Not all beta-blockers are the same. If you’ve been prescribed one, you might assume they all work the same way-lower heart rate, reduce blood pressure, protect the heart. But that’s not true. The difference between propranolol and nebivolol isn’t just the brand name or price. It’s the way they act in your body, what side effects you might get, and whether they’ll help or hurt you based on your other health conditions.
How Beta-Blockers Actually Work
Beta-blockers stop adrenaline and noradrenaline from binding to beta receptors in your heart and blood vessels. These are the chemicals that make your heart race during stress, exercise, or panic. By blocking them, beta-blockers slow your heart rate, reduce how hard your heart pumps, and lower blood pressure. That’s why they’re used after a heart attack, for heart failure, irregular heartbeats, and sometimes migraines or tremors.
But here’s the catch: your body has three types of beta receptors-beta-1, beta-2, and beta-3. Beta-1 receptors are mostly in the heart. Beta-2 are in your lungs, blood vessels, and muscles. Beta-3 are in fat tissue and blood vessel walls. Different beta-blockers target these differently. That’s where the real differences begin.
First-Generation: Nonselective and Broad Effects
Propranolol was the first beta-blocker ever made, back in the 1960s. It’s still used today, but it’s not the go-to anymore. Why? Because it blocks all beta receptors-beta-1, beta-2, even beta-3. That means while it helps your heart, it also tightens your airways. For someone with asthma or COPD, this can trigger serious breathing problems. Up to 30% of people with lung disease who take propranolol report worsened symptoms.
It also affects your metabolism. Beta-2 blockade can mask low blood sugar symptoms in diabetics-like a fast heartbeat or shaking-making hypoglycemia harder to spot. And because it crosses the blood-brain barrier, it’s more likely to cause fatigue, depression, or sleep issues. Patient reviews on Drugs.com show 38% of people on propranolol report moderate to severe side effects, including 27% with sleep problems and 19% with depression.
Second-Generation: Heart-Only Focus
Doctors started looking for something better. Enter atenolol, metoprolol, bisoprolol-these are cardioselective. That means they mainly block beta-1 receptors in the heart, leaving beta-2 receptors in the lungs mostly alone. That’s a big deal for people with asthma or diabetes. You’re still at some risk, but it’s much lower.
Metoprolol comes in two forms: tartrate (short-acting, taken twice daily) and succinate (long-acting, once daily). The succinate version is preferred for heart failure because it gives steady blood levels. But even with selectivity, side effects don’t disappear. Fatigue hits 42% of users, and cold hands or feet affect nearly a third. That’s because beta-blockers reduce blood flow to the skin and limbs.
Still, these drugs are safer. In a Cleveland Clinic survey, heart failure patients on bisoprolol or metoprolol succinate had 85% better adherence than those on propranolol. Why? Fewer breathing issues, less brain fog.
Third-Generation: The Game Changers
Carvedilol and nebivolol aren’t just beta-blockers-they’re multitaskers. Carvedilol blocks beta-1 receptors and alpha-1 receptors. Alpha-1 blockade relaxes blood vessels, lowering blood pressure even more. In the US Carvedilol Heart Failure Study (1996), carvedilol cut death risk by 35% compared to placebo. That’s why it’s a top choice for heart failure with reduced pumping ability.
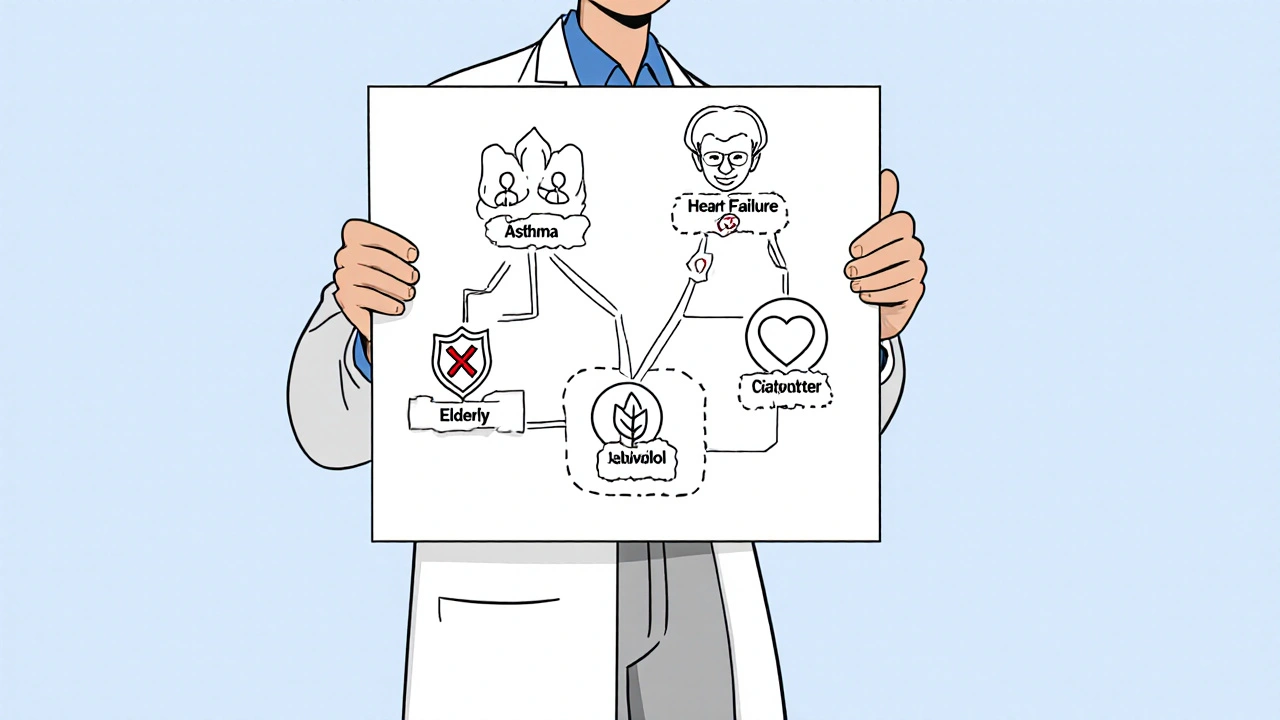
Nebivolol works differently. It blocks beta-1 receptors but also triggers the release of nitric oxide-a natural blood vessel relaxant. This means it lowers blood pressure without making you feel sluggish. It’s also linked to better sexual function in men over 50. On Reddit’s r/Cardiology, 65% of users reported improved erectile function on nebivolol versus only 35% on older beta-blockers.
And it’s not just about blood pressure. Nebivolol has antioxidant effects. Studies show it reduces oxidative stress in heart tissue by 30-40%. That helps prevent scarring and stiffening of the heart muscle. The SENIORS trial found nebivolol lowered cardiovascular death by 14% in elderly heart failure patients.
Why Dosing and Titration Matter
You can’t just start a beta-blocker at the full dose. These drugs need to be started low and increased slowly. Why? Because your body adapts. Jumping to a high dose can cause low blood pressure, dizziness, or even heart failure worsening.
Carvedilol requires 8 to 16 weeks to reach the target dose of 25 mg twice daily. Bisoprolol can be ramped up faster-4 to 8 weeks. If you’re on metoprolol tartrate, you’re taking it twice a day. If you’re on metoprolol succinate, it’s once. Mixing them up can lead to under- or over-treatment.
The FDA warns that stopping beta-blockers suddenly can spike your risk of heart attack by 300% in the first two days. That’s why you never quit cold turkey. Always taper under medical supervision.

Drug Interactions and Real-World Risks
Beta-blockers don’t play well with everything. If you’re on an inhaler like albuterol for asthma, nonselective beta-blockers like propranolol can make it useless. The EMA says this combo reduces bronchodilator effectiveness by 40-50%. That’s dangerous.
They also interact with calcium channel blockers like verapamil or diltiazem. Together, they can slow your heart too much, leading to fainting or heart block. And if you have kidney disease, some beta-blockers like atenolol need dose adjustments because they’re cleared by the kidneys. Carvedilol and nebivolol are mostly broken down by the liver, so they’re safer in kidney failure.
And don’t forget about other meds. Beta-blockers can mask symptoms of low blood sugar. If you’re diabetic and take insulin or sulfonylureas, you need to check your glucose more often.
Who Gets Which Drug? The Real Decision Tree
There’s no one-size-fits-all. Here’s how doctors pick:
- Heart failure with reduced ejection fraction? Carvedilol, bisoprolol, metoprolol succinate, or nebivolol. Avoid propranolol.
- Asthma or COPD? Stick to cardioselective agents (atenolol, bisoprolol, metoprolol). Still monitor closely.
- High blood pressure alone? Beta-blockers are no longer first-line. ACE inhibitors, ARBs, or calcium channel blockers work better at protecting your arteries. Beta-blockers are reserved if you also have heart disease or arrhythmias.
- Post-heart attack? Any cardioselective beta-blocker. Propranolol still works, but newer ones have better tolerability.
- Older adults over 80? Be cautious. 28% of prescriptions here are inappropriate per STOPP/START guidelines. Avoid high doses. Nebivolol or bisoprolol are often preferred for safety.
- Sexual side effects? Nebivolol is the only beta-blocker with evidence of improving erectile function.
The Bottom Line
Beta-blockers are powerful, but they’re not interchangeable. Choosing the right one depends on your heart condition, lung health, diabetes status, age, and even your sex life. Propranolol might be cheap, but it’s not always the best. Carvedilol and nebivolol cost more, but they offer real benefits-less fatigue, better heart remodeling, fewer breathing issues.
And while their use in simple high blood pressure has declined, they remain essential for heart failure, post-heart attack care, and certain arrhythmias. The key isn’t just taking a beta-blocker-it’s taking the right one for you.
Are all beta-blockers the same?
No. Beta-blockers differ in selectivity, how they’re cleared from the body, and additional effects. First-generation drugs like propranolol block all beta receptors and can cause breathing problems. Second-generation drugs like metoprolol target mainly the heart. Third-generation drugs like carvedilol and nebivolol also relax blood vessels, offering extra benefits for heart failure and fewer side effects.
Which beta-blocker is safest for someone with asthma?
Cardioselective beta-blockers like bisoprolol, metoprolol succinate, or atenolol are safer because they mainly affect the heart and have less impact on the lungs. But even these aren’t risk-free. Doctors still monitor closely, and the lowest effective dose is used. Never use nonselective beta-blockers like propranolol if you have asthma.
Why is carvedilol preferred for heart failure?
Carvedilol blocks both beta-1 and alpha-1 receptors, which reduces blood pressure and eases strain on the heart. It also has strong antioxidant properties that reduce heart tissue damage. Clinical trials show it lowers death risk by 35% in heart failure patients compared to placebo. It’s one of the few beta-blockers proven to improve survival in this group.
Can beta-blockers cause depression or fatigue?
Yes, especially older ones like propranolol that cross into the brain. Up to 19% of users report depression, and 42% feel unusually tired. Newer agents like nebivolol and bisoprolol are less likely to cause these effects because they don’t enter the brain as easily. If you’re feeling down or exhausted, talk to your doctor-switching drugs may help.
Is it safe to stop taking a beta-blocker suddenly?
No. Stopping abruptly can trigger a rebound effect-your heart rate and blood pressure can spike, increasing your risk of heart attack by up to 300% in the first 48 hours. Always taper off slowly under your doctor’s guidance, even if you feel fine.
Do beta-blockers affect sexual function?
Many older beta-blockers like propranolol and metoprolol are linked to erectile dysfunction. But nebivolol is different. It boosts nitric oxide, which improves blood flow-including to the penis. Studies show 65% of men over 50 on nebivolol report improved sexual function, compared to only 35% on other beta-blockers.
Why are beta-blockers no longer first-line for high blood pressure?
Studies show beta-blockers lower blood pressure less effectively than other drugs like ACE inhibitors or calcium channel blockers, especially in reducing central aortic pressure-the pressure that matters most for stroke and heart damage. They also don’t protect kidneys as well. So unless you have heart disease, diabetes, or a history of heart attack, other drugs are preferred for simple hypertension.
All Comments
Andy Louis-Charles November 24, 2025
Just wanted to say nebivolol changed my life. No more brain fog, no more cold hands, and honestly? My sex life improved too. I was on metoprolol for years and felt like a zombie. Switched last year and now I’m hiking again. 🌿💪
Akash Chopda November 25, 2025
Big Pharma wants you to think these drugs are different but they’re all just poison with fancy labels. They don’t care if you live or die as long as you keep buying. The real cure is fasting and sunlight. Propranolol is just a trap.
Sam Jepsen November 25, 2025
Hey everyone - if you’re on a beta-blocker and feeling off, don’t just suffer. Talk to your doc. There’s a better fit out there. I was on propranolol and thought fatigue was just aging. Turns out it was the drug. Switched to bisoprolol and I’m back to playing guitar at 11pm again. You got this 💪
Yvonne Franklin November 26, 2025
Nebivolol for erectile function? Surprised more people don’t know this. It’s the only beta-blocker that actually helps with blood flow without crushing energy. If you’re a guy over 50 and on a beta-blocker, ask about it. No shame.
Bartholemy Tuite November 27, 2025
Look I’m Irish and we’ve got a thing for overmedicating but honestly this post is spot on. I was on propranolol for migraines and ended up in the ER with a panic attack because my blood sugar dropped and I didn’t feel it. My GP didn’t even mention the diabetes risk. Took me 3 years to figure it out. Now I’m on nebivolol and I can actually eat a sandwich without worrying I’m gonna pass out. Also I don’t feel like I’m walking through molasses anymore. The docs need to stop treating us like lab rats.
Neoma Geoghegan November 28, 2025
Cardioselective = game changer. Avoid propranolol if you have any lung history. Even if you think you’re fine. It’s not worth the risk. Nebivolol’s NO boost is legit science not marketing. Ask for it.
Victoria Stanley November 28, 2025
Thank you for writing this. So many people get handed a script and never question it. I’m a nurse and I’ve seen too many older patients on propranolol with COPD - it’s heartbreaking. Please, if you’re reading this and have lung issues, talk to your doctor about alternatives. You deserve to breathe easy.
steven patiño palacio November 28, 2025
Correction: The SENIORS trial showed a 14% reduction in cardiovascular death with nebivolol, but it was statistically significant only in patients aged 70+ with heart failure. Not all elderly populations. Precision matters. Also, carvedilol’s alpha blockade reduces afterload - that’s why it outperforms in systolic HF. Not just antioxidants.
stephanie Hill November 29, 2025
They don’t want you to know that beta-blockers were originally developed as pesticides. Now they’re in your water, your food, your pills. The FDA is in bed with the pharmas. You think nebivolol is better? It’s just the next flavor of poison. Watch the documentary ‘The Heart Pill Scam’ - it’s eye-opening.
Jeff Hicken November 30, 2025
bro why are we even taking these? just do yoga and drink celery juice