When you’ve been living with chronic pain for months or years, you’ll try almost anything to feel better. That’s why so many people turn to cannabinoids-CBD oil, THC gummies, cannabis tinctures-hoping for relief without the risks of opioids. But here’s the hard truth: cannabinoids for pain aren’t a miracle cure. And the science? It’s messy, conflicting, and often misleading.
What Exactly Are Cannabinoids?
Cannabinoids are chemicals found in the cannabis plant. The two most talked-about are THC (tetrahydrocannabinol) and CBD (cannabidiol). But there are others-CBG, CBN, THCV-that are starting to show promise in labs. These compounds interact with your body’s endocannabinoid system, a network of receptors that helps regulate pain, mood, sleep, and inflammation. THC is the part that gets you high. CBD doesn’t. That’s why so many people assume CBD is safer. But safety doesn’t always mean effectiveness. And that’s where things get complicated.The Evidence Is Split-Here’s Why
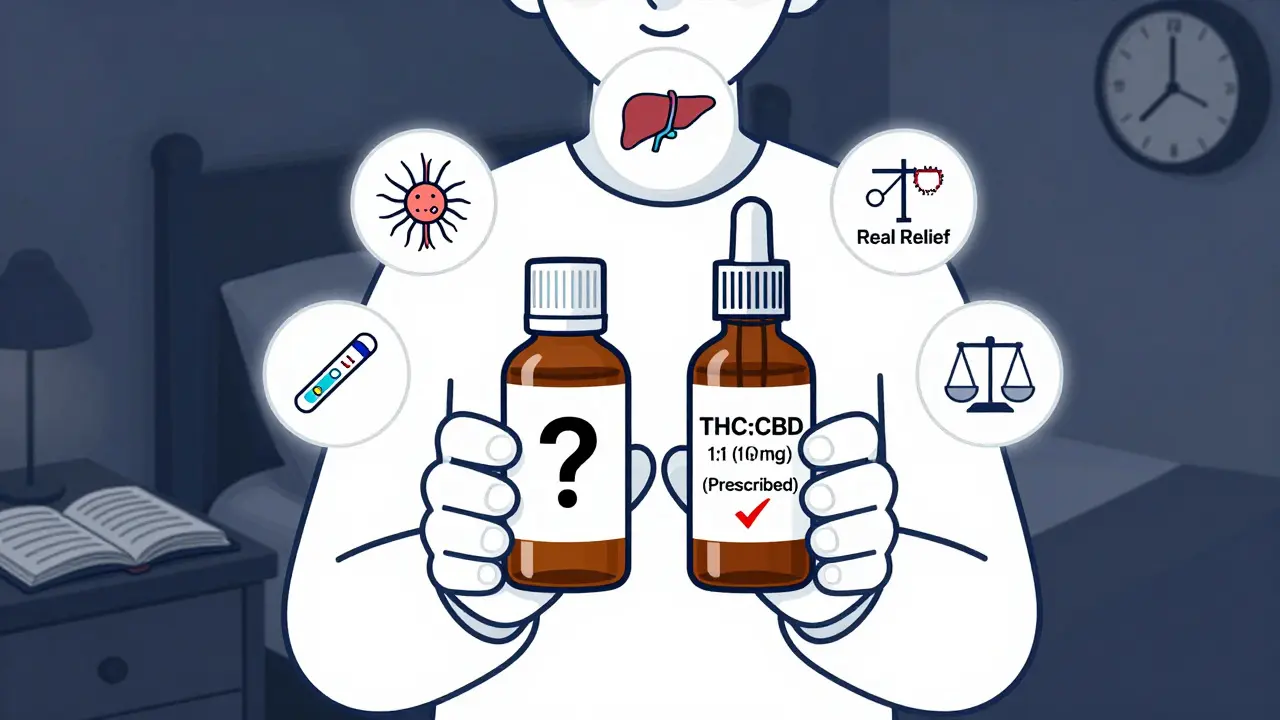
You’ve probably seen headlines claiming CBD cures pain. But look closer. A major 2023 study from the University of Bath analyzed 16 high-quality trials using pharmaceutical-grade CBD. Fifteen of them found CBD performed no better than a placebo for pain relief. That’s not a fluke. It’s a pattern. Meanwhile, a 2015 JAMA review found moderate-quality evidence that cannabinoids (including THC) can help with chronic pain-especially neuropathic pain, the kind caused by nerve damage. The CDC backs this up, saying there’s limited evidence for most pain types, but some benefit for nerve-related pain. So why the contradiction? Because not all cannabinoids are the same. CBD alone? Weak evidence. THC combined with CBD? Stronger. A 1:1 ratio of THC:CBD, like in the drug Sativex, is approved in Canada for multiple sclerosis pain and cancer pain that opioids can’t touch. Patients using it often report cutting their opioid doses by 70% or more. And then there’s CBG-cannabigerol. A January 2025 study from Yale found CBG reduced pain signals in nerve cells more effectively than CBD or CBN. It didn’t cause intoxication. It didn’t show liver toxicity in early tests. It’s not available in stores yet. But if it makes it through clinical trials, it could be the first truly promising non-psychoactive cannabinoid for pain.What About CBD Products You Can Buy Online?
This is where things get dangerous. A University of Bath lab tested 125 popular CBD oils and gummies sold in the U.S. and U.K. They found 43% contained less CBD than labeled-some had none at all. 22% had more than advertised. And 1 in 5 contained illegal levels of THC. That means you could be getting high without knowing it. Or worse-you could be ingesting pesticides, heavy metals, or synthetic cannabinoids that aren’t even listed on the label. Amazon reviews tell the same story. One user tried a popular CBD oil for arthritis for six weeks. No difference. Then they switched to a placebo oil. Still no difference. Another person spent $400 on CBD gummies for back pain. Zero relief. A third reported a 30% drop in fibromyalgia pain after two weeks. But that’s the exception, not the rule. Trustpilot analyzed over 14,500 reviews of top CBD brands. The average rating? 3.2 out of 5. Why the low score? The biggest complaint: “No pain relief.” Forty-one percent of negative reviews said exactly that. People are spending hundreds of dollars a month on something that, for most, doesn’t work.
Dosing: No Rules, Just Guesswork
There are no official dosing guidelines for cannabinoids and pain. Why? Because the FDA hasn’t approved any for that use-except for rare epilepsy drugs. That means doctors have to wing it. Most pain clinics suggest starting low: 2.5 to 5 mg of THC, or 10 to 20 mg of CBD. Wait at least two hours before taking more. Increase slowly over days or weeks. Track your pain on a scale of 1 to 10. Keep a journal. But here’s the catch: your body’s response depends on your weight, metabolism, liver function, and what other medications you take. CBD can interfere with blood thinners, antidepressants, and seizure meds. THC can raise your heart rate or make anxiety worse. And high doses of CBD have been linked to liver enzyme changes in rare cases. If you’re switching from opioids, don’t quit cold turkey. Talk to your doctor. Withdrawal from opioids can be brutal. Cannabinoids won’t stop withdrawal symptoms-they might just help manage the pain while you taper.Safety: What You’re Not Being Told
Cannabinoids aren’t risk-free. The JAMA review found people using cannabinoids were more likely to feel dizzy, have dry mouth, or feel nauseous. THC can cause paranoia, memory issues, or impaired coordination. Long-term use might affect brain development in people under 25. And the biggest hidden risk? Contamination. The CBD market is a Wild West. No federal oversight. No standard testing. You’re trusting a company that doesn’t have to prove what’s in the bottle. Even if it says “0% THC,” it might not be true. A positive drug test could cost you your job. Or your custody rights. That’s why medical programs in Canada and the Netherlands are more trusted. They grow cannabis under controlled conditions, test every batch, and dispense it through pharmacies. You know what you’re getting. In the U.S.? You’re gambling.
Who Might Actually Benefit?
Not everyone. But some people do get real relief. - People with neuropathic pain (diabetic nerve pain, post-shingles pain, MS-related pain) are most likely to see benefit, especially with THC:CBD combinations. - Those who can’t tolerate opioids due to side effects or addiction risk. - Patients who’ve tried physical therapy, NSAIDs, and antidepressants with no success. But if you have back pain from a herniated disc? Arthritis? Migraines? The evidence is thin. You’re better off with proven options: exercise, physical therapy, cognitive behavioral therapy, or low-dose antidepressants like amitriptyline.The Future: What’s Coming Next
The FDA is reviewing whether to reschedule cannabis from Schedule I (no medical use, high abuse risk) to a lower category. That could unlock federal funding for research. Right now, there are over a dozen Phase III trials running-testing CBD for chronic low back pain, THC:CBD for cancer pain, CBG for inflammatory pain. If one of these gets approved by 2027, we’ll finally have a standardized, lab-tested cannabinoid medicine for pain. No more guessing. No more contaminated products. Just a pill or spray with a known dose and proven effect. Until then, treat cannabinoids like a supplement-not a medication. Don’t expect miracles. Don’t spend your life savings on hope. And if you do try it, start low, go slow, and talk to your doctor.What to Do If You’re Considering Cannabinoids
1. Don’t replace proven treatments. Use cannabinoids only as an add-on, not a substitute. 2. Choose medical-grade products. If you’re in a state with legal medical cannabis, get it from a licensed dispensary. Avoid online CBD sellers. 3. Start with low doses. 5 mg THC or 10 mg CBD. Wait 2 hours. Repeat only if needed. 4. Track your pain. Use a simple app or notebook. Rate pain daily. Note sleep, mood, side effects. 5. Talk to your doctor. Especially if you take other meds. Tell them exactly what you’re using. 6. Be skeptical of claims. If it says “cures arthritis” or “eliminates pain,” it’s a scam. 7. Watch for red flags. Products that don’t list ingredients, third-party lab results, or manufacturing details? Avoid them.Chronic pain is exhausting. It steals sleep, relationships, and joy. It’s natural to want a solution. But not all solutions are real. Right now, the only cannabinoid with solid evidence for pain is a 1:1 THC:CBD combo-prescribed, regulated, tested. Everything else? It’s still experimental. And the market is full of people who profit from your desperation.
Be smart. Be patient. And don’t let hope replace science.
Can CBD oil really help with chronic pain?
The evidence for CBD alone is weak. Most high-quality studies show it doesn’t work better than a placebo for chronic pain. Some people report mild relief, but it’s inconsistent. If you’re looking for real pain control, CBD oil is unlikely to deliver.
Is THC better than CBD for pain?
Yes, for most types of chronic pain-especially nerve pain. THC has stronger pain-blocking effects than CBD. A combination of THC and CBD (like Sativex) is proven to help with multiple sclerosis and cancer pain. But THC can cause dizziness, anxiety, or impaired thinking, so it’s not for everyone.
Can I use cannabinoids instead of opioids?
Some patients reduce their opioid use when adding a THC:CBD product, but you shouldn’t switch without medical supervision. Opioid withdrawal can be dangerous. Cannabinoids may help manage pain during tapering, but they’re not a direct replacement. Always work with your doctor.
Are over-the-counter CBD products safe?
Many are not. Testing has shown that up to 43% of products contain less CBD than labeled, and 1 in 5 contain illegal amounts of THC. Some have pesticides, heavy metals, or synthetic chemicals. There’s no federal oversight, so you’re taking a risk with every bottle.
What’s the best way to take cannabinoids for pain?
Tinctures (under the tongue) and capsules offer the most consistent dosing. Smoking or vaping can irritate lungs and deliver unpredictable doses. Topicals (creams, patches) may help localized pain but don’t affect deep or nerve pain. Start with low doses and increase slowly.
Can cannabinoids cause liver damage?
High doses of CBD (over 1,000 mg per day) have been linked to elevated liver enzymes in some studies, which can signal stress on the liver. This is rare but possible, especially if you already have liver issues or take other medications metabolized by the liver. Always get liver function checked if you’re using high-dose CBD long-term.
Will I fail a drug test if I use CBD?
Possibly. Many CBD products contain trace amounts of THC-even if labeled “THC-free.” In a 2023 study, 1 in 5 CBD products had enough THC to trigger a positive drug test. If your job or legal situation requires drug screening, avoid all CBD products unless they’re from a licensed medical source with guaranteed zero THC.
Is CBG the next big thing for pain?
Early lab results are promising. A 2025 Yale study found CBG reduced pain signals more than CBD or CBN without causing intoxication. But it’s still in preclinical testing. No CBG-based pain products are approved or widely available yet. Don’t buy CBG supplements expecting results-there’s no proof they work in humans.
All Comments
Susie Deer January 15, 2026
CBD is just snake oil sold to gullible people who dont wanna work on their pain. If you want relief get a gym membership or see a PT. Stop wasting money on fancy oils.
Allison Deming January 15, 2026
It is deeply concerning that the public continues to embrace unregulated substances as therapeutic alternatives without demanding the same level of scientific rigor that we expect from pharmaceuticals. The fact that over 40% of CBD products are mislabeled speaks not only to a lack of oversight but to a systemic failure of consumer protection in the realm of wellness marketing. People are not just spending money-they are placing their health in the hands of corporations with zero accountability.
Andrew Freeman January 16, 2026
lol at all these studies saying cbd dont work i tried it for my back and it worked better than ibuprofen so maybe your study is wrong or maybe your body just dont respond to it
says haze January 16, 2026
The real tragedy isn't the lack of efficacy-it's the epistemic collapse of public discourse. We've replaced clinical evidence with anecdotal validation, and now we treat placebo responses as if they're divine revelation. The CBD industry doesn't sell relief; it sells the comforting illusion of agency to people who feel abandoned by medicine. And that, more than any chemical compound, is what's truly dangerous.
TooAfraid ToSay January 18, 2026
You people are so scared of THC you'd rather take placebo gummies from Amazon. I've been using 1:1 tincture for 8 years. My nerve pain? Gone. My anxiety? Better. My job? Still have it. Who wrote this article-a pharmaceutical rep with a grudge?
Henry Sy January 19, 2026
Man I used to think CBD was magic until I spent 600 bucks on that fancy brand everyone raves about and got zero results. Then I switched to a $20 bottle from a dispensary with actual THC in it and suddenly I could sleep without feeling like my spine was on fire. The whole market is a scam unless you're buying from a legit source.
Sarah -Jane Vincent January 20, 2026
They're hiding the truth. The FDA banned real cannabinoid research for decades because Big Pharma didn't want competition. Now they're using 'inconsistent results' as an excuse to keep the market chaotic so they can control the future meds. CBG? They're already patenting it. You think this is about science? Nah. It's about profit.
Alvin Bregman January 22, 2026
I get where you're coming from but i think people just want something that works without the side effects of opioids or NSAIDs. i dont care if its placebo if it helps me get through the day. i started with 5mg cbd and now i do 10mg with a little thc. not perfect but better than screaming in pain every morning
Anna Hunger January 23, 2026
Thank you for presenting a balanced, evidence-based perspective. It is imperative that individuals suffering from chronic pain receive accurate, scientifically validated information rather than being exploited by predatory marketing. I encourage all readers to consult with licensed healthcare professionals before incorporating cannabinoids into their treatment regimen, and to prioritize FDA-regulated products when available.
Dylan Livingston January 24, 2026
Oh wow. Another sanctimonious op-ed dressed up as medical advice. Let me guess-you’ve never had a herniated disc, never spent three years on opioids, never had your insurance deny physical therapy because ‘it’s not medically necessary.’ You sit in your yoga pants sipping oat milk latte and judge people who try to survive. The real villain here isn’t CBD-it’s a healthcare system that leaves people with nothing but desperation and a credit card.