ADHD Growth Tracking Tool
Track Your Teen's Growth
This tool helps you monitor height and weight changes while taking ADHD medication. According to research, 89% of teens who experience slowed growth catch up to their expected height by age 25.
Add Measurement
What to Look For
Normal growth: Height and weight typically follow percentile lines (25th, 50th, 75th) on standard growth charts.
Red flags (consult doctor):
- Weight loss over 10% of body weight
- Height falling below the 5th percentile
- Growth velocity drops below the 25th percentile
Growth Chart
Note: Standard growth charts are based on CDC data for U.S. teens. Your teen's growth may differ based on genetics and other factors.
When a teenager starts ADHD medication, parents often focus on the big wins: better grades, fewer outbursts, less chaos at home. But there’s another side to the story-one that doesn’t get talked about enough. ADHD medication can quietly affect how a teen grows, what they eat, and how they feel day to day. These aren’t rare side effects. They’re common. And if you’re not watching for them, they can sneak up on you.
How ADHD Medications Work-and What They Do to the Body
Most teens prescribed ADHD meds are taking stimulants: methylphenidate (like Ritalin or Concerta) or amphetamines (like Adderall or Vyvanse). These drugs work by boosting dopamine and norepinephrine in the brain, especially in the prefrontal cortex. That’s the part responsible for focus, planning, and impulse control. For about 70 to 80% of teens, this means fewer distractions, better homework completion, and calmer interactions. But the brain isn’t the only place these drugs act. They also affect the body’s hunger signals, metabolism, and even growth pathways. The same mechanism that helps a teen sit still in class can also shut down appetite. It’s not a bug-it’s a feature of how these medications work. That’s why appetite loss is reported in 50 to 80% of teens on stimulants, according to studies in Pediatric Clinics of North America.Appetite Suppression: The Silent Hunger Crisis
Imagine this: your teen takes their medication at 7 a.m. By 10 a.m., lunchtime rolls around, and they say they’re not hungry. They pick at a granola bar. Skip lunch entirely. By the time they get home at 4 p.m., they’re starving-but the medication is still kicking in. They eat a whole pizza. Then cookies. Then leftovers from dinner. This isn’t rebellion. It’s biology. A 2023 thread on ADDitude Magazine’s forum had 147 parents sharing similar stories. Two-thirds said their teens ate less than 300 calories during school hours. One parent wrote, “My 14-year-old used to be at the 50th percentile for weight. After 8 months on Concerta, he dropped to the 15th. We had to switch meds.” The problem isn’t just calories. It’s nutrition. Skipping meals means missing protein, iron, calcium, and vitamin D-all critical for growing bodies. Teens on ADHD meds often get enough energy later in the day, but it’s too late to support bone growth, muscle development, or brain maturation.Growth: The Long-Term Question
Growth suppression is the most concerning side effect for many parents. Studies show teens on stimulants may grow 1.39 to 2.55 centimeters (about half an inch to one inch) less than expected over several years. That’s not nothing. But here’s what most people don’t realize: it’s not permanent for most. The 2023 follow-up to the landmark MTA study found that 89% of teens who had slowed growth caught up to their genetic height potential by age 25. Only 11% had a lasting reduction of more than 1.5 cm. That’s a key point: delayed growth isn’t the same as stunted growth. There’s also a difference between medication types. Amphetamines like Vyvanse show slightly more growth suppression than methylphenidate-based drugs. A 2019 meta-analysis found that after three years, teens on amphetamines were about 1.7 cm shorter on average than those on methylphenidate, which averaged 1.1 cm. Non-stimulants like atomoxetine (Strattera) have almost no effect on growth-but they’re also less effective at managing core ADHD symptoms, working for only about 60% of teens compared to 75% with stimulants.
What Does Monitoring Actually Look Like?
The American Academy of Pediatrics doesn’t just say “watch for side effects.” They give exact steps:- Measure height and weight at the start of treatment
- Check again every 3 months during the first year
- Then every 6 months after that
What to Do When Growth Slows or Appetite Vanishes
You don’t have to choose between managing ADHD and letting your teen grow. There are practical fixes. Meal timing matters. Give a high-calorie, protein-rich breakfast before the medication kicks in. Think scrambled eggs with cheese, peanut butter on whole grain toast, or a smoothie with banana, nut butter, and Greek yogurt. A 2022 CHADD survey found that 31% of parents who used this strategy saw no weight loss at all. Snacks are non-negotiable. Keep calorie-dense snacks handy: trail mix, cheese sticks, whole milk yogurt, avocado slices, or even a small jar of nut butter. Teens on stimulants often eat better after school. Make sure those evening meals are packed with nutrients. Medication holidays. Many pediatric psychiatrists support short breaks during summer or school holidays. A 2020 study in the Journal of Attention Disorders found 73% of clinicians recommended this. One 16-year-old in Exeter started taking a break every July and August. By the time school started again, he’d gained back 3 pounds and grown 0.8 cm-enough to stay on track. Medication switches. If weight loss is severe (over 10% of body weight), switching from an amphetamine to a methylphenidate-based drug, or even to a non-stimulant, can help. Newer formulations like Adhansia XR, approved by the FDA in 2023, were designed to reduce appetite suppression-and early data shows 18% less weight loss than older versions.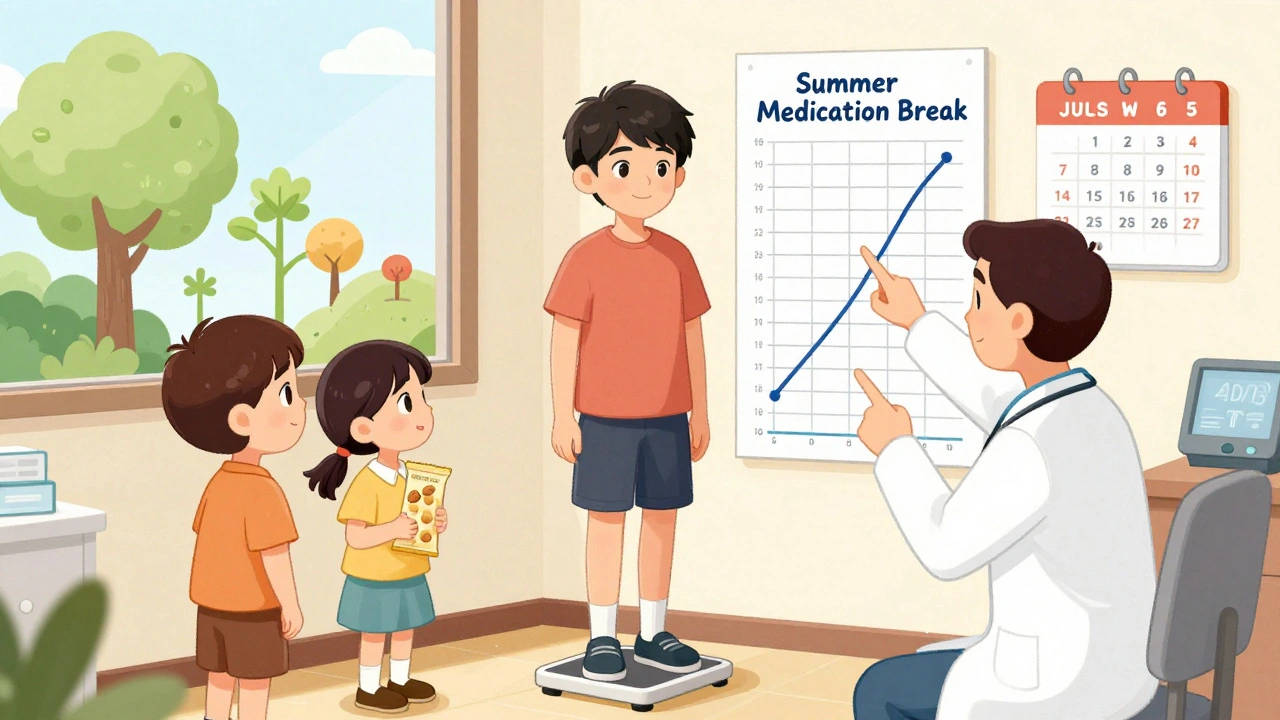
When to Worry-and When to Relax
It’s easy to panic when your teen’s growth curve dips. But here’s the reality: less than 10% of teens experience clinically significant growth suppression, according to the AAP’s 2019 guidelines. Most of the time, it’s mild and reversible. The real red flags:- Weight loss over 10% of body weight
- Height falling below the 5th percentile
- Significant fatigue, mood swings, or sleep problems that don’t improve
The Bigger Picture: Benefits vs. Risks
Dr. Joseph Biederman from Harvard puts it plainly: “The height reduction seen in some studies is clinically insignificant when weighed against the benefits.” Teens on effective ADHD treatment are less likely to drop out of school, get into trouble with the law, or develop anxiety and depression. A 2023 study in the Journal of the American Academy of Child & Adolescent Psychiatry showed that teens who stayed on medication had a 40% lower risk of developing substance use disorders by age 21. That’s huge. The goal isn’t to avoid medication. It’s to use it smartly. That means tracking growth, feeding well, adjusting doses, and knowing when to pause or switch.What’s Next? Personalized ADHD Care
The future of ADHD treatment is getting smarter. Companies like Genomind are using genetic testing to predict how a teen will respond to certain medications. Their 2022 trial found that when dosing was guided by CYP2D6 gene results, growth-related side effects dropped by 40%. The AAP is updating its guidelines in late 2024 to include clearer thresholds for intervention. The NIH has also launched the Growth and ADHD Longitudinal Study (GALS), a $4.2 million project to finally answer the big question: How much does long-term use really affect adult height? For now, the message is clear: ADHD meds work. But they need monitoring. Not because they’re dangerous-but because they’re powerful. And powerful tools require careful handling.Do ADHD medications permanently stunt growth in teens?
No, most teens catch up. Studies show that about 89% of adolescents who experience slowed growth while on stimulant medication reach their expected adult height by age 25. The average height difference is less than an inch, and it’s usually temporary. Growth slows most during the first year of treatment, then often resumes once the body adjusts or during medication breaks.
How can I help my teen eat enough on ADHD meds?
Time meals before the medication kicks in-offer a high-calorie, protein-rich breakfast before school. Keep nutrient-dense snacks available: cheese, nuts, nut butter, yogurt, smoothies. Encourage big, balanced dinners when the medication wears off. Avoid forcing meals during peak medication hours; instead, focus on calories later in the day. Many teens eat 2,000+ calories after 5 p.m. when the drug’s effect fades.
Should I stop ADHD meds if my teen is losing weight?
Don’t stop without talking to your doctor. Weight loss of more than 10% of body weight is a red flag and should be addressed-but stopping medication abruptly can cause a rebound in ADHD symptoms, which may be worse than the side effects. Your doctor may adjust the dose, switch to a different medication, suggest a medication holiday, or add appetite support like cyproheptadine in rare cases.
Are non-stimulant ADHD meds better for growth and appetite?
Yes, non-stimulants like atomoxetine (Strattera) have minimal impact on appetite and growth. But they’re less effective-working for about 60% of teens compared to 75% with stimulants. If growth or appetite is a major concern and ADHD symptoms are moderate, non-stimulants are a good option. For severe ADHD, stimulants still offer the best symptom control.
How often should my teen’s height and weight be checked?
At the start of treatment, then every 3 months during the first year. After that, every 6 months. If growth slows significantly, your doctor may check more often. Most pediatric offices now use digital growth charts to track changes precisely. If your teen’s height or weight drops below the 25th percentile for their age, it’s time to reassess the treatment plan.
Can ADHD medication affect puberty?
There’s no strong evidence that ADHD medications delay puberty. Some teens may gain weight more slowly or appear leaner due to reduced appetite, but this doesn’t mean their pubertal development is on hold. If you’re concerned about delayed puberty, your doctor can check hormone levels and bone age with a simple X-ray. Most teens on ADHD meds go through puberty normally.
What’s the difference between immediate-release and extended-release ADHD meds for growth?
Extended-release versions (like Concerta or Vyvanse) provide steady medication levels all day, which can lead to longer appetite suppression. Immediate-release versions (like Ritalin) wear off faster, often allowing appetite to return by afternoon. Some families find immediate-release easier to manage because they can time meals around dosing. However, extended-release reduces the need for midday dosing, which helps with school compliance.
Is it safe to take a break from ADHD meds during summer?
Yes, and many experts recommend it. A summer break-often called a “medication holiday”-can help teens catch up on growth and regain appetite. A 2013 study found that 87% of teens recovered 75% of their expected growth rate within six months of stopping. This works best for teens with stable symptoms and good routines. Always consult your doctor before pausing medication.
All Comments
Inna Borovik December 6, 2025
Let’s be real - this whole 'growth suppression' panic is overblown. The AAP data shows 89% catch up by 25. That’s not a crisis, it’s a delay. Parents treat ADHD meds like poison instead of tools. If your kid’s eating pizza at 9 p.m. and sleeping through the night, you’re winning.
Stop micromanaging calories. Start managing expectations.
Akash Takyar December 6, 2025
I appreciate the thoroughness of this post - truly. As a parent of a 15-year-old on Concerta, I can confirm that timing meals before the medication kicks in made all the difference. We now serve a protein-heavy breakfast at 6:30 a.m., and by 10 a.m., he’s not starving - he’s just not hungry. We’ve learned to respect the biology.
Also, the 3-month growth checks? Non-negotiable. Our pediatrician caught a dip in velocity early, and we switched to a lower dose. No drama. Just data.
Arjun Deva December 6, 2025
Of course they suppress growth - Big Pharma doesn’t want your kid to grow tall, they want him dependent on pills forever. The FDA? Controlled by the same people who sold you cigarettes in the ‘50s. Look at the studies - they’re funded by the manufacturers. Who do you think pays for the ‘89% catch up’ claim? The same labs that invented Vyvanse.
They’re lying. And you’re letting them.
Rashmi Gupta December 7, 2025
Wait - so you’re saying stimulants are fine because kids eat pizza at night? That’s not nutrition, that’s a sugar coma.
And you call this ‘smart use’? My cousin’s kid got a growth hormone referral because he lost 12% of his body weight in six months. You think that’s normal? It’s not. It’s negligence dressed up as ‘data’.
Andrew Frazier December 8, 2025
Why are we even talking about this? In America, we fix stuff. If the meds make your kid skinnier, give him a protein shake. If he’s not growing, give him a growth spurt pill. Problem solved.
Other countries cry about this. We just adapt. That’s why we lead the world.
Nava Jothy December 9, 2025
OMG I’m so glad someone finally said this!! 😭 My daughter was at the 90th percentile for weight at 12. Now she’s at the 10th. I cried every night for months. We switched to Strattera. She’s still a mess in class, but at least she’s not a ghost. And yes - I know it’s less effective… but what’s the point of focus if your kid looks like a walking skeleton? 💔
Doctors just say ‘it’s temporary.’ Temporary is 14 months of nightmares.
olive ashley December 10, 2025
Let me guess - you’re one of those parents who thinks ‘medication holidays’ are a magic fix. Newsflash: ADHD doesn’t take summer off. Your kid’s grades tank, they get suspended, you panic, you restart meds - and now they’re even more suppressed because their body’s confused. This isn’t a reset button. It’s a rollercoaster.
And the ‘89% catch up’ stat? That’s not comforting. It’s a lie wrapped in a p-value.
Ibrahim Yakubu December 11, 2025
You people think this is unique to America? In Nigeria, we don’t even have access to these drugs. Our children with ADHD are labeled lazy, beaten, thrown out of school. You’re arguing over 1.39 cm of growth? We’d kill for the chance to even see a pediatric psychiatrist.
Stop your first-world problems. Your kid is alive. That’s the win.
Dan Cole December 12, 2025
There is a metaphysical dimension here that transcends the biological. ADHD medication is not merely a pharmacological intervention - it is a symbolic rupture in the child’s ontological development. The suppression of appetite mirrors the suppression of the authentic self under the weight of neurotypical conformity.
When we force a child to eat at 6 a.m. to compensate for dopamine modulation, we are not nurturing - we are programming. The body becomes a machine. The soul? It retreats.
Perhaps the real question is not whether they grow taller - but whether they grow whole.
Max Manoles December 12, 2025
My 16-year-old’s been on Vyvanse for 2 years. He lost 15 pounds in the first 4 months. We did everything: breakfast before school, midnight snacks, calorie-dense smoothies, weekend breaks. He’s now back at his original weight and grew 2 inches last year.
The key? Consistency. And a doctor who actually listens. I wish I’d known about the growth chart tracking earlier - it’s not magic, it’s just math. Track it. Adjust it. Don’t panic.
Mayur Panchamia December 13, 2025
Let me tell you something - if your kid’s on ADHD meds and you’re not feeding him butter, eggs, and ghee every morning, you’re doing it wrong. This isn’t some hippie organic salad nonsense. This is India - we know how to fuel a growing boy. Ghee on toast. Paneer scramble. Milk with dates. That’s how you fight suppression.
Stop listening to American doctors. Our grandmas knew this before they invented Ritalin.
Karen Mitchell December 14, 2025
This entire post reads like an industry-funded op-ed. The AAP guidelines? Written by consultants with ties to pharmaceutical companies. The ‘89% catch up’ statistic? Extracted from a study with a 20% attrition rate. The ‘non-stimulants are less effective’ claim? Based on subjective teacher ratings.
There is no transparency. There is no independent oversight. And you, dear reader, are being manipulated into believing this is a safe, benign intervention.
I will not normalize this.
Geraldine Trainer-Cooper December 15, 2025
I just give my kid peanut butter sandwiches at 7 and let him eat nachos at 10. Works fine.