Cumulative Drug Toxicity Calculator
How much is too much?
Cumulative toxicity happens when medications build up in your body over time. This calculator helps you understand your total exposure compared to safe limits.
How it works: This calculator estimates your total exposure based on daily dose and duration. Cumulative toxicity depends on how much drug your body has absorbed over time, not just the daily dose.
Most people think side effects show up right away. You take a new pill, feel dizzy or nauseous, and you assume it’s the drug’s fault. But what if the problem isn’t the first dose - it’s the 50th? Or the 200th? That’s cumulative drug toxicity: side effects that don’t appear until months or years later, because your body has been quietly hoarding the drug, molecule by molecule, until it finally crosses a dangerous line.
How Your Body Stores Drugs You Don’t Even Notice
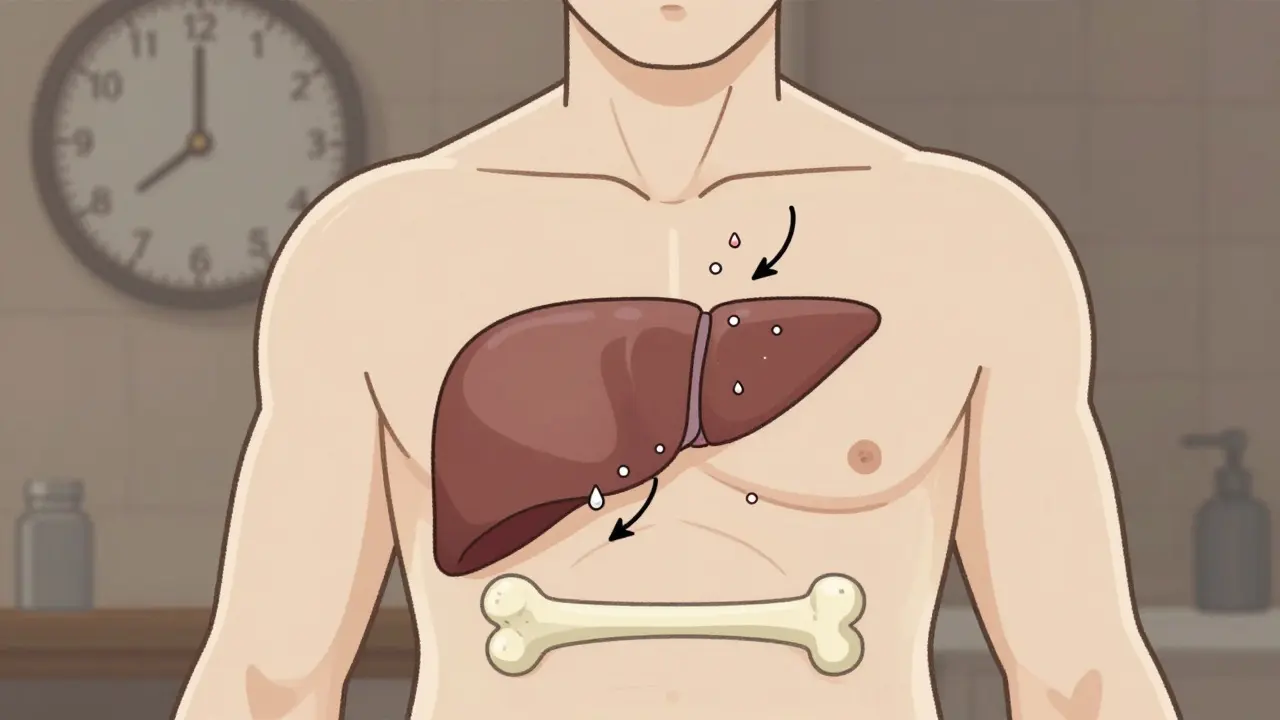
Not all drugs leave your system quickly. Some stick around - especially if they’re fat-soluble. Think vitamin A, D, E, K, or heavy metals like lead and mercury. These don’t wash out with urine. Instead, they settle into your fat tissue, bones, or liver. Over time, they build up. Even if you take the same dose every day, your body can’t keep up. The amount in your bloodstream slowly climbs. By the time you feel anything, you might have already taken 10 times the safe limit. This isn’t rare. In fact, it’s common in long-term treatments. Cancer drugs like doxorubicin, heart meds like digoxin, antibiotics like amiodarone, and even blood thinners like warfarin can all cause problems this way. The key isn’t how much you take each day - it’s how much you’ve taken in total. That’s the cumulative dose.Why Older Adults Are at Higher Risk
Your liver and kidneys don’t work the same way at 70 as they did at 30. As you age, your body’s ability to break down and flush out drugs drops by 30% to 50%. That means a drug that was perfectly safe for years suddenly starts building up. A 2019 study in the Journal of the National Cancer Institute found that nearly 68% of serious side effects in elderly patients on chronic meds came from this slow accumulation - not from overdosing or mistakes. That’s why the American Geriatrics Society updated its Beers Criteria in 2023 to list 34 medications with high cumulative risk for older adults. For example, anthracycline chemotherapy drugs have a hard cap: no more than 450 mg/m² over a lifetime. Exceed that, and your heart muscle starts dying. It doesn’t happen overnight. It happens after 10 cycles. After 20. After years of thinking you’re fine.What Happens When the Damage Finally Shows Up
Cumulative toxicity doesn’t scream. It whispers. First, you feel a little more tired. Then your hands go numb. Your skin turns gray. Your breathing gets shallow. By the time you see a doctor, the damage might be irreversible. One real case from a Reddit thread in March 2023 tells the story: a patient on amiodarone for heart rhythm problems had normal blood tests every month. No signs of trouble. But after taking a total of over 600 grams - well above the safe limit - they developed severe lung scarring. The damage was so advanced, treatment options were gone. The doctor said: "We monitored levels. We didn’t monitor the total dose. That was our blind spot." This isn’t isolated. The FDA’s Adverse Event Reporting System logged over 12,000 cumulative toxicity cases between 2018 and 2022. Nearly half involved blood thinners. Almost a third involved heart drugs. These aren’t accidents. They’re predictable - if you’re tracking the numbers.How Doctors Miss It - and How They Can Stop
Most clinics don’t track cumulative doses. They track daily doses. That’s like checking your car’s fuel level every morning but never looking at the odometer. You know you’re refilling, but you don’t know how far you’ve driven. Therapeutic drug monitoring - measuring drug levels in your blood - helps, but only if the drug is cleared quickly. For drugs that build up in fat, blood levels can look normal even when your tissues are overloaded. That’s why the American Society of Health-System Pharmacists recommends specific protocols for drugs like digoxin, lithium, and aminoglycosides. But only 38% of electronic health records today can automatically calculate cumulative doses. The good news? When clinics do track it, outcomes improve. A 2021 study in the Journal of Clinical Pharmacy and Therapeutics showed that a simple cumulative dose tracker in a rheumatology clinic cut methotrexate-related hospitalizations by 37%. Pharmacists who took charge of these calculations reduced hospital admissions for drug toxicity by 29% across 45 healthcare systems.What You Can Do - Even If You’re Not a Doctor
You don’t need a medical degree to protect yourself. Here’s what works:- Know your drugs. If you’ve been on a medication for more than six months, ask: "Could this build up?" Look up the drug’s half-life. If it’s over 24 hours, it’s a candidate for accumulation.
- Track your total dose. Keep a log. Write down the name, dose, and how long you’ve been taking it. Use a phone app if it helps. Many pharmacies now offer dose trackers.
- Ask for a cumulative dose review. At your next appointment, say: "I’ve been on this for X years. Has my total dose been checked?" If your doctor doesn’t know, they’re not alone - but you can be the one to start the conversation.
- Watch for slow changes. Fatigue, memory fog, tingling, dry skin, shortness of breath - if these creep in over months, don’t brush them off as "getting older." Ask if they could be linked to your meds.
The Future Is Coming - But You Don’t Have to Wait
New tools are on the way. AI models at Memorial Sloan Kettering are now predicting individual toxicity risk with 82% accuracy by analyzing 27 factors - from genetics to kidney function. The FDA’s Sentinel system now scans data from 190 million patients to spot hidden patterns of accumulation. And starting in January 2024, the European Medicines Agency requires all new chronic-use drugs to include cumulative toxicity assessments. But you don’t have to wait for tech to save you. The tools are already here: your memory, your logbook, your questions. The biggest risk isn’t the drug - it’s assuming you’re safe because you feel fine today. Cumulative toxicity doesn’t care about how you feel. It only cares about how much you’ve taken.When to Get Help
If you’ve been on any of these meds for over a year - especially if you’re over 65 - and you’ve noticed new symptoms, talk to your doctor or pharmacist now:- Amiodarone (for heart rhythm)
- Digoxin (for heart failure)
- Lithium (for bipolar disorder)
- Methotrexate (for arthritis or cancer)
- Anthracyclines (like doxorubicin)
- Long-term antibiotics like tetracycline or minocycline
- Chronic NSAIDs (like ibuprofen or naproxen)
Can cumulative drug toxicity be reversed?
Sometimes, but not always. If caught early - before organ damage occurs - stopping the drug and letting your body clear the buildup can lead to full recovery. But if the toxicity has already damaged your liver, lungs, or heart, the damage may be permanent. That’s why early detection matters more than treatment.
Do over-the-counter drugs cause cumulative toxicity?
Yes. Long-term use of NSAIDs like ibuprofen or naproxen can cause kidney damage or stomach bleeding that builds up slowly. Even daily use of acetaminophen (Tylenol) can lead to liver toxicity over time, especially if you drink alcohol or have existing liver issues. There’s no "safe" daily dose for these drugs if taken for years without monitoring.
Why don’t doctors check cumulative doses more often?
Most electronic health records don’t track it automatically. Doctors are busy. They’re trained to watch for immediate side effects, not long-term accumulation. And many drugs don’t have clear cumulative limits listed in guidelines. But that’s changing. Pharmacists and tech tools are stepping in to fill the gap - but you need to ask.
Is cumulative toxicity only a problem for cancer patients?
No. While cancer drugs are the most studied, cumulative toxicity affects anyone on long-term meds: people with arthritis, heart disease, epilepsy, depression, or chronic pain. In fact, the most common cases reported to the FDA involve blood thinners and heart medications - not chemotherapy.
How long does it take for a drug to build up to dangerous levels?
It depends on the drug and your body. For some, like amiodarone, it can take 6-12 months. For others, like lithium, it can happen in weeks if your kidneys slow down. Fat-soluble drugs like vitamin A can take years. There’s no universal timeline - that’s why tracking your total dose is the only reliable way to know.
Don’t assume your meds are safe just because you’ve taken them for years. The body doesn’t forget. And neither should you.
All Comments
Jake Moore January 18, 2026
Man, I had no idea this was a thing. My grandma’s on digoxin and she’s been complaining about fatigue for months. We just thought it was aging. Now I’m gonna print out this post and hand it to her cardiologist. This needs to be standard practice.
Joni O January 20, 2026
thank you for this!! i’ve been on methotrexate for 5 years and my dr never mentioned cumulative dose. i started tracking it in my notes app last week. just got my first blood test back and my liver enzymes are normal, but now i’m gonna ask for a full review. you’re right-don’t wait for symptoms.
Eric Gebeke January 21, 2026
Of course this is happening. The pharmaceutical industry doesn’t want you to know that your pills are slowly poisoning you. They profit from long-term use, not from patients getting better. It’s not negligence-it’s a business model. You think they’d warn you? Ha. They’d rather see you on a transplant list than admit their drugs are toxic over time.
Ryan Otto January 22, 2026
Let’s be honest: this isn’t just about pharmacokinetics. It’s about the complete failure of Western medicine to treat the human body as a dynamic system. We quantify everything except the total burden. The FDA’s 12,000-case database? That’s the tip of the iceberg. The real number is hidden in unreported deaths labeled as "cardiac arrest" or "natural causes." You’re being lied to by the system that claims to protect you.
Max Sinclair January 23, 2026
Really appreciate the practical advice here. I’m a nurse and I’ve seen this happen too many times. The biggest barrier isn’t knowledge-it’s workflow. If EHRs could auto-calculate cumulative dose and flag high-risk patients, we’d prevent so much harm. Maybe someone should build a plugin for Epic? I’d use it tomorrow.
Praseetha Pn January 25, 2026
They don’t tell you this because they’re scared you’ll stop taking your meds and start drinking colloidal silver and eating kale smoothies with moonlight-infused turmeric. But guess what? Your liver doesn’t care about your Instagram detox trends-it cares about 3000 mg of ibuprofen over 12 years. And yeah, Big Pharma is in bed with the FDA, but so is your doctor who just got a free lunch from a rep. Wake up, sheeple!
Nishant Sonuley January 25, 2026
Look, I get it-you’re trying to sound smart with all this cumulative toxicity talk. But let’s not pretend this is new. In India, we’ve been dealing with this for decades because people can’t afford to switch drugs every six months. My uncle took tetracycline for acne for 11 years. His kidneys gave out at 52. We didn’t have fancy EHRs, but we had grandmas who remembered every pill you ever took. Maybe we’re the ones who got it right all along-by just paying attention, not waiting for AI to save us.
Emma ######### January 27, 2026
This made me cry. My mom died from lung fibrosis after 14 years on amiodarone. They said her blood levels were fine. She never knew she’d hit 700 grams. I wish I’d known then what I know now. Thank you for writing this. I’m sharing it with everyone I know on long-term meds.
Danny Gray January 28, 2026
Interesting. But if we’re talking about accumulation, why not also talk about the accumulation of trauma, stress, and societal neglect? Maybe the real toxicity isn’t in the pill-it’s in the system that forces people to stay on pills for decades because they can’t afford therapy, nutrition, or rest. You’re blaming the drug, but the drug is just a symptom of a broken world.
Tyler Myers January 28, 2026
So let me get this straight-you’re telling me my 10-year-old prescription for lithium is slowly turning my brain into mush and no one told me? And now you want me to trust some app I downloaded from the App Store? LOL. I’ve been on this since college. My doctor’s been my best friend. You think I’m gonna stop because some guy on Reddit says so? Nah. I’ll keep taking it. And if I die? At least I died happy. Unlike you, probably.