CNS Depressant Risk Calculator
Assess Your Risk Level
This tool helps you understand the risks of combining cannabis with CNS depressants based on medical research.
When you take cannabis along with a sleep aid, anxiety medication, or painkiller, you’re not just adding two effects together-you’re multiplying the risk. The combination of cannabis and other central nervous system (CNS) depressants can slow your breathing to dangerous levels, leave you unconscious for hours, or even cause a fatal overdose. This isn’t theoretical. Emergency rooms across the U.S. and Europe are seeing more cases every year, and the numbers are climbing fast.
How Cannabis Acts Like a CNS Depressant
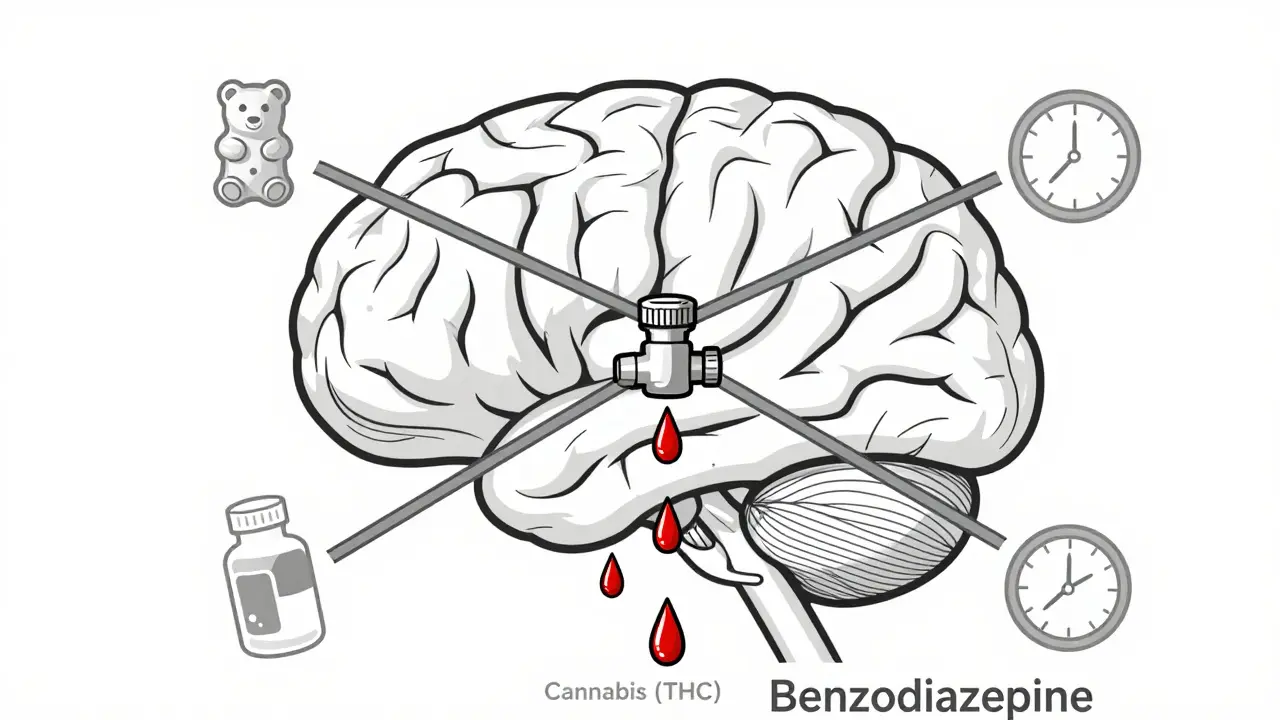
Many people think of cannabis as a stimulant because it can make you feel energetic or giggly at low doses. But at moderate to high doses, especially with THC levels above 10%, it acts just like alcohol, benzodiazepines, or opioids: it slows down your brain and nervous system. The active ingredient, delta-9-tetrahydrocannabinol (THC), binds to CB1 receptors in the brain, reducing nerve signals. This leads to drowsiness, muscle relaxation, slower reaction times, and trouble focusing-exactly what you’d see with a prescription sedative. The effects kick in fast if you smoke or vape: within minutes, peaking around 30 minutes. If you eat it, like in gummies or brownies, it takes 30 to 90 minutes to start, and the high can last 6 to 8 hours. That’s longer than most people expect. And here’s the catch: even experienced users aren’t immune. A single 10 mg dose of THC can impair coordination and memory enough to make driving or operating machinery risky.Why Mixing with Other Depressants Is Dangerous
CNS depressants like benzodiazepines (Xanax, Valium), barbiturates, opioids (oxycodone, morphine), and even some sleep meds all work by boosting GABA, a calming neurotransmitter in the brain. Cannabis doesn’t work the same way, but the result is the same: slower brain activity. When you combine them, the effects don’t just add up-they multiply. This is called additive sedation. A 2020 study in the Journal of Clinical Medicine found that people using both cannabis and benzodiazepines had over three times the risk of ending up in the emergency room compared to those using just the prescription drug. Nearly 70% of those visits were due to breathing problems. Another study showed that patients using cannabis with opioids had a much higher chance of respiratory depression, even at low doses of each. The reason? Both substances suppress the brain’s drive to breathe, but through different pathways. Together, they create a perfect storm. Real stories back this up. One Reddit user reported waking up on the bathroom floor after taking a small amount of Xanax and a puff of 20% THC flower. Their oxygen level had dropped to 82%-a level that can cause brain damage if not corrected quickly. That’s not an isolated case. Between 2019 and 2022, emergency visits involving cannabis and benzodiazepines jumped 42% in the U.S., from 5,521 to 7,842 cases.Who’s at Highest Risk?
It’s not just recreational users. Many older adults are the most vulnerable. They’re often prescribed multiple CNS depressants for chronic pain, anxiety, or insomnia. When they start using medical cannabis for the same conditions, they rarely realize how dangerous the mix can be. A 2021 survey of over 1,200 medical cannabis patients found that nearly 39% were already taking a prescription depressant. Of those, more than 22% had experienced extreme drowsiness, memory blackouts, or difficulty waking up-enough to require medical help. Age plays a big role. People over 65 metabolize drugs slower, so effects last longer and build up faster. The American Society of Anesthesiologists warns that anyone using cannabis within 72 hours of surgery is at risk during anesthesia, which is itself a powerful CNS depressant. One study found cannabis users needed 20-25% more propofol to be put under, but then had 37% more breathing problems when waking up. Even people who think they’re being careful can get caught off guard. A 2023 review of patient reviews on Drugs.com showed consistent complaints: “I slept for 14 hours and couldn’t get up,” “I forgot where I was,” “I felt like I was drowning in my own body.” These aren’t side effects-they’re warning signs.
What Doctors Are Doing About It
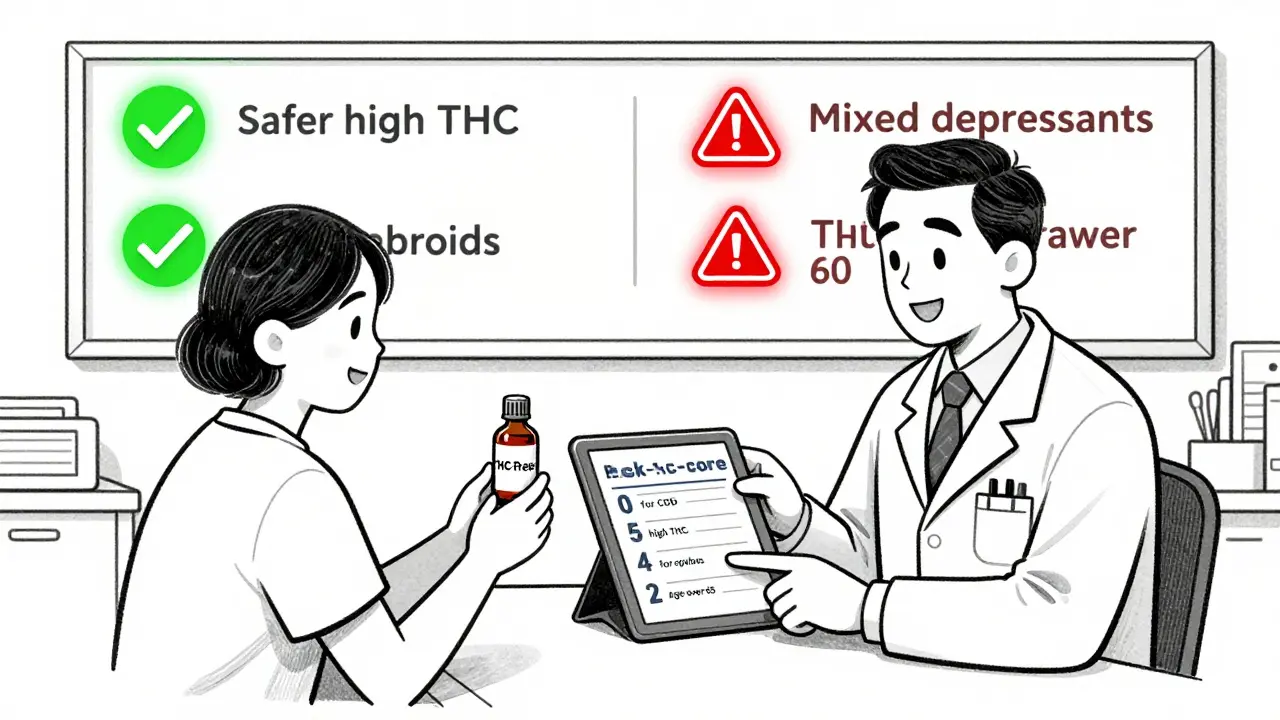
Medical professionals are catching on. The American Medical Association now recommends that doctors ask every patient about cannabis use before prescribing benzodiazepines or opioids. The CDC updated its opioid guidelines in 2022 to explicitly warn that cannabis can make opioids more dangerous. In California, doctors who certify patients for medical cannabis must now complete a mandatory two-hour training on drug interactions. Since the rule started in 2022, high-risk combinations have dropped by 28%. Some hospitals now use a simple risk-scoring tool. It gives points based on: THC concentration (1 point for under 5%, up to 5 for over 15%), type of depressant (3 for benzodiazepines, 4 for opioids, 5 for barbiturates), and patient age (2 points if over 65). A score above 7 means high risk-and doctors should consider alternatives.How to Reduce the Risk If You Must Use Both
If you’re using cannabis for pain, anxiety, or sleep-and you’re also on a depressant-don’t stop without talking to your doctor. But do take steps to lower your risk:- Avoid high-THC products. Stick to products under 10% THC. High-potency flower, concentrates, and edibles are far more likely to cause dangerous sedation.
- Space out your doses. Wait at least 4 hours between taking a depressant and using cannabis. This gives your body time to process one before introducing the other.
- Start low and go slow. Use the smallest effective dose of both. If you’re new to cannabis, begin with 2.5 mg of THC or less.
- Choose CBD-dominant products. A 2022 study in JAMA Internal Medicine found that high-CBD, low-THC oils (150 mg CBD, less than 0.3% THC) showed no significant interaction with alprazolam. CBD may even help balance THC’s sedative effects.
- Never mix with alcohol. Alcohol is a CNS depressant too-and combining it with cannabis increases overdose risk even more.
What the Future Holds
Research is moving fast. The National Institutes of Health spent over $140 million in 2023 on cannabis-drug interaction studies, up from less than $30 million in 2020. Scientists are now testing whether specific cannabinoid ratios-like CBD:THC at 20:1-can reduce risks while keeping benefits. The National Academies of Sciences recommend creating standardized risk scores for clinicians and setting safe THC limits for patients on other depressants. In the U.S., 37 states have medical cannabis programs. By 2025, the American College of Physicians wants every one of them to require interaction screening. If they succeed, they could prevent 2,300 emergency visits each year.Bottom Line
Cannabis isn’t harmless when mixed with sedatives. It’s not just “more sleepy.” It’s potentially life-threatening. The combination can shut down your breathing, erase your memory, and leave you unable to wake up. If you’re using cannabis along with any prescription or over-the-counter depressant, talk to your doctor. Don’t assume it’s safe because it’s “natural.” Your brain doesn’t care where the drug comes from-it only cares about what it does.Can I use CBD instead of THC if I’m on a CNS depressant?
CBD alone, especially in high doses and with minimal THC (under 0.3%), appears to have little to no interaction with most CNS depressants. A 2022 clinical trial found no significant pharmacokinetic interference between high-CBD oil and alprazolam. However, many CBD products still contain trace THC, so always check lab reports. If you’re using CBD for anxiety or sleep, stick to products labeled as THC-free and avoid anything labeled “full-spectrum” unless your doctor approves it.
How long should I wait after using cannabis before taking a sedative?
Wait at least 4 hours after using cannabis before taking a CNS depressant like a benzodiazepine or opioid. If you’ve consumed an edible, wait 6 to 8 hours, since effects last longer. This reduces the chance of overlapping peaks in sedation. But the safest approach is to avoid combining them altogether unless under direct medical supervision.
Is it safe to use cannabis before surgery?
No. The American Society of Anesthesiologists advises avoiding cannabis for at least 72 hours before surgery. Cannabis can interfere with anesthesia, requiring higher doses and increasing the risk of breathing problems during recovery. Even if you’re a regular user, your body may not metabolize anesthetics the same way. Always tell your anesthesiologist about any cannabis use, even if you think it’s unrelated.
What are the signs I’ve taken too much when combining cannabis and depressants?
Danger signs include extreme drowsiness, confusion, slurred speech, slow or shallow breathing (fewer than 8 breaths per minute), inability to wake up, blue lips or fingernails, and loss of coordination. If you or someone else shows these symptoms, call emergency services immediately. Do not wait. Respiratory depression can lead to brain damage or death within minutes.
Do over-the-counter sleep aids or allergy meds interact with cannabis?
Yes. Many OTC products contain diphenhydramine (Benadryl), doxylamine (Unisom), or alcohol-all of which are CNS depressants. Combining them with cannabis can cause the same risks as prescription drugs: excessive sedation, memory loss, and breathing trouble. Always read labels. If a product says “may cause drowsiness,” don’t mix it with cannabis.
Can cannabis help me reduce my opioid or benzodiazepine dose?
Some studies show promise. A 2022 case series found that chronic pain patients reduced opioid use by nearly half by adding low-dose THC (2.5-5 mg) under strict medical supervision. But this only worked with careful dosing, regular monitoring, and no other depressants. Never attempt to self-taper. Always work with a doctor who understands both cannabis and your current medications.
All Comments
Thomas Anderson December 16, 2025
Just got back from my doc’s office-she told me to ditch the Xanax and try low-THC CBD oil for anxiety. Said the combo was risking my breathing. I was skeptical, but after reading this, I’m switching. No more mixing. Simple as that.
Daniel Wevik December 17, 2025
The pharmacokinetic synergy between CB1 agonism and GABAergic potentiation creates a nonlinear respiratory depression profile that’s clinically indefensible. THC’s allosteric modulation of opioid receptor signaling further exacerbates CNS suppression-this isn’t anecdotal, it’s evidence-based polypharmacy risk. We need standardized THC thresholds in prescribing protocols, stat.
Alexis Wright December 17, 2025
Oh wow, another ‘cannabis is dangerous’ scare piece from the medical-industrial complex. You know what’s really killing people? Prescription opioids and alcohol. But let’s blame the plant because it’s easier than regulating Big Pharma’s profit-driven benzodiazepine pipelines. You’re not protecting people-you’re protecting corporate interests. Wake up.
Sinéad Griffin December 19, 2025
AMERICA NEEDS TO STOP THIS CANNABIS FEARMONGERING 😤 I’ve been smoking and taking my sleep meds for years-no problems. You’re just scared of what you don’t understand. #FreeWeed #StopTheWarOnCannabis 🌿🇺🇸
Edward Stevens December 21, 2025
So let me get this straight-you’re telling me that if I take my Ativan and a puff of weed, I might not wake up… but if I take two Ativan, that’s totally fine? 😏 The real danger is trusting doctors who think they can outsmart biology with arbitrary rules.
Jonny Moran December 21, 2025
I’ve been helping my dad manage chronic pain with low-dose THC and physical therapy. He was on oxycodone for years. We cut his dose by 60% after 6 months of careful cannabis use under his pain specialist’s supervision. It’s not magic-but it’s not the monster they make it out to be. Talk to your doctor. Don’t guess.
Rich Robertson December 22, 2025
As someone who’s lived in Canada, the Netherlands, and now back in the U.S., I’ve seen how differently this is handled. In Amsterdam, pharmacies label cannabis potency like alcohol. Here? You’re left guessing if your gummy is 5mg or 50mg. The problem isn’t cannabis-it’s the lack of regulation. Standardize the product, educate the public, and stop treating patients like criminals.
Natalie Koeber December 23, 2025
you know what they dont tell u? the feds planted the ‘cannabis + depressants = death’ story to scare ppl away from using weed so they keep buying pharma drugs. the real cause of those ER visits? synthetic cannabinoids and fake xanax laced with fentanyl. they blame the plant so they can keep selling pills. #cannabisisinnocent #deepstate
Wade Mercer December 25, 2025
People treat cannabis like it’s harmless because it’s ‘natural.’ But nature doesn’t care if you kill yourself. You think your grandma’s sleep aid is safe? It’s not. And neither is your ‘wellness’ vape. This isn’t about freedom-it’s about responsibility. Stop being selfish with your brain.
Daniel Thompson December 26, 2025
Thank you for posting this. I’ve been avoiding telling my psychiatrist I use CBD for anxiety. I thought it was harmless. Now I’m booking an appointment tomorrow. I didn’t realize how much risk I was taking. This post saved me from a potential disaster.