, dirty-looking skin on the palms and fingers. Then there’s PM/Scl overlap, where polymyositis and scleroderma appear together. Patients show skin tightening and muscle weakness, with about half developing lung scarring. And when three or more autoimmune diseases show up in one person, it’s called Multiple Autoimmune Syndrome (MAS). Type 2 MAS, for instance, often includes Sjögren’s, rheumatoid arthritis, and autoimmune thyroid disease-all happening in the same body.Why Diagnosis Is So Hard
There’s no single test for overlap syndromes. The American College of Rheumatology and European League Against Rheumatism have clear rules for diagnosing lupus or scleroderma individually-but not when they blend. That’s why 30-40% of patients initially labeled with “undifferentiated connective tissue disease” (UCTD) end up being reclassified as having an overlap syndrome within five years. The real clue lies in autoantibodies. Anti-U1-RNP is almost always present in MCTD (95% specificity). Anti-PM/Scl antibodies show up in 2-5% of scleroderma patients and 8-10% of myositis cases. Anti-Jo-1 is found in 75-80% of antisynthetase syndrome cases. These aren’t just markers-they’re diagnostic anchors. But here’s the catch: symptoms overlap so much that doctors often miss the bigger picture. A 2022 study in Cureus found that 45% of patients waited over 18 months for a correct diagnosis-double the delay of single-disease patients. One patient on Reddit described seeing seven specialists before someone connected her muscle pain, tight skin, and lung issues into one condition. “They treated me for one thing while ignoring the others,” she wrote. That’s the problem: fragmented care leads to fragmented diagnoses.The Hidden Threat: Interstitial Lung Disease
One of the most dangerous aspects of overlap syndromes is how often they affect the lungs. Up to 70% of people with antisynthetase syndrome develop interstitial lung disease (ILD)-scarring that slowly steals breath. In PM/Scl overlap, it’s about half. Left unchecked, ILD becomes irreversible. That’s why the European League Against Rheumatism (EULAR) now recommends that every suspected overlap patient get a high-resolution CT scan and pulmonary function tests. These aren’t optional extras-they’re essential. A 2023 FDA approval of tocilizumab for antisynthetase-associated ILD was a major milestone. In clinical trials, it cut disease progression by 55% compared to placebo. For patients who didn’t respond to steroids or methotrexate, this drug became a lifeline. But lung damage doesn’t always show up early. That’s why AI tools are now being tested. A 2022 study in Nature Medicine showed machine learning models could predict overlap syndrome development from electronic health records-with 82% accuracy-up to a year before symptoms appeared. That kind of early warning could change outcomes.
How Treatment Works (and When It Goes Wrong)
There’s no one-size-fits-all treatment. The starting point is usually low-dose corticosteroids (like prednisone) combined with one immunosuppressant-most often methotrexate or mycophenolate mofetil. If lung disease is present, rituximab is often added. For MCTD with severe arthritis, hydroxychloroquine may help. But here’s the trap: too many doctors reach for a cocktail of drugs. Dr. Mary Crow of Hospital for Special Surgery warned in JAMA Rheumatology that 35% of overlap patients are on three or more immunosuppressants, even though there’s little proof this improves outcomes. The risk? Serious infections. Patients on triple therapy have a 28% chance of getting pneumonia or sepsis-nearly double the risk of those on one or two drugs. It’s not aggressive treatment-it’s over-treatment. The key is targeting the dominant problem. If skin and joints are the main issue, focus there. If lungs are failing, prioritize lung protection. Treatment isn’t about checking every box-it’s about stopping the most dangerous process first.Care Coordination: The Missing Piece
Most patients with overlap syndromes see multiple specialists: a rheumatologist, a pulmonologist, a dermatologist, maybe a cardiologist. But who’s holding the whole picture together? Too often, no one. The Cleveland Clinic’s Overlap Syndrome Program found that adding a dedicated care coordinator-someone who schedules appointments, tracks test results, and communicates between teams-cut hospitalizations by 35% and boosted medication adherence by 42%. Patients reported feeling less lost and more in control. In Europe, 65% of tertiary centers follow EULAR’s 2020 guidelines for coordinated care. In North America, it’s only 40%. That gap matters. A 2022 survey by the Sjögren’s Foundation found that 68% of patients with Sjögren’s-lupus overlap struggled to get coordinated care-compared to 42% of those with just Sjögren’s. A single point of contact doesn’t mean one doctor does everything. It means someone makes sure the rheumatologist knows what the pulmonologist found, that the pharmacist checks for drug interactions, and that the patient isn’t drowning in pills with conflicting instructions.What’s Next? Precision Medicine and New Tools
The future of overlap syndromes is personalization. In January 2023, the NIH launched a $15 million project-the Overlap Syndrome Biomarker Consortium-to find specific biological signals that predict who will progress, who will respond to which drug, and who’s at highest risk for lung damage. New tools are also emerging. The American College of Rheumatology’s 2023 guidelines now push for “treat-to-target” goals: keep lung function above 80% predicted, skin score below 15, and arthritis in remission. These aren’t vague hopes-they’re measurable targets. Anifrolumab, a drug approved for lupus, is now in phase 2 trials for MCTD, with results expected by the end of 2024. If it works, it could offer a new option for patients who don’t respond to steroids. Meanwhile, researchers are building composite disease activity scores that combine muscle strength, skin thickness, joint pain, and lung function into one number-making it easier to track progress across multiple systems.
What Patients Need to Know
If you’re living with overlapping autoimmune symptoms, here’s what matters:- Get tested for specific autoantibodies-don’t settle for a general “autoimmune” label.
- Insist on a chest CT and pulmonary function tests-even if you feel fine breathing.
- Ask if your care team has a coordinator or case manager. If not, request one.
- Keep a symptom journal: note when skin tightens, when muscles weaken, when breathing changes.
- Be wary of triple immunosuppressant regimens. Ask: “Is this helping, or just adding risk?”
- Seek care at a center that specializes in complex autoimmune diseases. They see more cases, make fewer mistakes.
Frequently Asked Questions
Can autoimmune overlap syndromes be cured?
No, there is no cure yet. But many patients achieve long-term remission or stable disease with the right treatment plan. The goal isn’t to eliminate the disease completely-it’s to stop it from getting worse, protect vital organs like the lungs and heart, and maintain quality of life. Some patients stay in remission for years with low-dose medication.
Are overlap syndromes inherited?
They’re not directly inherited like cystic fibrosis or Huntington’s. But certain genes can increase risk. People with family members who have autoimmune diseases (like lupus, thyroiditis, or type 1 diabetes) are more likely to develop an overlap syndrome themselves. It’s a mix of genetic vulnerability and environmental triggers-like infections, stress, or toxins-that sets the immune system off track.
Why do I need so many tests if I already have a diagnosis?
Because overlap syndromes change over time. You might start with joint pain and Raynaud’s, but later develop lung scarring or muscle weakness. Regular testing-like lung function scans, blood work, and skin exams-catches those changes early. Waiting until you feel worse means damage may already be done. Early detection saves organs.
Can I still work or exercise with an overlap syndrome?
Yes-often with modifications. Many patients continue working full-time with proper pacing, workplace accommodations, and physical therapy. Low-impact exercise like swimming, walking, or yoga helps maintain muscle strength and joint flexibility. But pushing too hard can trigger flares. Listen to your body. A physical therapist familiar with autoimmune diseases can design a safe, effective routine.
What’s the difference between MCTD and lupus?
MCTD has high anti-U1-RNP antibodies and often includes puffy hands, severe Raynaud’s, and muscle weakness-features less common in classic lupus. Lupus typically has more kidney involvement, butterfly rash, and neurological symptoms. MCTD rarely causes severe kidney disease or seizures. The antibody test is the clearest differentiator.
How do I find a specialist who understands overlap syndromes?
Look for rheumatologists who specialize in connective tissue diseases or work at major academic medical centers. Johns Hopkins, Mayo Clinic, Hospital for Special Surgery, and Cleveland Clinic all have dedicated overlap syndrome programs. Ask if they see at least 20-30 overlap cases per year. Smaller practices often treat them as “complex lupus” or “mystery cases”-and miss the bigger picture.
All Comments
Melvina Zelee November 22, 2025
ive been living with this for 5 years and no one ever put it together until i started keeping a symptom journal. it was like someone finally turned on the light in a dark room. dont wait for them to figure it out-write it down, show them, and keep asking. your body is talking, even if theyre not listening yet.
Robin Johnson November 24, 2025
the real issue isnt the diagnosis-it’s the system. doctors treat symptoms like separate problems, not pieces of one broken machine. you need someone who sees the whole puzzle, not just one corner. find that person or become that person for yourself.
Latonya Elarms-Radford November 25, 2025
oh honey, let me tell you-this isnt just medicine, this is metaphysical. the body is a cathedral of suffering, and when the immune system turns against itself, its not a mistake-it’s a cry from the soul. the antibodies? they’re not just proteins, they’re echoes of ancestral trauma, of environmental poison, of the modern world screaming back at us through our flesh. i’ve read the papers, i’ve sat in silence with patients who weep because their lungs forget how to breathe, and let me say this: we are not just treating disease, we are healing the collective wound of civilization.
Mark Williams November 26, 2025
the anti-U1-RNP titers are the linchpin. without serological anchoring, you’re just chasing clinical noise. the real diagnostic power lies in the intersection of high-titer autoantibodies + multi-organ involvement + absence of isolated organ dominance. that’s the triad. everything else is noise.
Daniel Jean-Baptiste November 27, 2025
just wanted to say thanks for writing this. i had no idea i wasnt alone. my doc called it 'weird lupus' for years. turned out i had pm/scl. got the ct scan last year and found early fibrosis. started tocilizumab-my oxygen levels are up. still tired but alive. thanks for the hope.
Ravi Kumar Gupta November 28, 2025
in india, we dont even have access to these tests. my cousin had joint pain, skin tightness, cough-she was given painkillers for 2 years. when she finally got to a big hospital, they said 'you have three diseases at once.' how? we cant even afford one. this article is beautiful but it feels like a luxury for rich countries. what about the rest of us?
Rahul Kanakarajan November 28, 2025
you people are overcomplicating this. if you have muscle weakness + skin thickening + lung issues, you have overlap. stop waiting for antibodies. stop waiting for guidelines. if you feel it, demand the ct scan. if your doctor says 'wait and see,' get a new doctor. this isnt a mystery, its negligence.
David Cunningham November 30, 2025
chill. i had this too. took 4 years. got diagnosed after a random rheum doc asked if my fingers turned blue in the car AC. i said yeah. he said 'ok, we’re doing the full panel.' 3 months later: MCTD. sometimes the answer is just one question away. dont panic, just ask.
luke young December 1, 2025
thank you for this. i’ve been sharing this with my support group. we all felt so lost. now we have words for what we’re going through. the care coordinator tip? life-changing. my sister got one last year and her hospital visits dropped by half. small change, huge difference.
james lucas December 2, 2025
so many of us are just told 'its lupus' and sent on our way. but then your skin gets tight, your muscles ache, your lungs feel like sandpaper-why are they ignoring it? i kept saying 'something else is wrong' and they called me a hypochondriac. turns out i had antisynthetase. got the anti-Jo-1 test done on my own dime. now im on rituximab and breathing like a normal person again. dont let them gaslight you. trust your body.
Jessica Correa December 2, 2025
the part about triple immunosuppressants scared me. my doc put me on prednisone methotrexate and azathioprine because 'better safe than sorry.' i got pneumonia last winter. i almost died. now im on just one drug and im doing better. why do they think more drugs = better? it’s not a buffet. its a minefield.
Patrick Marsh December 4, 2025
Anti-U1-RNP >1:10,000. High-res CT. Pulmonary function tests. Care coordinator. These are non-negotiables.
New Yorkers December 6, 2025
the real tragedy? this is all predictable. the science has been here for a decade. but the medical system is still stuck in the 1990s. silos. ego. bureaucracy. patients are the collateral damage. you’re not broken. the system is.
manish chaturvedi December 6, 2025
in my village in India, we say: 'the body remembers what the mind forgets.' this article is a gift. thank you for naming the invisible. i will share this with every patient i meet. you have given us language. that is power.