When a standard pill just won’t work, compounded medications step in. They’re not mass-produced like the drugs you pick up at your local pharmacy. Instead, they’re made one at a time-tailored to your body, your allergies, your swallowing problems, or your unique health needs. For some people, they’re the only way to take medicine safely and effectively. But they’re not without risks. Understanding when and how they’re used can mean the difference between relief and serious harm.
Why Standard Drugs Don’t Always Work
Most medications you’ve taken came from a factory, made in bulk with fixed doses and standard ingredients. That works fine for most people. But for about 3-5% of patients, it’s a problem. Maybe you’re allergic to the dye in a pill. Or you can’t swallow capsules. Or your doctor needs you to take exactly 1.5 mg of a drug, but the only pills available are 1 mg and 2 mg. In those cases, a standard drug doesn’t just fall short-it can be dangerous.That’s where compounding comes in. Pharmacists mix ingredients from scratch to create exactly what’s needed. A child who refuses to take a bitter pill might get a cherry-flavored liquid. An elderly patient with stomach issues might get a hormone patch instead of a pill that won’t absorb properly. Someone with multiple medications might get all five combined into one daily gel. These aren’t just conveniences-they’re medical necessities for some.
What Compounded Medications Can Do
Compounded medications offer flexibility that factories can’t match. Here’s what they can do that store-bought drugs can’t:- Adjust dosages precisely-like 1.5 mg or 0.75 mg-when commercial options only come in 1 mg or 2 mg.
- Remove allergens like lactose, gluten, or artificial dyes that trigger reactions in sensitive patients.
- Change the form of the medicine: turn a pill into a cream, a liquid, a suppository, or a lozenge.
- Combine several drugs into one dose to simplify complex regimens-cutting five daily pills down to one.
- Flavor medications for children or elderly patients who refuse to take unpalatable drugs.
- Create bioidentical hormone formulas that match a patient’s natural hormone levels more closely than synthetic versions.
These aren’t theoretical. In 2022, a survey of 1,450 patients found that 82% said compounded medications improved their symptom control. One parent on Reddit shared that their child’s adherence to ADHD medication jumped from 40% to 95% after switching to a flavored liquid compound. For people with chronic pain, a topical gel combining three different pain relievers can reduce side effects while delivering relief directly to the affected area.
When Compounding Goes Wrong
But here’s the catch: compounded medications aren’t FDA-approved. That means no one checks their safety, strength, or purity before they reach you. The FDA doesn’t inspect them the way it does factory-made drugs. And that’s where things can go badly.The 2012 meningitis outbreak linked to contaminated steroid injections from a compounding pharmacy killed 64 people and sickened nearly 800. It wasn’t a mistake-it was a pattern. Poor sanitation, untrained staff, and lack of oversight led to fungal contamination in batches meant for thousands. Since then, the FDA has issued over 12 warning letters to compounding pharmacies in just one year (2022) for issues like improper sterilization and mislabeling.
Even without a major outbreak, quality can vary. One patient on PatientsLikeMe reported that their compounded thyroid medication had wildly inconsistent dosing-sometimes too strong, sometimes too weak. Their TSH levels jumped unpredictably, causing fatigue, heart palpitations, and weight gain. This kind of inconsistency is rare, but it happens. Studies show that compounded drugs account for just 1% of prescriptions but 17% of drug recalls between 2010 and 2020.
Who Should Use Them-and Who Shouldn’t
Compounded medications aren’t for everyone. They’re meant for patients who truly can’t use standard drugs. Here are the best candidates:- Pediatric patients who can’t swallow pills and need flavored liquids or easy-to-swallow gels.
- Patients with allergies to dyes, preservatives, gluten, or lactose in commercial medications.
- Elderly patients with absorption issues who need transdermal patches or suppositories.
- People on five or more daily medications who need a simplified regimen.
- Patients needing hormone therapies with specific bioidentical ratios not available commercially.
- Veterinary patients requiring species-specific dosing (like cats or rabbits) that aren’t made for humans.
On the other hand, avoid compounding if:
- A commercially available FDA-approved drug exists and works for you.
- You’re looking for a cheaper version of a popular drug like semaglutide (Ozempic) without a prescription.
- The pharmacy doesn’t follow strict quality standards or won’t show you their certifications.
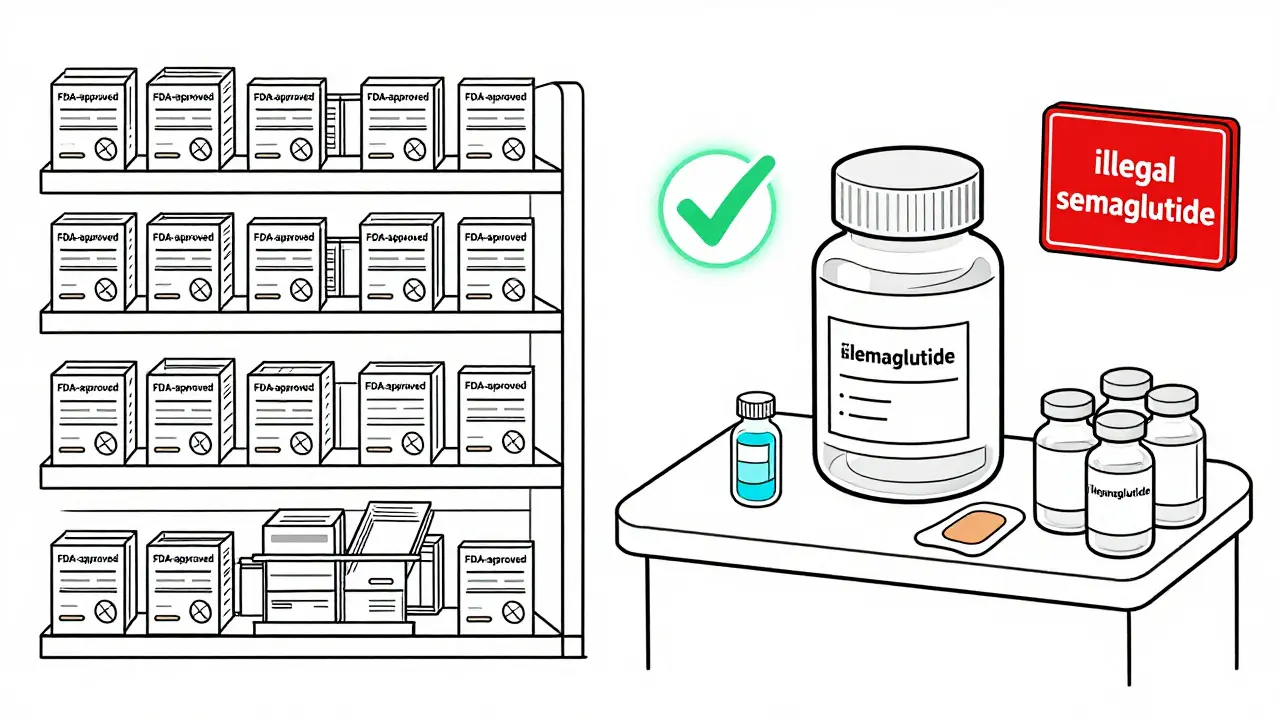
The FDA is cracking down on pharmacies that compound large batches of weight loss drugs like semaglutide and sell them without prescriptions. These aren’t personalized-they’re mass-produced under the guise of compounding. That’s not compounding. That’s manufacturing. And it’s illegal and dangerous.
How to Find a Safe Compounding Pharmacy
Not all compounding pharmacies are equal. In the U.S., about 7,500 pharmacies offer compounding services. But only 350 of them are accredited by the Pharmacy Compounding Accreditation Board (PCAB). That’s less than 5%.Here’s how to pick a safe one:
- Ask your doctor for a referral to a pharmacy they trust.
- Check if the pharmacy is PCAB-accredited. You can verify this on the PCAB website.
- Ask if they follow USP Chapter <795> for non-sterile compounds or <797> for sterile ones. These are national standards for cleanliness and testing.
- Ask if they test their final products for potency and purity. Reputable pharmacies do this routinely.
- Look for reviews from other patients. Specialty compounding pharmacies average 4.6 stars on Healthgrades-nearly a full point higher than general pharmacies that offer limited compounding.
If a pharmacy won’t answer these questions, walk away.
Cost and Insurance
Compounded medications cost more than standard drugs. A simple non-sterile compound might run $30-$100, while a sterile injectable could cost $200-$500. Compare that to a generic pill, which might be $10-$50.Insurance coverage is patchy. Medicare Part D covers only 42% of compounded claims. Private insurers vary widely-some cover them fully, others only if you prove no commercial alternative exists. Always check with your insurer before filling a compounded prescription. You may need a letter of medical necessity from your doctor.
The Future of Personalized Medicine
The future of compounding is getting smarter. Some pharmacies are now using pharmacogenomic testing-analyzing your genes to see how you process certain drugs. One lab in Texas reported 30% better outcomes in patients with CYP2D6 gene variants when their medications were adjusted based on genetic data. This isn’t science fiction-it’s happening now.But experts warn: compounding should be the exception, not the rule. As Dr. Michael Ganio of the American Society of Health-System Pharmacists says, "It’s not about making something new. It’s about filling a gap that no other drug can fill."
Regulators are tightening rules. The 2022 Compounding Quality Act now requires outsourcing facilities to report adverse events and follow stricter quality controls. The FDA is monitoring compounding pharmacies more closely than ever. But the goal isn’t to shut them down-it’s to make sure they’re safe.
Compounded medications save lives. But only when they’re made right. The key isn’t to avoid them-it’s to demand quality. Know why you need them. Know where they come from. And never accept a compounded drug without asking the hard questions.
Are compounded medications FDA-approved?
No, compounded medications are not FDA-approved. The FDA does not review their safety, effectiveness, or manufacturing quality before they’re dispensed. This is different from mass-produced drugs, which go through years of testing and approval. Compounded drugs are made under state pharmacy regulations and national standards like USP <795> and <797>, but they don’t have the same federal oversight.
Can I get a compounded medication without a prescription?
No. Federal law requires a valid prescription from a licensed healthcare provider-like a doctor or nurse practitioner-for every compounded medication. Any pharmacy offering compounded drugs without a prescription is operating illegally. This is especially common with popular weight loss drugs like semaglutide, where some pharmacies falsely market compounded versions as "over-the-counter." These are dangerous and illegal.
How do I know if my compounding pharmacy is safe?
Look for PCAB accreditation-that’s the gold standard. Also, ask if they follow USP <795> for non-sterile compounds or <797> for sterile ones. Ask if they test each batch for potency and purity. Check online reviews and ask your doctor if they’ve worked with the pharmacy before. If they can’t answer these questions clearly, find another pharmacy.
Why do compounded medications cost more?
Because they’re made by hand, one at a time, with specialized equipment and trained staff. A pharmacy that compounds sterile injections needs clean rooms, air filters, and rigorous testing-costs that don’t exist in a factory making thousands of identical pills. Basic non-sterile compounds cost $30-$100; complex sterile ones can hit $500. You’re paying for customization, not mass production.
Can I switch back to a regular drug if my compounded one works?
Yes-if a commercially available, FDA-approved drug becomes available that meets your needs, you should consider switching. Compounded medications are meant for cases where no standard option exists. If a generic version of your drug becomes available and you can tolerate it, your doctor may recommend switching to reduce cost and increase safety. Always consult your provider before changing medications.

All Comments
Elan Ricarte February 7, 2026
Let’s be real-compounding isn’t some magical cure-all. It’s a workaround for a broken system. Pharma companies don’t make 1.5mg pills because they don’t make enough profit. So they force us into this weird gray zone where a pharmacist mixes your meds like a science experiment in someone’s garage. And yeah, sometimes it saves lives. But sometimes it’s just a loophole for lazy doctors and sketchy pharmacies to charge $300 for a jar of flavored jelly that should’ve been a simple pill.
And don’t get me started on the ‘bioidentical hormones’ crap. That’s not medicine-it’s a cult. You’re not ‘matching your natural levels.’ You’re getting a placebo with a fancy label and a price tag that makes your bank account cry.
There’s a reason FDA doesn’t approve these: because they can’t guarantee consistency. One batch makes you feel like a god. The next makes you hallucinate. I’ve seen it. I’ve documented it. And yeah, I’m the toxic analyst who ruins dinner conversations with this stuff.
Camille Hall February 8, 2026
I appreciate the nuance here. Compounding isn’t perfect, but for my sister with severe EDS and multiple allergies, it’s the only thing that lets her take her blood pressure med without breaking out in hives or vomiting.
She used to go weeks without meds because nothing commercial worked. Now, she gets a tiny, dye-free, lactose-free liquid that tastes like mint. Her BP is stable. She’s not in the ER anymore. That’s not a loophole-that’s dignity.
Yes, oversight needs work. But let’s not throw the baby out with the bathwater. The answer isn’t to ban compounding. It’s to fund better regulation, train more pharmacists, and hold bad actors accountable. We can do better than fear-mongering or blind trust.
Ritteka Goyal February 9, 2026
OMG I CANT BELIEVE U R TALKING ABOUT THIS LIKE ITS SOME KIND OF SCIENCE THING LOL
IN INDIA WE JUST USE AYURVEDIC MIXTURES FOR EVERYTHING AND IT WORKS BETTER THAN THESE WESTERN PHARMA GAMES LOL
MY COUSIN TOOK HER HYPERTENSION MEDS FROM A LOCAL HERBALIST AND NOW SHE RUNS 10KM EVERY MORNING AND SHE WAS ON 5 DIFFERENT PILLS BEFORE
WHY DO WE EVEN NEED LABS AND STERILE ROOMS WHEN OUR GRANDMAS KNEW HOW TO MIX HERBS WITH HONEY AND IT WORKED FOR 5000 YEARS
AMERICA IS SO OVERMEDICATED AND AFRAID OF NATURAL THINGS ITS PATHETIC
PS I JUST USED A COMPOUNDED HORMONE CREAM FROM A PHARMACY IN DELHI AND MY SKIN IS SOFT AND I DONT HAVE MOOD SWINGS ANYMORE
YALL NEED TO STOP WORSHIPING FDA AND START TRUSTING TRADITION
LOL SORRY FOR THE TYPING IM ON MY PHONE AND MY THUMB IS SLIPPING
Jonah Mann February 9, 2026
Okay, I’ve been a pharmacist for 18 years, and I’ve compounded hundreds of prescriptions. Most of them? Perfect. Safe. Life-changing.
But here’s the thing no one talks about: the bad ones? They’re not from PCAB-accredited pharmacies. They’re from fly-by-night operations that use a kitchen blender and call it a ‘compounding station.’
And yeah, the FDA doesn’t inspect them before they ship-that’s true. But the *good* pharmacies? They test every batch. They use HPLC machines. They have clean rooms with HEPA filters. They’re more meticulous than the factory that makes your iPhone.
So don’t hate compounding. Hate the unregulated ones. And if you’re a patient? Ask for the test report. If they can’t give it to you, walk out. Simple.
Also-yes, the cost sucks. But if your kid can’t swallow a pill and you’re giving them a shot in the butt every day? You’ll pay $400 for a cream that works. No regrets.
THANGAVEL PARASAKTHI February 10, 2026
Very informative post. I am from India and we have been doing compounding for ages. In rural areas, we often mix medicines as per patient needs because commercial options are not available or too expensive.
For example, we combine antihypertensives and diuretics into one syrup for elderly patients who can’t take multiple tablets. It works. We use clean glassware, sterilized spoons, and store in dark bottles.
Maybe we don’t have PCAB, but we have experience, care, and trust. Maybe the real issue isn’t the method-it’s the profit-driven system that ignores patient needs.
Also, I’ve seen compounding save lives in dialysis patients who can’t tolerate preservatives. So let’s not throw the baby out with the bathwater. Regulation yes. Eradication no.
Tricia O'Sullivan February 10, 2026
Thank you for presenting this issue with such clarity and balance. It is refreshing to encounter a discussion that acknowledges both the indispensable utility of compounded medications and the legitimate concerns regarding regulatory oversight.
The distinction between personalized therapeutic necessity and commercial exploitation is, indeed, paramount. One cannot help but reflect upon the ethical imperative to ensure that patient safety remains the unequivocal priority, irrespective of economic or systemic pressures.
It is my sincere hope that future policy will prioritize accreditation, transparency, and evidence-based practice-not as bureaucratic hurdles, but as non-negotiable standards of care.
Scott Conner February 11, 2026
Wait so if a pharmacy makes a cream with three pain meds in it… is that considered compounding? Or is that just… mixing? Like… what’s the difference between that and a pharmacy just dumping stuff in a jar?
Also-how do they even test potency? Do they send a sample to a lab? Or just guess? I’m genuinely confused. I thought all meds had to be tested. But you said FDA doesn’t inspect them… so who does?
And why does one pharmacy charge $80 and another $220 for the same thing? Is it the ingredients? Or just… how much they think you’ll pay?
Kathryn Lenn February 13, 2026
Oh wow. So the FDA doesn’t regulate these? That’s wild. I bet the same people who are screaming about Big Pharma are also secretly ordering compounded Ozempic from some guy in Florida who runs it out of his garage.
And let’s not forget-this whole thing is just a tax write-off for insurance companies. Why pay $10 for a generic when you can pay $300 for a ‘custom’ version and make the patient feel special?
Also, ‘bioidentical hormones’? That’s just a fancy word for ‘we don’t have the science so we made up a word.’
And PCAB accreditation? Sure. Just like ‘organic’ on a bag of chips. Sounds legit. Doesn’t mean squat.
Next thing you know, they’ll be compounding vaccines in a bathtub and calling it ‘holistic immunity.’
Y’all are being played. Again.
Angie Datuin February 14, 2026
I have a friend whose daughter has a rare metabolic disorder. She can’t process any fillers or preservatives. Without compounded meds, she’d be dead by now.
I used to think this was a niche thing. Now I see how many people are just one allergy away from being trapped in a system that doesn’t care.
It’s not about conspiracy. It’s about humanity. We need to fix this-not trash it.
Monica Warnick February 15, 2026
Okay, so I’ve been on a compounded thyroid med for 3 years. Last month, my TSH went from 2.1 to 8.7. I felt like a zombie. My hair fell out. I cried every day.
I went back to the pharmacy. They said, ‘Oh, the batch was off.’
They gave me a new one. TSH dropped to 0.9. I got anxiety attacks. Heart racing. Couldn’t sleep.
I’m done. I don’t trust this. I don’t trust them. I don’t trust the ‘PCAB’ sticker. I don’t trust the ‘USP’ thing.
I just want a pill that doesn’t make me feel like I’m being slowly poisoned by a lab accident.
And now I’m terrified to even take my blood pressure med.
Someone please tell me I’m not alone.
Ashlyn Ellison February 17, 2026
My cat got a compounded pain med after surgery. It was a tiny gel on her ear. She licked it. Didn’t even flinch. She’s running around like a lunatic now. Worth every penny.
Also-yes, I cried when I saw the bill. But I’d pay $500 again if it meant she wasn’t in pain.