DVT Risk Assessment Tool
Assess Your Deep Vein Thrombosis (DVT) Risk
This tool estimates your risk of developing a blood clot in the context of chronic venous insufficiency (CVI). Based on your responses, you'll receive a risk level and personalized recommendations.
Your Risk Assessment
Recommendations: Maintain healthy lifestyle habits including regular movement, proper hydration, and wearing compression stockings as recommended by your healthcare provider.
EMERGENCY: SEEK IMMEDIATE MEDICAL ATTENTION
Your symptoms may indicate a potentially life-threatening condition. Please call emergency services or go to the nearest emergency room immediately.
When veins in the legs can’t push blood back to the heart efficiently, you might hear the terms chronic venous insufficiency or CVI. But what does that have to do with blood clots? Understanding the connection can help you spot danger early, avoid serious complications, and choose the right treatment.
What Is Chronic Venous Insufficiency?
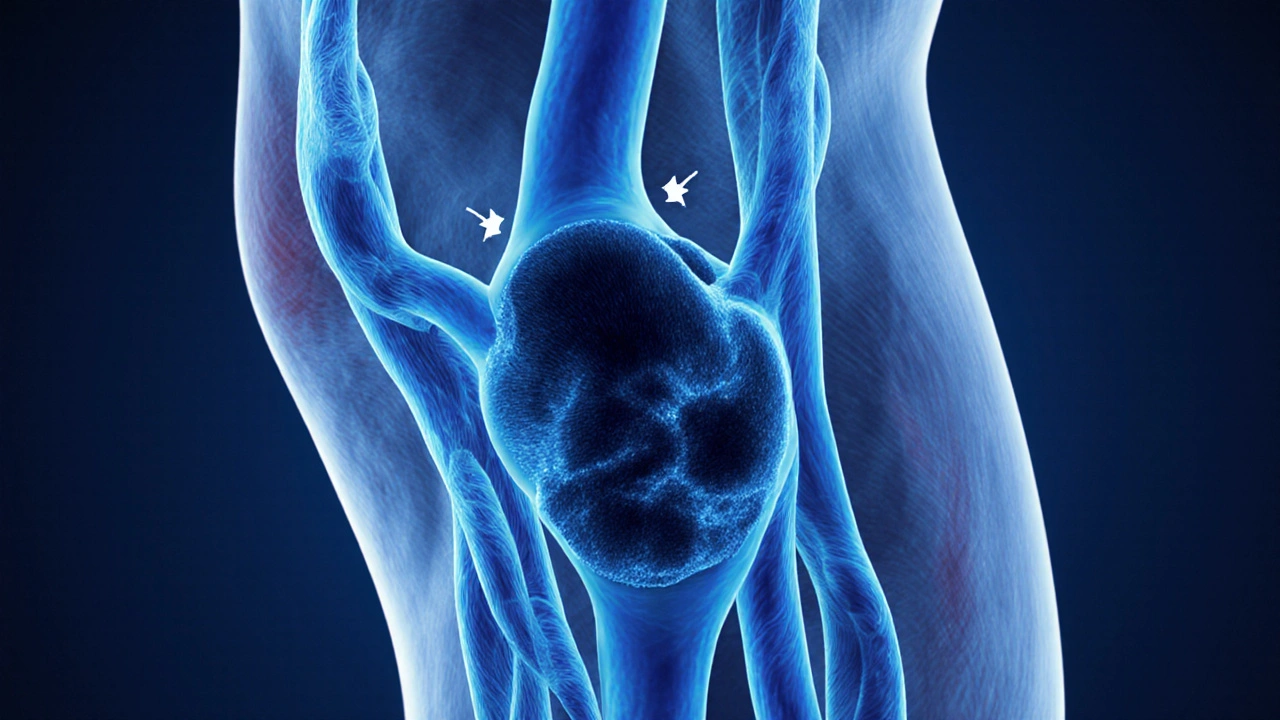
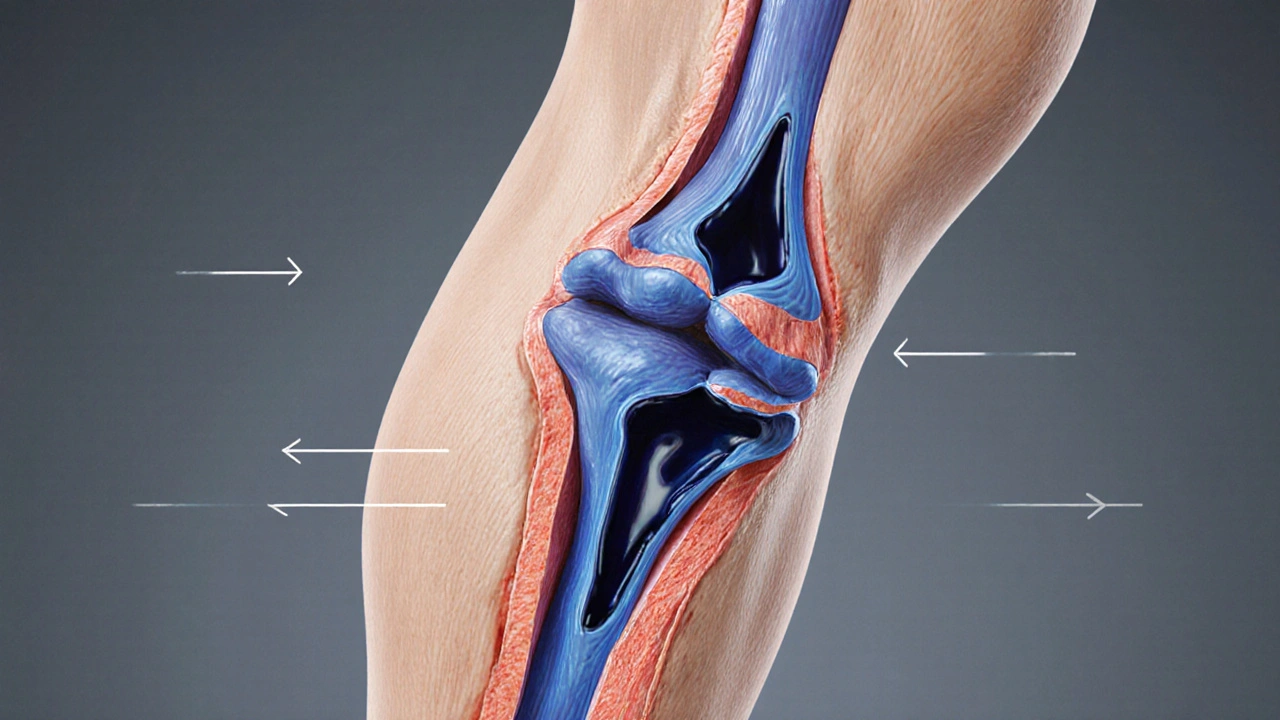
Chronic Venous Insufficiency is a condition where leg veins lose their ability to move blood upward, causing pooling, swelling, and skin changes. The underlying problem is often damaged or leaky venous valves, which normally act like one-way gates.
Typical signs include aching calves, heaviness, visible varicose veins, and, in advanced stages, skin discoloration or ulceration. According to a 2023 epidemiology report, about 25% of adults over 50 show early CVI signs, and the prevalence rises sharply with age.
How Blood Clots Fit Into the Picture
Blood clots-technically called Thrombus-form when blood solidifies inside a vessel. In the leg veins, a clot is most commonly known as Deep Vein Thrombosis (DVT). While CVI and DVT are separate diagnoses, they share several risk pathways.
Stagnant blood flow from vein valve failure creates a breeding ground for clot formation. Conversely, a clot can further damage the valve wall, worsening CVI. Studies from the British Venous Forum (2022) show that people with untreated CVI are 1.7times more likely to develop a DVT than those with healthy veins.
Key Risk Factors for Both Conditions
- Prolonged standing or sitting - common in retail, office jobs, and long flights.
- Obesity - excess weight increases pressure on leg veins.
- Age - vein elasticity declines after 40.
- Family history of clotting disorders or varicose veins.
- Hormonal influences - pregnancy, oral contraceptives, and hormone replacement therapy.
- Smoking - damages vessel walls and promotes clotting.
Identifying these factors early lets you target prevention before swelling turns into a painful ulcer or a life‑threatening clot.
Symptoms That Signal a Possible Clot in CVI
Both conditions share swelling and pain, but a few red‑flag signs point specifically to a clot:
- Sudden, sharp calf pain that feels like a cramp.
- Warmth and redness over the affected area.
- Visible vein hardening (a “cord”) under the skin.
- Shortness of breath, chest pain, or coughing up blood - possible signs of a clot that has traveled to the lungs (pulmonary embolism).
If any of these appear, seek medical assessment right away.
How Doctors Diagnose CVI and Clots
Modern imaging makes it easy to differentiate swelling from a clot. The primary tools are:
| Test | Purpose | Typical Findings |
|---|---|---|
| Duplex Ultrasound | Assess blood flow, valve competence, and clot presence | Reversed flow in reflux; echogenic clot in deep veins |
| Venography | Gold‑standard for detailed vein mapping | Contrast filling defects indicate clot |
| D-dimer Blood Test | Screen for active clotting | Elevated levels suggest recent clot formation |
| CT or MRI Angiography | Identify complications like pulmonary embolism | Blocked pulmonary arteries or clot migration |
Most clinicians start with a duplex ultrasound because it’s non‑invasive, quick, and accurate for both reflux (CVI) and clot detection (DVT).
Treatment Pathways: From Compression to Anticoagulation
Therapy depends on whether you’re dealing with isolated CVI, an acute clot, or both.
Compression Therapy
Compression therapy involves wearing specially fitted stockings or bandages that apply graduated pressure-from the ankle upward-to push fluid back toward the heart.
- Low‑profile (15-20mmHg) for mild CVI.
- Moderate (20-30mmHg) for moderate swelling or after a DVT.
- High (30‑40mmHg) for severe ulcer‑prone skin.
Clinical trials in 2024 showed a 45% reduction in ulcer recurrence when patients adhered to proper compression for six months.
Anticoagulant Medication
When a clot is confirmed, doctors prescribe anticoagulants to stop further clot growth and allow the body to dissolve the existing clot. Options include:
- Direct oral anticoagulants (DOACs) such as apixaban or rivaroxaban-no routine blood monitoring needed.
- Warfarin-requires regular INR checks, but is cheaper for long‑term use.
Duration typically ranges from three to six months for a first‑time DVT, extending to indefinite therapy if clot risk remains high.
Interventional Procedures
In severe CVI with ulceration, minimally invasive procedures like endovenous laser therapy (EVLT) or radiofrequency ablation (RFA) close incompetent veins, improving circulation and reducing clot risk.

Everyday Steps to Lower Your Risk
Beyond medical treatment, lifestyle tweaks make a big difference:
- Move every hour-stand up, stretch, or walk for two minutes.
- Maintain a healthy weight-aim for a BMI under 25.
- Stay hydrated-makes blood less sticky.
- Elevate legs while resting-use a pillow to keep them above heart level.
- Wear loose clothing-avoid tight socks or waistbands that restrict flow.
For those on long flights, a compression stocking and occasional calf raises can prevent both swelling and clot formation.
When to Call a Doctor Immediately
Even if you’ve been managing CVI for years, sudden changes warrant urgent attention:
- Rapid increase in leg size or pain.
- Redness, warmth, or a hard cord-like vein.
- Shortness of breath, chest discomfort, or coughing up blood.
These symptoms could signal a new clot or a pulmonary embolism, both medical emergencies.
Key Takeaways
- CVI weakens vein valves, leading to blood pooling and a higher chance of clot formation.
- Recognize red‑flag symptoms-sharp calf pain, warmth, sudden swelling, and respiratory signs.
- Duplex ultrasound is the go‑to test for both reflux and DVT.
- Compression therapy is the cornerstone for CVI; anticoagulants treat confirmed clots.
- Regular movement, weight control, and proper leg elevation keep both problems at bay.
Frequently Asked Questions
Can I develop a blood clot if I already have chronic venous insufficiency?
Yes. Stagnant blood caused by valve failure in CVI creates an environment where clots can form, especially if other risk factors like immobility or obesity are present.
How long should I wear compression stockings after a DVT?
Most guidelines recommend at least three months of graduated compression (20‑30mmHg) after the clot resolves, then reassessment based on vein function and symptom relief.
Is swelling alone enough to diagnose CVI?
Swelling is a common sign, but a definitive CVI diagnosis requires imaging-usually duplex ultrasound-to confirm valve reflux and rule out other causes.
Can lifestyle changes replace medication for preventing clots?
Lifestyle measures significantly lower risk but don’t eliminate it for high‑risk patients. Anticoagulants remain essential after an acute DVT, while compression and movement support long‑term prevention.
What are the signs of a pulmonary embolism that can follow a leg clot?
Sudden shortness of breath, sharp chest pain that worsens with breathing, rapid heart rate, and coughing up blood are classic warning signs. Treat as an emergency.
All Comments
Ben Hooper October 12, 2025
Blood clots and CVI are linked because stagnant blood encourages clot formation. The article covers the basics well.
Marjory Beatriz Barbosa Honório October 21, 2025
Wow, this post really shines a light on a topic that many of us overlook in our daily hustle. I love how it mixes solid medical facts with practical tips that anyone can follow, from busy parents to office warriors. The colorful breakdown of risk factors feels like a friendly guide rather than a scary lecture. Keep spreading the word and empowering people to take charge of their leg health, you’re doing awesome work.
G.Pritiranjan Das October 31, 2025
Great summary, staying active can really help.
Karen Wolsey November 10, 2025
Oh sure, just stand up every hour and the world’s problems vanish. It’s not like we have deadlines or meetings that chain us to our desks. A little movement won’t magically erase years of vein damage though. Still, a sarcastic nod to the advice is better than ignoring it.
Trinity 13 November 19, 2025
When you first hear the term chronic venous insufficiency, it can feel like another medical buzzword that belongs on a hallway poster rather than your personal health checklist.
But the reality is that the leg veins are literally fighting a losing battle against gravity, and the valves that are supposed to act like one‑way doors start to leak.
That leakage creates a backpack of blood that hangs around the lower extremities, making your calves feel heavy, achy, and sometimes even swollen.
Now throw a clot into that mix and you’ve got a perfect storm that can turn a simple ache into a life‑threatening emergency.
The article does a solid job of laying out the anatomy of the problem, the risk factors that stack up like dominoes, and the warning signs that should set off alarm bells.
I especially appreciate the way it breaks down everyday habits-like sitting for marathon meetings or scrolling on the couch for hours-as hidden culprits that most of us never consider.
Compression stockings get a lot of love here, and for good reason; they’re like the unsung heroes that apply gentle pressure to coax blood back toward the heart.
If you’ve ever tried those tight socks and felt a bit of relief, you know they’re not just a fashion statement.
On the medication side, the piece mentions direct oral anticoagulants, which have made the whole anticoagulation game less of a hassle compared to warfarin’s weekly blood draws.
That said, nothing replaces a good conversation with your doctor, especially when you’re juggling multiple risk factors like obesity, smoking, or hormonal therapy.
Imaging is another star of the show-duplex ultrasound is quick, painless, and can spot both reflux and clots in one sweep.
If you’re ever on a long flight, toss on a pair of compression stockings, do some calf raises, and keep the blood moving, otherwise you might end up writing a different kind of post about a pulmonary embolism.
Lifestyle changes may sound like a bore, but swapping a soda for water, taking the stairs, and maintaining a healthy weight can shave years off your risk profile.
I’ve seen patients who thought a little leg elevation was a waste of time, only to watch their swelling melt away after a few weeks.
Bottom line: stay aware, stay active, and don’t wait for the pain to crescendo before you seek help.
Your legs carry you through life-treat them with the respect they deserve, and the rest of you will thank you.
Rhiane Heslop November 29, 2025
The government should prioritize funding for vein health, not waste money on flashy tech that ignores real prevention.
Dorothy Ng December 8, 2025
The information presented aligns with current clinical guidelines and offers a clear roadmap for patients seeking to manage CVI and reduce clot risk.
Justin Elms December 18, 2025
Exactly right. Keep moving and wear your stockings. It really works.
Jesse Stubbs December 28, 2025
The piece feels like a recycled brochure, lacking depth and the urgency that a condition as serious as DVT deserves.
Melissa H. January 6, 2026
Love the thoroughness 😊 the guide covers everything from risk factors to treatment options and really drives home how important early detection is.
Poppy Johnston January 16, 2026
Great summary guys, remember to stay active and support each other in adopting healthy habits for better leg health.