You clicked this because you want the clean, no-drama answer to how albendazole actually kills worms-and what that means in real use. Here’s the promise: a plain-language tour from molecule to clinic, with the practical bits you’ll actually use (food timing, tissue penetration, resistance signals). No fluff, and I’ll keep it relevant to how albendazole is used in 2025 according to major references (BNF 2025, WHO deworming guidance 2023, FDA/CDC labeling updates).
- TL;DR: Albendazole binds parasite beta-tubulin, blocks microtubules, halts glucose uptake, drains glycogen, and starves worms to death.
- Fatty food increases the active metabolite in blood several-fold-good for tissue infections; an empty stomach keeps more drug in the gut-good for luminal worms.
- It’s selective because parasite tubulin binds albendazole better than human tubulin; dose and duration shape safety.
- Resistance happens via beta-tubulin mutations and drug efflux; combinations and correct regimens help.
- Think ahead: long courses need liver checks; dying tissue parasites can inflame-steroids and careful monitoring reduce risk.
What Albendazole Does at the Molecular Level
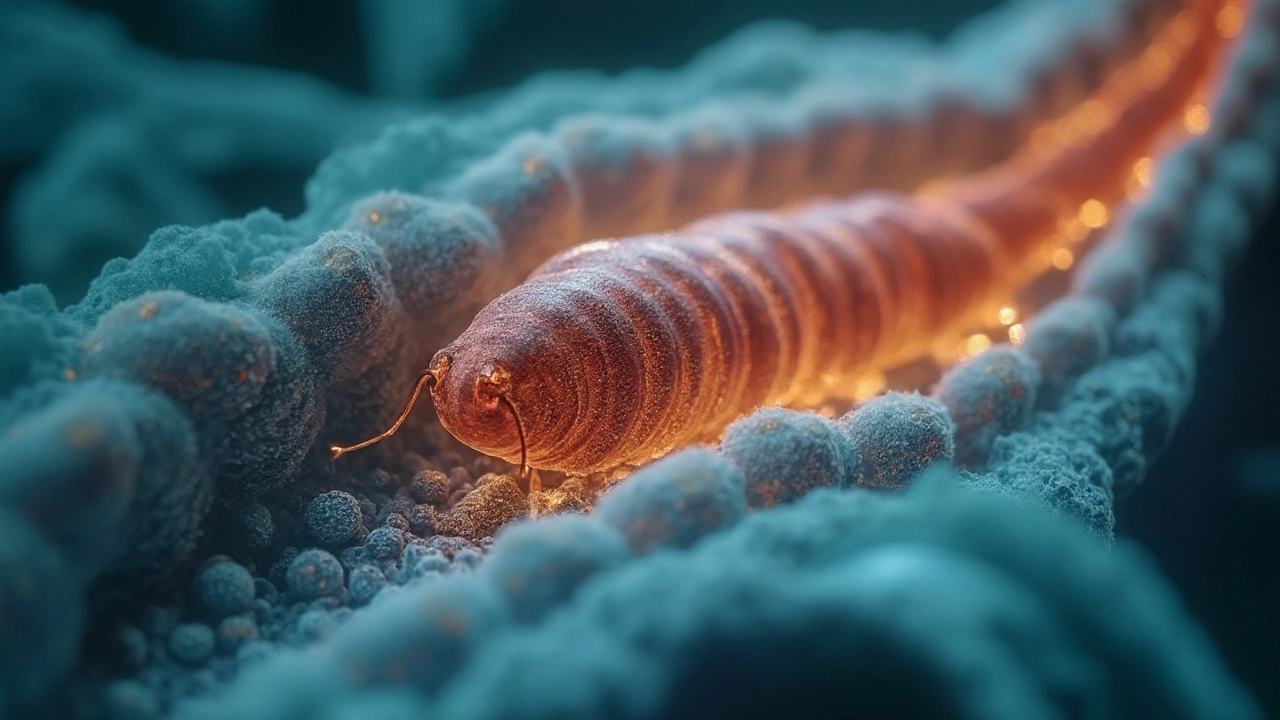
Albendazole is a benzimidazole anti-helminthic. Its target is not vague-it binds to beta-tubulin in parasites and prevents microtubules from forming. Microtubules are the cell’s scaffolding and conveyor belts. Without them, intestinal cells in worms can’t pull in glucose, can’t move nutrients around, and can’t divide properly. The parasite runs out of fuel and stalls.
Mechanistically, this plays out in a few steps:
- Binding: Albendazole (and its active sulfoxide metabolite) attaches to parasite beta-tubulin at the colchicine site. Affinity is higher for helminth isoforms than for human tubulin isoforms.
- Microtubule collapse: Polymerization fails. Think of a factory where all the conveyor belts fall apart.
- Energy failure: Glucose uptake drops, glycogen stores empty, and ATP (energy) production slides. Parasites become sluggish, then non-viable.
- Cell division stalls: Eggs and larvae struggle to mature; adults can’t maintain their gut lining (tegument in cestodes), so nutrient absorption craters.
- Death or expulsion: The worm dies in place or loses its grip and is cleared by gut motility and immune pressure.
That’s the core of the albendazole mechanism of action. Two more nuances matter:
- Secretory trafficking: Vesicles can’t travel without microtubules, so surface proteins and enzymes don’t reach the parasite’s exterior. Its protective coat suffers.
- Egg impact: Reduced egg production and viability help in public health by cutting transmission during mass drug administration (shown repeatedly in school-based deworming programs reported to WHO).
Scope of activity: Albendazole hits most intestinal nematodes (Ascaris, hookworm, whipworm, pinworm), tissue nematodes like Strongyloides with caveats, and many larval/tissue stages (neurocysticercosis, echinococcosis). It’s also active against some cestodes. Trematodes (flukes) are a poor fit-praziquantel or triclabendazole work better there.
From Swallow to Site: Absorption, Metabolism, and Where the Drug Goes
Albendazole is a prodrug. The tablet itself barely dissolves and is poorly absorbed. The magic happens after first-pass metabolism in the gut wall and liver, where it flips into albendazole sulfoxide-the active metabolite that circulates and reaches tissues.
Key pharmacokinetic points (summarized from FDA labeling, BNF 2025, and CDC materials):
- Food effect: A fatty meal can increase albendazole sulfoxide exposure by roughly 2-5 times. That’s a big lever.
- Tmax: Peak sulfoxide levels usually arrive 2-5 hours post-dose.
- Distribution: The sulfoxide is about 70% protein-bound and penetrates many tissues. It reaches cerebrospinal fluid and cyst fluid-often estimated at roughly 30-50% of plasma levels, which is why it works in neurocysticercosis and hydatid disease.
- Half-life: Albendazole sulfoxide hangs around about 8-12 hours, then becomes an inactive sulfone and other metabolites cleared by the liver.
- Variability: Enzyme inducers (like carbamazepine or phenytoin) can lower sulfoxide levels; cimetidine and dexamethasone can raise them. This matters most for long, tissue-targeted courses.
How to use this in real life:
- Gut-only infections (e.g., pinworm, Ascaris): Taking albendazole on an empty stomach can keep more drug in the gut lumen where the worms live, instead of pulling it into the bloodstream.
- Tissue infections (e.g., neurocysticercosis, echinococcosis): A fatty meal boosts blood levels and tissue penetration, which improves effect on cysts and larvae deep in organs.
Albendazole also accumulates in hydatid cysts to useful levels. That’s why it’s part of pre- and post-operative protocols around echinococcal surgery or percutaneous drainage in many centres cited in surgical infectious disease texts and echoed in WHO/PAHO materials.
Now, because tissue penetration is a double-edged sword, there’s one more principle: when parasites die in the brain or eye, inflammation can spike. Steroids and careful monitoring are not “nice to haves”-they’re standard good practice in neurocysticercosis pathways (CDC clinical guidance, neurology society statements).
| Use case | Main targets | Where the drug acts most | Food advice | Typical duration | Helpful co-therapy | Notes |
|---|---|---|---|---|---|---|
| Luminal soil-transmitted helminths (Ascaris, hookworm, whipworm) | Nematodes in the intestine | Intestinal lumen, parasite gut cells | Empty stomach | Single dose or short course (1-3 days depending on species) | Iron if anaemic from hookworm; hygiene | Reduces egg output; repeat dose may be used in some settings (WHO school programs). |
| Pinworm (Enterobius) | Perianal pruritus; household spread | Intestinal lumen | Empty stomach | Single dose with repeat in 2 weeks common locally | Treat close contacts; wash bedding; nail hygiene | Egg re-exposure is the norm; environmental control matters. |
| Neurocysticercosis (Taenia solium larvae) | Parenchymal brain cysts | Systemic-brain tissue/CSF | Fatty meal | Weeks, guided by imaging and response | Steroids; antiepileptics if seizures; consider proton pump inhibitor | Watch for inflammatory worsening when cysts die; specialist oversight essential. |
| Echinococcosis (hydatid disease) | Liver/lung cysts (Echinococcus) | Systemic-cyst fluid and wall | Fatty meal | Prolonged courses (months) or peri-procedural | Surgery or PAIR as indicated; monitor LFTs | Albendazole sterilizes cysts and lowers recurrence. |
| Toxocariasis / Visceral larva migrans | Migratory larvae | Systemic tissues | Fatty meal | Weeks | Steroids if heavy inflammatory load | Diagnosis often serology + eosinophilia; eye disease requires caution. |

Why Worms, Not You: Selectivity, Safety, and What to Watch
Why doesn’t albendazole wreck human cells? Selectivity. The drug prefers helminth beta-tubulin variants. Substitutions at positions like codon 200 (phenylalanine vs tyrosine in many resistant helminth strains) change binding. Human tubulin isoforms have lower affinity, so your microtubules are mostly left alone at therapeutic doses.
That said, systemic exposure is not zero-especially on long courses. Real-world safety notes pulled from BNF 2025, FDA labeling, and neurology/ID guidelines:
- Common: Mild GI upset, headache, transient ALT/AST rises, reversible hair thinning with extended courses.
- Less common but important: Bone marrow suppression (neutropenia), usually with long, high-dose therapy. That’s why blood counts matter over weeks.
- Inflammatory flares: When tissue parasites die (brain, eye, spinal cord), symptoms can worsen before they improve. Preempt with steroids when indicated.
- Pregnancy: Animal data show teratogenicity. Most authorities advise avoiding albendazole in the first trimester. WHO permits single-dose use after the first trimester in high-burden deworming campaigns when benefits outweigh risks. For individual care, clinicians weigh risks/benefits.
- Breastfeeding: Small amounts in milk; major references consider it compatible. Monitor the infant if the mother takes prolonged therapy.
- Contraception: For people who could become pregnant, avoid conception during therapy and for at least 1 month after the last dose (a common label recommendation).
Drug interactions to keep in mind:
- Enzyme inducers (carbamazepine, phenytoin, phenobarbital): Lower albendazole sulfoxide levels-tissue efficacy may suffer.
- Cimetidine and dexamethasone: Can increase sulfoxide levels-useful in some tissue protocols, but watch for side effects.
- Warfarin: INR can be affected when prolonged therapy alters hepatic metabolism; closer INR checks are sensible.
Monitoring rules of thumb for longer/tissue courses:
- Baseline and periodic liver enzymes (e.g., every 2-4 weeks on multi-month regimens).
- Full blood count at intervals when courses extend beyond a couple of weeks or when symptoms suggest marrow suppression.
- Symptom watch: New neurological symptoms during neurocysticercosis treatment need urgent review.
Resistance and Real-World Use: When Albendazole Struggles and What Helps
Albendazole resistance is well-documented in veterinary helminths and has warning signs in human programs, particularly where mass drug administration repeats over years. Mechanisms include:
- Beta-tubulin mutations: Codons 167, 198, and 200 are the classics. These reduce binding, so microtubules keep forming.
- Drug efflux pumps: Upregulated transporters lower intracellular drug levels.
- Metabolic tweaks: Changes that affect drug activation or deactivation.
What that means for practice in 2025:
- Programmatic rotation and combination therapy: In some regions, alternating benzimidazoles or combining with another class (like ivermectin in certain campaigns) helps slow resistance. WHO implementation reports describe these strategies in high-transmission zones.
- Individual therapy choices: Praziquantel beats albendazole for schistosomiasis and adult tapeworms in many cases. Ivermectin can outperform albendazole for strongyloidiasis. Mebendazole is a close cousin to albendazole for many luminal nematodes and is sometimes preferred in pregnancy after the first trimester.
- Adherence and dosing context: Under-dosing or taking the drug the wrong way (e.g., empty stomach for a tissue infection) can look like resistance when it’s really pharmacokinetics.
- Diagnostics matter: Persistent egg shedding could be reinfection, not resistance. Environmental control and retreatment schedules make a big difference for pinworm and Ascaris.
Combination examples (as reflected in CDC and specialty texts): Albendazole plus praziquantel can be used in certain neurocysticercosis patterns to cover different cyst stages. Dexamethasone co-therapy is common to blunt inflammation and, as a side note, can increase sulfoxide exposure.

The Practical Playbook: Rules of Thumb, Quick Checks, and FAQs
Use these to convert mechanism into decisions you can act on.
Rules of thumb (food, formulation, timing):
- Target in the gut? Empty stomach keeps drug in the lumen.
- Target in tissues? Fatty meal boosts blood levels for better penetration.
- Long course coming up? Plan baseline LFTs, FBC, pregnancy test if relevant, and a schedule for re-checks.
- New seizures or headache on therapy for neurocysticercosis? Think inflammation from dying cysts and escalate care quickly.
- Tablet tricks: Chewable tablets exist; crushing standard tablets is common when swallowing is hard-absorption differences are minimal compared with the food effect.
Decision mini-tree (simplified):
- If infection is limited to the intestine and the person is otherwise well → consider empty stomach dosing and short course; focus on household/environmental control to prevent reinfection.
- If larvae or cysts are in tissues (brain, liver, lung, eye) → ensure specialist input, use fatty meals, plan steroids and imaging follow-up, and monitor labs.
- If prior therapy failed → confirm species and exposure, check food/dose adherence, review interacting drugs (inducers), and consider alternative/combination therapy.
Cheat-sheet comparisons (mechanism angle):
- Albendazole: Beta-tubulin binding; microtubule collapse; energy starvation.
- Mebendazole: Same class and mechanism; often used similarly for luminal nematodes.
- Praziquantel: Increases calcium influx in trematodes/cestodes; causes paralysis and tegument damage-best for schistosomiasis and many tapeworms.
- Ivermectin: Glutamate-gated chloride channel agonist; causes paralysis-strongyloidiasis, onchocerciasis, ectoparasites.
Mini-FAQ
- Why do guidelines disagree about food? They don’t, really. They’re speaking to different targets. Empty stomach for gut bugs; fatty meal for tissues.
- How fast does albendazole work? Parasite paralysis and death begin within days, but symptom relief depends on species and burden. Tissue cysts can take weeks to months to shrink.
- Is one dose enough? For pinworm and Ascaris, often yes, with a repeat to catch hatchlings. For tissue infections, almost never-courses are longer and monitored.
- Can I take it in pregnancy? Avoid in the first trimester. After that, some programs use single-dose therapy when benefits are clear. Individual decisions belong with a clinician.
- What if liver tests rise? Mild, transient bumps are common. Stop and reassess if increases are significant or symptoms (e.g., jaundice) appear-especially on long courses.
- Does albendazole reach the brain? Yes-the active metabolite enters CSF and brain tissue, enough to treat neurocysticercosis. That’s why food and interactions matter.
Next steps and troubleshooting
- For clinicians starting long tissue regimens: Set up lab monitoring (LFTs, FBC) and diary dates up front. Review concomitant antiepileptics or rifamycins that lower exposure. Consider whether dexamethasone is needed on day one.
- For public health teams: Track egg reduction rates and cure rates across cycles. If numbers slide, check adherence, drug quality, and species mix before assuming resistance. Consider rotating or combining classes per WHO operational guidance.
- For patients in households passing pinworms around: Pair the dose with a two-week repeat, trim nails, wash bedding hot, and clean common touchpoints the same day as treatment.
- If therapy seems to fail: Verify the species. Hookworm and Trichuris can be more stubborn; some regimens extend duration or pair with another agent. Also, check if the dose was taken with or without food as intended.
- When you need higher exposure: If tissue disease is hard to reach (dense cysts, multiple brain lesions), confirm high-fat meals, review for enzyme inducers, and discuss whether adding praziquantel (select cases) makes sense.
Evidence anchors used to shape this playbook: BNF 2025 monograph on albendazole for UK practice; WHO deworming guideline (2023 update) for programmatic context; FDA-approved label and CDC clinical guidance (revised through 2024) for pharmacokinetics, safety, and co-therapy notes; neurology/infectious disease society statements for neurocysticercosis management. These sources agree on the central mechanism, food effects, and safety patterns described here.
All Comments
Jarid Drake September 16, 2025
Just took albendazole for hookworm last month - fatty meal, no regrets. Felt like a wizard summoning energy from my burrito.
Worms didn’t stand a chance.
KAVYA VIJAYAN September 17, 2025
What’s fascinating is how the beta-tubulin binding specificity isn’t just a molecular quirk - it’s evolutionary armor. Helminths evolved tubulin isoforms optimized for their parasitic niche, and albendazole exploits that vulnerability like a key in a lock designed by nature itself. Human tubulin? Too structurally conservative, too phylogenetically distant. The drug doesn’t discriminate by malice - it just binds better where the binding pocket is more permissive. That’s why resistance mutations at codon 200 (Phe→Tyr) are so insidious: they subtly reshape the binding cleft without crippling the parasite’s cytoskeleton. It’s a Darwinian arms race in microtubule form. And the food effect? Pure pharmacokinetic poetry. Fatty acids boost micelle solubilization of the prodrug, enhancing lymphatic uptake and bypassing first-pass metabolism. That’s why tissue infections demand buttered toast, not black coffee. This isn’t magic - it’s biochemistry with intent.
Roderick MacDonald September 18, 2025
Bro this is the most useful thing I’ve read all year. I’m a med student in rural Oregon and we get a ton of soil-transmitted helminths - I’ve been giving albendazole on empty stomach like a robot, not realizing I was underdosing for tissue stuff.
Now I’m telling everyone: butter first, then pill. Game changer.
Also, steroids for neurocysticercosis? YES. Saw a guy crash after treatment because no one warned him. This should be a textbook chapter.
Tariq Riaz September 20, 2025
Interesting that you mention resistance in human programs. But let’s be honest - most of the "resistance" is just poor adherence and mass administration without diagnostic confirmation. In India, we give albendazole to kids who don’t even have worms. Of course the efficacy looks like it’s dropping. It’s not the parasite evolving - it’s the program collapsing under its own weight.
Also, the food effect is real, but nobody in public health programs cares about dietary compliance. You can’t tell a child in a slum to eat fat before taking a pill. That’s not medicine - that’s privilege.
Terrie Doty September 21, 2025
I’ve been on a long albendazole course for toxocariasis and honestly, the fatigue and mild liver enzyme spike were scary at first. But reading this breakdown made me feel so much better - it’s not that my body’s failing, it’s just the drug doing its job. I didn’t realize the cysts were still alive and just slowly dying. The inflammation wasn’t a setback - it was a sign it was working.
Also, I started taking it with avocado toast and honestly? I feel more stable. No more random headaches. Small changes, big difference.
Thanks for writing this. It’s rare to get something this clear and kind.
Guy Knudsen September 22, 2025
Albendazole binds tubulin? Yeah right. Next you’ll tell me the moon landing wasn’t faked.
They’re just using this to sell pills. The real mechanism? The government wants us all docile. Parasites are just a distraction so you don’t ask why your water tastes like metal.
And fatty meals? That’s just Big Pharma’s way of making you buy more butter. You’re being manipulated.
Also, I’ve been taking it on an empty stomach for 3 years and still have worms. Coincidence? I think not.
George Ramos September 23, 2025
Albendazole doesn’t kill worms - it makes them *feel* dead while the CDC secretly harvests their DNA for bio-weapons.
That’s why they tell you to take it with fat - so the metabolite gets into your bloodstream and syncs with your neural implants.
And the "steroids"? That’s not to reduce inflammation - it’s to keep you calm while they monitor your cytokine spikes.
They’ve been doing this since the 90s. Look up Project HelminthControl. You think WHO gives a damn about your liver enzymes? They’re tracking your immune response.
And don’t even get me started on the "food effect" - that’s just a cover for the fact that the drug only works if you’re eating GMO avocadoes from California.
Wake up. The worms are the least of your problems.
Chantel Totten September 23, 2025
Thank you for writing this with such care. I’m a nurse who’s given this drug to dozens of patients, and I’ve always felt uneasy about the lack of clear guidance on food timing - especially for elderly patients with poor appetites. This makes it so much easier to explain.
Also, the note about breastfeeding being compatible? That’s huge. I had a new mom panic last week because she was told to stop nursing. She didn’t know it was safe. This changes lives.
I’m printing this out for our clinic. No fluff, just truth. Exactly what we need.