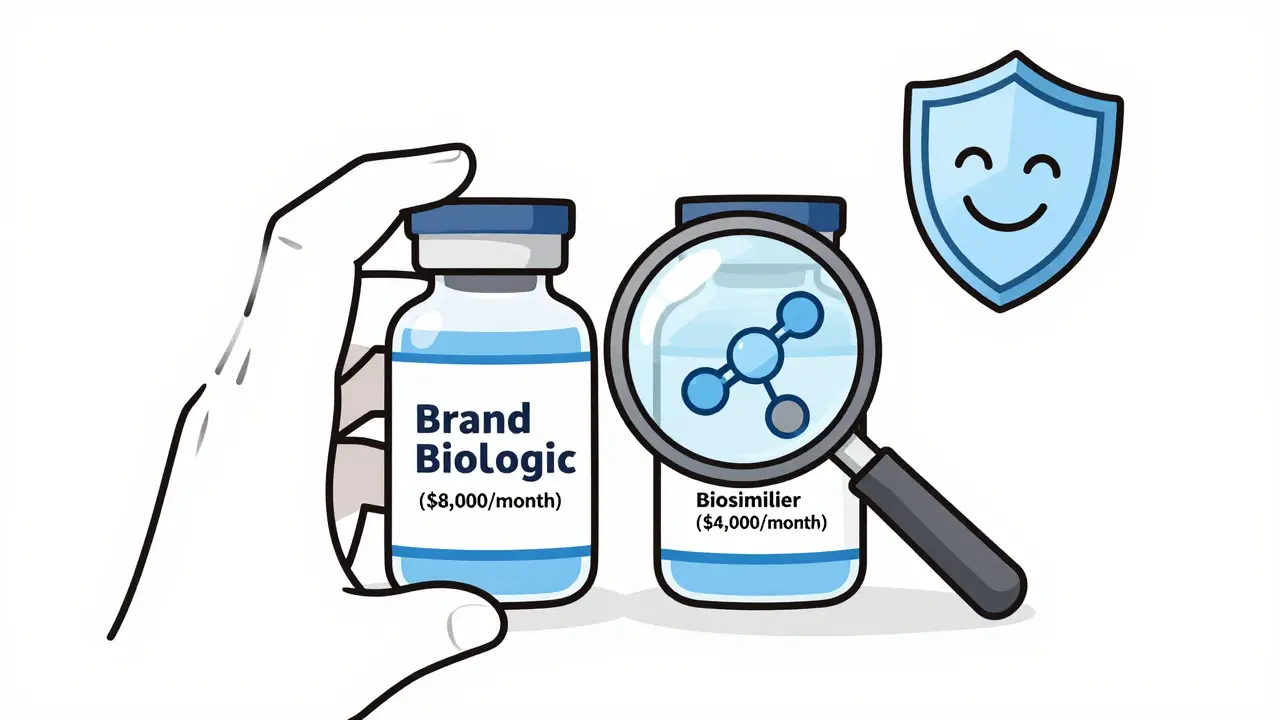
When a patient needs a biologic drug for rheumatoid arthritis, cancer, or diabetes, they often face a monthly cost of $5,000 to $8,000. These drugs are life-changing but financially crushing. Enter biosimilars - not generics, not copies, but highly similar alternatives that can cut those costs by 50% or more. The FDA’s approval process for these drugs has changed dramatically since October 2025, and the shift is finally making biosimilars a realistic option for millions of Americans.
Why Biosimilars Aren’t Like Generics
Most people think of generics as simple copies of brand-name pills. Take aspirin: one tablet has the exact same chemical structure as another. But biologics aren’t made in a chemistry lab. They’re grown in living cells - yeast, bacteria, or mammalian cells - and are made of complex proteins, sugars, and structures that can vary slightly even between batches from the same manufacturer. That’s why you can’t just swap one biologic for another like you would with a generic. A biosimilar isn’t identical to its reference product, but it’s close enough that no clinically meaningful differences exist in safety, purity, or potency. Think of it like two handmade wooden chairs from the same craftsman. They look the same, feel the same, and hold the same weight. But if you zoom in with a microscope, you’ll see tiny differences in grain or finish. The FDA doesn’t require those differences to be erased - just proven to be harmless.The Old Way: A Long, Costly Hurdle
Before October 2025, getting a biosimilar approved meant jumping through hoops that made development nearly impossible for smaller companies. The FDA required full-scale clinical trials comparing the biosimilar directly to the original biologic - not just to check if it worked, but to prove it worked exactly the same. These trials took 2-3 years and cost up to $300 million. Most of that time and money went into testing efficacy in thousands of patients, even though the drug’s structure had already been proven nearly identical through lab tests. That’s why, despite 76 biosimilars being approved by the end of 2025, only 23% of the U.S. market used them. In Europe, where the approval process was simpler, biosimilars make up 67% of the market. The gap wasn’t because Americans didn’t trust them - it was because they were rarely offered.The 2025 FDA Breakthrough
On October 29, 2025, the FDA released a new draft guidance that changed everything. It no longer requires comparative efficacy studies for most biosimilars. Instead, if a company can prove three things, they can skip the big clinical trials:- The biosimilar and reference product are made from the same type of cell line and are highly purified.
- The link between the drug’s physical properties and its clinical effect is well understood - like with adalimumab or trastuzumab.
- A pharmacokinetic (PK) study shows the drug behaves the same way in the body - how fast it’s absorbed, how long it lasts, how it’s cleared.
Interchangeability: The Big Confusion
Here’s where things get messy. Even if a biosimilar is approved, it doesn’t automatically mean a pharmacist can swap it for the brand-name drug without asking the doctor. That’s called interchangeability. Until recently, the FDA required separate “switching studies” - where patients alternated between the biosimilar and the original - to prove no harm was done. The October 2025 guidance scrapped that requirement. FDA Commissioner Marty Makary said at a conference: “Every biosimilar should have the designation of interchangeable.” He called interchangeability a “legislative term, not a scientific one.” In other words: if a biosimilar is approved, it’s safe to swap. But here’s the catch: the law still says interchangeability must be formally designated. So while the FDA now says it’s unnecessary, they’re still reviewing applications for interchangeability - and they’ve already approved two denosumab biosimilars with that status in October 2025. The disconnect between science and regulation is real. Some doctors are confused. Pharmacists are stuck between state laws and federal guidance. And patients? They’re just hoping their insurance covers the cheaper option.Who’s Winning - and Who’s Struggling
Big companies like Sandoz, Pfizer, and Amgen have the resources to handle the complex analytical testing. Together, they’ve brought 39 biosimilars to market. But smaller firms? It’s harder. Only 12 of the 76 approved biosimilars came from companies with fewer than 100 employees. Why? Because setting up a lab that can analyze 200+ quality attributes - from sugar chains to protein folding - costs millions upfront. The FDA’s new guidance helps, but it doesn’t fix the infrastructure gap. Still, momentum is building. Viatris and Biocon are stepping up. And new players are entering. The market is projected to grow from $18.7 billion in 2024 to $62.3 billion by 2029. Hospitals are already feeling the impact. Mayo Clinic saved $18 million in one year by switching oncology patients to biosimilars. That’s a 37% drop in drug costs.
Real Patient Experiences
Patients aren’t just numbers. On Reddit, a thread titled “Switched to biosimilar for rheumatoid arthritis - experiences?” had 87 responses. Sixty-three percent said their symptoms stayed the same. Twenty-two percent noticed minor changes - mostly at the injection site, like redness or stinging. One user wrote: “I had a flare-up after switching. My rheumatologist said it was stress, not the drug. We switched back. I’m fine now.” A September 2025 survey by the Arthritis Foundation found 78% of users were satisfied. But 41% were scared at first. Once they talked to their doctor, 68% felt better. That’s the real barrier: fear, not science.What’s Next?
The FDA’s draft guidance is open for public comment until January 27, 2026. Final rules are expected by June 2026. Analysts predict approvals will jump from 8-10 per year to 15-20. McKinsey forecasts biosimilars could capture 40-50% of the market by 2030 - up from 23% today. But roadblocks remain. Patent lawsuits have delayed 68% of approved biosimilars, according to the FTC. And some states still block pharmacists from substituting biosimilars without a doctor’s okay - even when the FDA says it’s safe. The law hasn’t caught up to the science.Bottom Line
The FDA’s 2025 update is the biggest step forward for biosimilars since Congress created the pathway in 2010. It’s faster, cheaper, and smarter. It doesn’t lower safety standards - it just uses better tools to meet them. The science is clear: if a biosimilar matches the original in structure and behavior, it’s safe to use. The next challenge isn’t regulatory - it’s cultural. Patients need to know biosimilars work. Doctors need to trust them. Pharmacies need clear rules. And lawmakers need to fix the laws that still treat biosimilars like second-class drugs.One thing’s certain: the $250 billion in potential savings over the next decade won’t happen unless we stop treating biosimilars like a compromise - and start treating them like the breakthrough they are.
How is a biosimilar different from a generic drug?
Generics are exact chemical copies of small-molecule drugs like aspirin or metformin. Biosimilars are highly similar to complex biologic drugs made from living cells - like antibodies or proteins. They can’t be identical because of their size and structure, but they must have no clinically meaningful differences in safety or effectiveness. The approval process for biosimilars is far more complex than for generics.
What did the FDA change in its biosimilar approval process in 2025?
In October 2025, the FDA updated its guidance to no longer routinely require comparative clinical efficacy studies for biosimilar approval. Instead, companies can rely on advanced analytical testing, pharmacokinetic (PK) studies, and immunogenicity data if the reference product is well-characterized and the biosimilar matches it closely. This cuts development time from 8-10 years to 5-7 years and reduces costs from $100-300 million to $50-150 million.
What is interchangeability, and why does it matter?
Interchangeability means a pharmacist can swap a biosimilar for the brand-name drug without asking the prescriber - just like switching between generic pills. The FDA now says all approved biosimilars should qualify as interchangeable, but the law still requires separate applications and proof. This creates confusion. Some states block substitution, even when the FDA approves interchangeability. The October 2025 approvals of two denosumab biosimilars with interchangeability status mark a turning point.
Why aren’t more biosimilars available in the U.S. compared to Europe?
Europe’s EMA has approved over 100 biosimilars since 2006 because its process is simpler - often requiring just one PK study. The FDA previously demanded full clinical trials proving efficacy, which delayed entry. Even after the 2025 changes, patent lawsuits and restrictive state laws still block access. Today, biosimilars make up only 23% of the U.S. market for eligible drugs, versus 67% in Europe.
Do biosimilars really save money?
Yes. Hospitals like Mayo Clinic reported a 37% drop in biologic drug costs after switching to biosimilars, saving $18 million annually. The FDA estimates biosimilars could save the U.S. healthcare system $250 billion over the next decade. A single biosimilar for a biologic that costs $80,000 per year can cost $40,000 or less. That’s tens of thousands in savings per patient.
Are biosimilars safe for long-term use?
Data from 76 approved biosimilars and real-world use show no safety concerns different from the reference products. Long-term studies on drugs like adalimumab biosimilars show consistent outcomes over 5+ years. The FDA’s updated guidance focuses on analytical similarity, which modern tools now predict with high accuracy. Critics warn about subtle differences, but no verified safety issue has emerged from over a decade of global use.
All Comments
Josiah Demara February 14, 2026
Let's cut through the corporate BS. The FDA didn't 'change' anything - they were forced into it by pressure from hospitals and patients screaming over $80k/year drugs. The real story? Big Pharma spent $200 million lobbying to keep biosimilars locked out. Now that the science is undeniable, they're scrambling to rebrand their patents as 'innovation.' This isn't progress - it's damage control. And don't get me started on 'interchangeability.' That's a legal loophole dressed up as safety. If it works in the lab, it works in the body. End of story.
Kaye Alcaraz February 15, 2026
The progress here is real and deeply meaningful. For patients living with chronic conditions, the difference between $8,000 and $4,000 a month isn't a statistic - it's the ability to keep their job, care for their children, or simply sleep through the night without anxiety. The FDA's updated guidance reflects decades of accumulated evidence, not political expediency. This is science meeting compassion. Let's not confuse bureaucratic nuance with failure. Many lives are being saved, quietly and steadily, because of this shift.
Charlotte Dacre February 15, 2026
Oh look, the FDA finally remembered that humans exist. Took them long enough. Meanwhile, in Europe, biosimilars have been saving lives and money since before most Americans knew what a biologic was. We're not talking about some futuristic dream - we're talking about a system that's been working for 15 years. The U.S. didn't 'innovate' - it finally caught up. And still, some states won't let pharmacists swap them. What is this, 1998?
Esha Pathak February 17, 2026
There is a deeper truth here, beyond patents and PK studies. The human body is not a machine. It is a symphony of energy, vibration, and unseen connections. When we reduce life to measurable attributes - sugar chains, protein folding - we forget that healing is not merely chemical. The biosimilar may match the molecule, but does it match the soul? Perhaps the real barrier is not regulation, but our fear of trusting something that is 'similar' rather than 'identical.' In Indian philosophy, we say: 'The form is illusion. The essence is truth.' The essence here is healing. And that, my friends, cannot be patented.
Kapil Verma February 19, 2026
America is finally waking up while the rest of the world has been moving forward. India and China have been manufacturing high-quality biosimilars for years. Why? Because we don't worship patents like religion. We care about people. You think this $250 billion savings is some American miracle? No. It's because global manufacturers - not just Pfizer and Amgen - have been doing this right. The FDA is playing catch-up. And if you think this is about science, you're blind. This is about who gets rich and who gets treated. We need to stop acting like the U.S. is the center of medical innovation. We're not. We're the last to the party.
Betty Kirby February 21, 2026
Let’s be honest: if this were a generic pill, no one would blink. But because it’s a ‘biologic,’ suddenly we need 200 analytical tests, three clinical trials, and a PhD in biochemistry to understand it. The fear-mongering around biosimilars is absurd. Patients are being told to fear what’s cheaper - as if saving money makes it less effective. This isn’t science. This is marketing. And the real villain? The insurance companies who still refuse to cover biosimilars unless you jump through 17 hoops. The FDA did their job. Now it’s time for payers to stop playing games.
Erica Banatao Darilag February 22, 2026
i just switched to a biosimilar last month and i wanted to say thank you to everyone who worked on this. i have ra and was paying $7200 a month. now it’s $3400. i didn’t even know i could switch. my dr didn’t mention it. my pharmacy didn’t tell me. i found out by accident. i’m so glad it worked. my symptoms are the same. no redness. no stinging. just… relief. thank you. really. this matters.
Chiruvella Pardha Krishna February 23, 2026
The question is not whether biosimilars work. The question is whether we have the moral courage to accept them. We live in a culture that equates cost with value, and complexity with superiority. A $40,000 drug is not more 'real' than a $20,000 one. The same protein. The same mechanism. The same outcome. We have the tools to see this clearly. But we refuse. Because to accept a biosimilar is to accept that profit, not patient care, has dictated medical policy for decades. And that truth is harder to swallow than any drug.