Osteoporosis Treatment Eligibility Checker
Is PTH Therapy Right for You?
This tool helps determine if you meet the primary eligibility criteria for Parathyroid Hormone therapy based on current clinical guidelines.
When a bone‑weakening disease like osteoporosis feels like a dead end, many patients wonder if there’s a treatment that actually builds bone rather than just slowing loss. parathyroid hormone does exactly that - it’s the only approved therapy that nudges the skeleton to grow new, stronger tissue. Below, we unpack how this hormone works, which drugs harness its power, and what you should watch for when it becomes part of your osteoporosis plan.
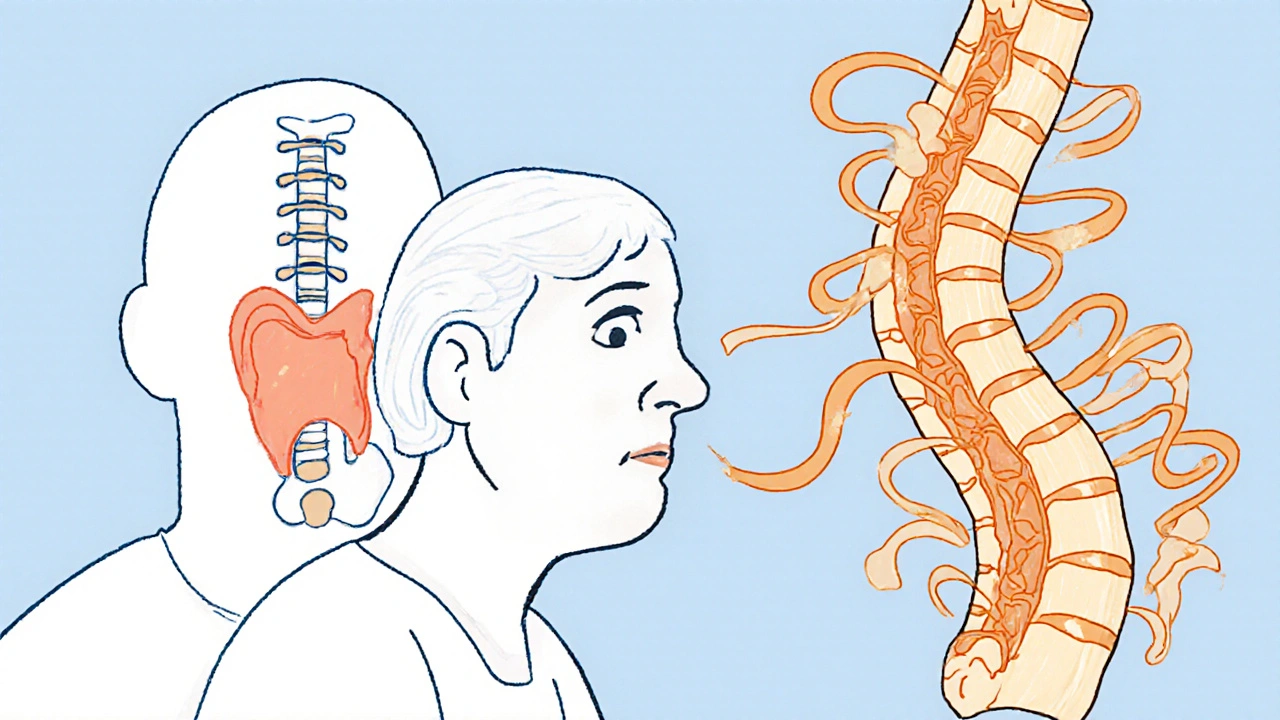
What is Parathyroid Hormone and Why It Matters for Bone
Parathyroid Hormone is a protein secreted by the four tiny glands behind your thyroid. Its main job is to keep blood calcium levels steady by balancing calcium release from bone, kidney reabsorption, and intestinal absorption. In a healthy adult, PTH spikes briefly after a meal, then drops, creating a daily rhythm that subtly stimulates bone remodeling - the process where old bone is resorbed and new bone is laid down.
When that rhythm is disrupted, bone loss can outpace formation, leading to osteoporosis. Researchers discovered that giving patients a low, continuous dose of PTH flips the script: instead of promoting resorption, it tips the balance toward formation, increasing bone mass and improving micro‑architecture.
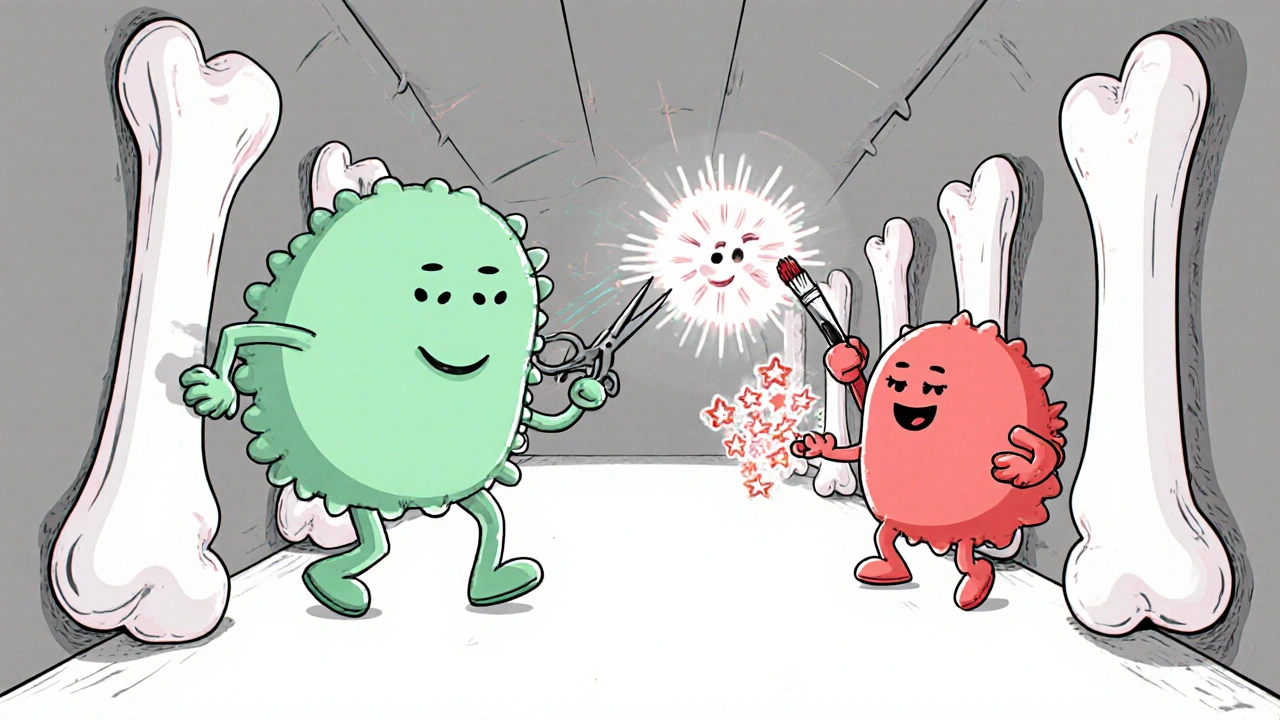
Bone Remodeling 101: The Cellular Dance
Bone is never static. Two cell types dominate the scene:
- Osteoclasts break down old bone (resorption).
- Osteoblasts lay down fresh bone matrix (formation).
PTH’s intermittent exposure preferentially activates osteoblasts, raising Bone Mineral Density (BMD) in the spine and hip - the sites most prone to fracture.
Therapeutic Forms of PTH: From Molecule to Medication
Two synthetic analogues dominate the market:
- Teriparatide (brand name Forteo) - the first‑in‑class daily injection that contains the first 34 amino acids of the natural hormone.
- Abaloparatide (brand name Tymlos) - a slightly tweaked version that binds a different receptor conformation, promising a lower calcium‑spike risk.
A newer player, Romosozumab, works by inhibiting sclerostin, effectively combining anabolic and anti‑resorptive actions. While not a direct PTH molecule, it’s often discussed alongside PTH‑based drugs because of its bone‑building promise.
Clinical Evidence: Do the Numbers Back Up the Hype?
The pivotal Phase III trials for teriparatide enrolled over 2,000 postmenopausal women with severe osteoporosis. After 18 months, vertebral fracture risk fell by 65 % compared with placebo, and hip fractures dropped 50 %. BMD gains averaged 9 % at the lumbar spine and 3 % at the total hip.
Abaloparatide’s pivotal ACTIVE trial showed a 43 % reduction in new vertebral fractures and a 72 % drop in non‑vertebral fractures over 18 months. Importantly, calcium excursions were 30 % less pronounced than with teriparatide, a finding that matters for patients with kidney stones or hypercalcemia concerns.
Romosozumab’s FRAME study (women) and ARCH study (men) reported a 73 % vertebral fracture reduction in the first year, but a signal of higher cardiovascular events sparked FDA warnings, limiting its use to patients who can’t tolerate other options.
How PTH Therapy Stacks Up Against Antiresorptives
| Feature | Teriparatide | Abaloparatide | Bisphosphonates (e.g., Alendronate) | Denosumab |
|---|---|---|---|---|
| Mechanism | Stimulates osteoblast activity | Stimulates osteoblasts via PTH1R | Inhibits osteoclast-mediated resorption | RANKL inhibition → less osteoclast formation |
| Typical dosing | 20 µg subcut daily | 80 µg subcut daily | Weekly oral tablet | 60 mg subcut every 6 months |
| Maximum treatment length | 24 months | 24 months | Indefinite (monitor renal function) | Indefinite (monitor calcium) |
| FDA approval year | 2002 | 2017 | 1995 (first‑gen) | 2010 |
| Common side effects | nausea, hypercalcemia | headache, mild hypercalcemia | esophagitis, musculoskeletal pain | skin infection, hypocalcemia |
In short, anabolic agents like teriparatide and abaloparatide build new bone, while antiresorptives merely slow loss. For patients with multiple fractures or very low BMD, the anabolic route often yields the biggest jump in strength.
Practical Considerations Before Starting PTH Therapy
- Eligibility: Generally reserved for postmenopausal women or men over 50 with a T‑score ≤ ‑2.5 and at least one fragility fracture.
- Baseline labs: Serum calcium, 25‑hydroxy‑vitamin D, renal function, and PTH levels. Correct vitamin D deficiency (<30 ng/mL) before injection.
- Administration: Daily self‑injection in the abdomen, thigh, or upper arm. Rotate sites to avoid lipohypertrophy.
- Monitoring: Check calcium and creatinine after the first month, then every 3-6 months. Bone density scan (DXA) at 12‑month intervals.
- Duration limit: 24 months max due to diminishing returns and potential osteosarcoma risk observed in animal studies (very rare in humans).
- Transition strategy: After completing an anabolic course, switch to a potent antiresorptive (e.g., denosumab) to preserve gains.
Patients with a history of skeletal malignancy, hyperparathyroidism, or unexplained hypercalcemia should avoid PTH analogues.

Cost, Insurance, and Access
Therapy costs run between £1,500 - £2,000 per month in the UK, but many NHS and private insurers cover a portion for high‑risk patients. The FDA (U.S.) and the European Medicines Agency (EMA) both restrict use to those who have failed or cannot tolerate other medications, so documentation of prior treatment failures is essential.
Decision Checklist: Is PTH Therapy Right for You?
- Severe osteoporosis (T‑score ≤ ‑2.5) with one or more fragility fractures?
- Vitamin D sufficient (≥30 ng/mL) and calcium intake >1,000 mg/day?
- No active cancer, hyperparathyroidism, or high baseline calcium?
- Ability to self‑inject daily for up to two years?
- Insurance or NHS approval for anabolic therapy?
If you tick most boxes, discuss an anabolic trial with your endocrinologist or bone specialist.
Frequently Asked Questions
Can PTH therapy reverse osteoporosis?
It can markedly increase bone density and reduce fracture risk, but “reverse” depends on baseline severity. Most patients see a 5‑10 % BMD gain in the spine after 18 months.
What are the most common side effects?
Mild nausea, transient hypercalcemia, and occasional injection‑site redness. Severe hypercalcemia is rare and usually linked to excessive calcium supplementation.
Do I need to take calcium supplements while on PTH?
Yes, most guidelines recommend 1,000‑1,200 mg of elemental calcium daily, split between diet and supplements, to support the anabolic effect and prevent hypocalcemia after stopping therapy.
How long does the benefit last after stopping?
Bone density gains plateau once treatment ends, but they do not disappear immediately. Switching to an anti‑resorptive agent can preserve up to 80 % of the acquired BMD.
Is there a risk of bone cancer?
Animal studies showed a very low incidence of osteosarcoma at high doses. In humans, the risk is considered negligible, but the therapy is limited to 24 months as a precaution.
Understanding how Parathyroid Hormone reshapes bone gives patients a powerful option when conventional drugs fall short. Talk to your doctor, get the labs right, and weigh the benefits against the injection commitment - the payoff can be a sturdier skeleton and fewer broken bones.
All Comments
Harry Bhullar October 21, 2025
Parathyroid hormone therapy is one of those rare treatments that actually adds bone instead of just slowing its loss, and that fact alone makes it worth a deep dive. When you inject teriparatide or abaloparatide daily, you’re essentially giving your skeleton a gentle, intermittent nudge that tells osteoblasts to get to work, building new matrix and increasing mineralization. The timing is crucial – a brief spike followed by a rapid decline mimics the body’s natural post‑prandial surge, and that pattern has been shown to favor formation over resorption in multiple animal models. Clinical trials consistently demonstrated that after about 18 months of therapy, patients see roughly a 9 % increase in lumbar spine BMD and a 3 % bump at the hip, which translates into dramatically lower fracture rates. Those numbers are not just statistical artifacts; they represent real, functional improvements that keep people out of the ER after a fall. What’s also cool is that the anabolic effect doesn’t disappear immediately when you stop the injections – the newly formed bone stays put, especially if you transition to an anti‑resorptive like denosumab right after the course ends. Of course, the therapy isn’t for everyone; you need to have a T‑score of ≤ ‑2.5, at least one fragility fracture, and be able to handle daily sub‑cutaneous injections for up to two years. Baseline labs are a must – check calcium, vitamin D, renal function, and make sure you’re not hypercalcemic before you start. Many patients wonder about calcium supplementation, and the answer is usually yes, about 1,000 mg daily split between diet and pills, to support the anabolic process and prevent hypocalcemia after stopping. Side‑effects are generally mild – a little nausea or transient hypercalcemia, which can be mitigated by adjusting calcium intake. The big scare about osteosarcoma comes from rodent data at very high doses; in humans the risk is essentially negligible, which is why the FDA caps the treatment length at 24 months as a precaution. If you’re on a bisphosphonate and haven’t had a fracture, you might want to try an anti‑resorptive first, but for those with multiple fractures or very low BMD, jumping to an anabolic agent gives the biggest bang for the buck. Insurance can be a hurdle, but many plans cover it if you meet the strict criteria, and some patient assistance programs are available. In practice, I’ve seen patients go from frequent vertebral fractures to a period of stability that lasts years after the therapy, especially when you follow up with bone density monitoring. Bottom line: PTH analogues are a powerful tool in the osteoporosis arsenal, but they require commitment, proper lab work, and a clear plan for what comes after the 24‑month window.
Lolita Gaela October 30, 2025
The pharmacodynamics of teriparatide and abaloparatide hinge on their selective activation of the PTH1 receptor's G‑protein‑coupled pathways, favoring the cAMP/PKA cascade that drives osteoblastic transcription factors such as RUNX2 and osterix. In contrast, intermittent dosing attenuates the RANKL‑mediated osteoclastogenesis that predominates under continuous exposure, which is why the anabolic window is preserved. Moreover, abaloparatide’s higher affinity for the RG conformational state of the receptor reduces intracellular calcium flux, accounting for its lower hypercalcemia profile observed in the ACTIVE trial. The dosing regimen-20 µg vs 80 µg daily-also reflects the differential potency and receptor kinetics, with the higher dose required to achieve comparable BMD gains due to its altered binding kinetics. From a clinical pharmacology standpoint, renal clearance is negligible, but hepatic metabolism via CYP3A4 contributes to the peptide’s half‑life, necessitating caution with strong inducers. The integration of these agents into a sequenced therapeutic algorithm typically involves an anti‑resorptive bridge post‑anabolic phase to consolidate the BMD gains, leveraging the anti‑remodeling effect of bisphosphonates or denosumab to maintain the newly formed bone matrix.
erica fenty November 9, 2025
Great overview! 👍👍👍
eric smith November 18, 2025
Wow, you really think a few bullet points are enough to cover the depths of endocrine bone remodeling? Let me guess, you also believe that "great overview" means the article is flawless. Spoiler: the devil's in the dosing details and the side‑effect nuances, which you totally brushed aside. Maybe next time actually read the trial protocols before applauding.
Erika Thonn November 27, 2025
i think we are all looking for a deeper meaning in the way bones rebuild themselves, like a philosphical rebirth of the skeleton after the caps of human frailty. the hormone is more than a molecule; it is a whisper of life unto the marrow, a reminder that even the hardest matter can be reshaped by a gentle pulse. some say that taking a daily injection is a commitment, but i see it as a ritual, a tiny act of faith in the body's own resilience. yet we must not forget the shadows – the hypercalcemic spikes that can stir trouble in the kidneys, the rare whispers of tumor that haunt the back of every researcher's mind. i beleive that every patient should weigh their own story against these risks, like a poet weighing each word before a line. in the end, thechoice to heal is as personal as the choice to write one's own destiny.
Rachel Valderrama December 6, 2025
Oh, look at us getting all deep and poetic about bone health – because that's exactly what the FDA wants to hear when they approve a drug! Sure, let's romanticize a daily needle and ignore the fact that most patients just want something that works without turning their lives into a sci‑fi experiment. But hey, if chanting about "resilience" helps you sleep at night, go for it. Meanwhile, the real world still needs clear guidance, not metaphors.
Brandy Eichberger December 16, 2025
While the therapeutic landscape for osteoporosis has indeed broadened, one must appreciate the nuanced hierarchy of evidence that situates anabolic agents as a premium intervention for high‑risk cohorts. The elegance of leveraging the PTH1R signaling axis lies not merely in its capacity to augment bone mass, but also in its ability to rejuvenate the microarchitectural integrity of trabecular compartments, as evidenced by high‑resolution peripheral quantitative computed tomography studies. Moreover, the strategic sequencing of anabolic followed by anti‑resorptive therapy embodies a sophisticated understanding of bone remodeling dynamics, optimizing both the accrual and preservation of newly formed tissue. It is incumbent upon clinicians to balance these mechanistic insights with pragmatic considerations such as patient adherence, comorbidity profiles, and health‑system reimbursement pathways. In doing so, we ensure that the deployment of these advanced therapeutics aligns with both scientific rigor and patient‑centered care.
Chirag Muthoo December 25, 2025
Indeed, the considerations outlined above merit a measured approach. Prior to initiating any anabolic regimen, a comprehensive assessment-including dual‑energy X‑ray absorptiometry, serum calcium, 25‑hydroxy‑vitamin D, and renal function-should be performed in accordance with established clinical guidelines. Following the 24‑month therapeutic window, transitioning to a bisphosphonate or denosumab is advisable to consolidate gains, as longitudinal data demonstrate sustained BMD preservation under such sequential therapy. It is also prudent to document patient consent and educate regarding potential adverse effects, particularly transient hypercalcemia, to ensure vigilant monitoring. This systematic protocol upholds both efficacy and safety within the therapeutic continuum.