When a patient picks up a prescription and sees a pill that looks completely different from what they’re used to, their first thought isn’t always, “This is cheaper.” More often, it’s, “Is this even the same drug?” That moment of doubt is real, common, and costly. In the U.S., 90.9% of prescriptions are filled with generics, yet nearly one in four patients still hesitate to take them. The problem isn’t that generics don’t work-they do. The problem is that patients don’t believe they do.
Why Patients Doubt Generics
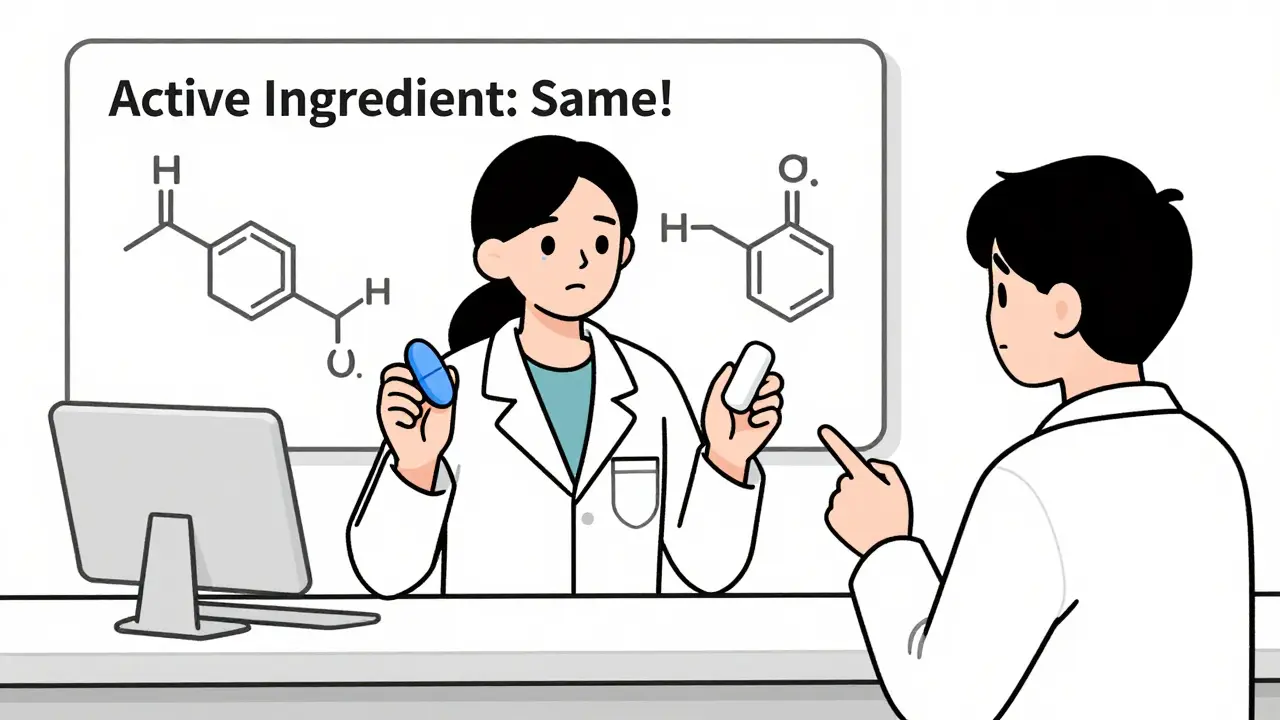
It’s not about intelligence. It’s about trust. Patients see a brand-name pill they’ve taken for years-say, a blue oval with “Lipitor” stamped on it-and suddenly, they get a white rectangle with no name at all. Their brain doesn’t register “same active ingredient.” It registers “different.” And in health, different feels dangerous. Research shows 78% of patients worry about changes in pill shape, color, or size. Even worse, 43% think generics contain only 80% of the active ingredient-when the FDA requires them to be within 80-125% of the brand’s bioequivalence. That’s not a gap. That’s a misunderstanding. And it’s not the patient’s fault. No one explained it. Some patients worry about manufacturing. They’ve heard stories-some true, some exaggerated-about overseas labs and quality control. Others fear that because it’s cheaper, it’s inferior. But cost isn’t the issue. It’s perception. And perception is shaped by how we talk about it.The Wrong Way to Talk About Generics
Saying “It’s the same drug, just cheaper” doesn’t work. In fact, it backfires. A 2023 review in U.S. Pharmacist found that when pharmacists used that phrase, patient acceptance dropped to just 31%. Why? Because it implies the only reason to switch is money-not quality, not safety, not science. And when you reduce a life-changing medication to a price tag, patients start to wonder: “If it’s so good, why isn’t my doctor prescribing the brand?” Another common mistake? Waiting until the patient asks. Too many pharmacists only address concerns when they’re already voiced. But by then, doubt has taken root. The best outcomes come from preemptive, calm, and confident conversations-not reactive defensiveness. And never dismiss a concern. If a patient says, “This pill doesn’t work like the other one,” don’t say, “That’s just in your head.” You’re not just invalidating their experience-you’re breaking trust.The Right Way: The VALUE Framework
The most effective approach isn’t about reciting facts. It’s about connection. The VALUE framework, backed by clinical data from the U.S. Pharmacist’s 2023 review, works because it starts with empathy:- Validate concerns: “I understand this looks different from what you’ve taken before.”
- Acknowledge feelings: “It’s totally normal to feel unsure when your medication changes.”
- Listen actively: Let them finish. Don’t interrupt. Pause. Look them in the eye.
- Understand perspective: “What’s been your experience with this medication so far?”
- Educate with empathy: “Here’s what’s actually in it-and why it’s safe.”
Use the ‘Ask-Tell-Ask’ Method
The FDA and the Journal of General Internal Medicine found that providers using the Ask-Tell-Ask method saw 68% of patients accept generics-compared to just 42% with regular explanations. Here’s how it works:- Ask: “What do you know about this generic version?”
- Tell: “The FDA requires it to have the exact same active ingredient, and it must work the same way in your body. The only differences are the color, shape, or name-because the brand company paid for the packaging, not the medicine.”
- Ask: “Can you tell me back what you understood?”

Personal Endorsement Changes Everything
Patients don’t just want facts. They want reassurance from someone they trust. A study in the American Journal of Managed Care found that when providers said, “I prescribe this generic for my own family,” acceptance jumped by 37 percentage points. Why? Because it’s human. It says, “I’m not just selling you this-I’m living it.” You don’t have to share your personal life. But you can say: “I’ve seen hundreds of patients switch to this, and their blood pressure, cholesterol, or diabetes numbers stayed exactly the same.” Or: “This is the same medication my sister takes for her high blood pressure. She’s been on it for five years with no issues.” Personal stories build bridges. Data alone builds walls.Timing Matters More Than You Think
The FDA’s 2022 report found that 89% of patients accepted generics when they heard about the switch at the time of prescribing. Only 63% accepted it when they found out at the pharmacy counter. That’s because by the time they get to the pharmacy, they’ve already formed an opinion. If the doctor didn’t mention it, they assume it’s a cost-cutting move-not a clinical one. The best practice? Prescribers should mention generics when writing the script. Pharmacists should reinforce it at pickup. Teamwork increases acceptance to 85%-far higher than either profession working alone.Use Visuals, Not Just Words
A Healthcare Hotline survey found that 68% of patients would accept generics if they could see a side-by-side comparison of the brand and generic pills. And 41% specifically asked for photos. The FDA now offers free digital tools-including 3D pill images and videos showing how bioequivalence is tested. Keep a tablet or printed chart in your counseling area. Show them the pills. Point out the active ingredient listed on both. Say: “Look-this part is identical. The rest is just the shell.” For patients who are visually oriented, this cuts through confusion faster than any speech.Don’t Lead With Cost
It’s tempting. Generics save patients hundreds a year. But research shows that when cost is the only reason given, trust drops by 22%. Instead of saying, “This saves you $50 a month,” say: “This contains the same active ingredient as the brand, but without the marketing costs. That’s why it’s priced lower-but the effect on your body is the same.” The difference? One focuses on money. The other focuses on science-and respects the patient’s intelligence.
All Comments
Stephen Craig January 5, 2026
It’s not about the pill. It’s about the story we tell ourselves about it.
Same chemistry, different packaging-and we treat it like a betrayal.
We’re wired to equate familiarity with safety. That’s not irrational. It’s evolutionary.
But we’ve forgotten that trust isn’t built by labeling something ‘generic’-it’s built by listening when someone says, ‘This doesn’t feel right.’
The VALUE framework isn’t a tactic. It’s a return to medicine as human work.
Connor Hale January 7, 2026
That 37-point jump when providers say they prescribe it for their own family? That’s the whole thing.
People don’t trust data. They trust people who look them in the eye and say, ‘I’d give this to my mom.’
Everything else is just noise.
Roshan Aryal January 8, 2026
Oh please. This whole ‘VALUE framework’ is just corporate fluff wrapped in pseudoscience.
Generics are made in India and China by factories that don’t even follow their own regulations.
You think the FDA inspects every batch? Please. They inspect one in ten-and that’s if the moon is in the seventh house.
And don’t get me started on ‘bioequivalence’-that’s a legal loophole dressed up as science.
Patients aren’t stupid. They smell the corruption. You’re just giving pharmacists a script to lie with a smile.
Jack Wernet January 10, 2026
While the VALUE framework presents a commendable shift toward patient-centered care, it is imperative to recognize that its efficacy is contingent upon systemic support.
Pharmacists, often overburdened and under-resourced, cannot be expected to deliver nuanced, empathetic counseling without adequate time, training, and compensation.
Moreover, the emphasis on personal endorsement, while psychologically potent, risks blurring professional boundaries if not applied with clinical discretion.
The data is compelling, but implementation remains the true frontier.
Catherine HARDY January 11, 2026
I’ve been on the same brand for 12 years. Last month they switched me without telling me.
Three days later I had the worst headache of my life.
They said it was ‘the same thing.’
But my blood pressure spiked. My doctor didn’t care.
Now I’m scared to take anything new.
What if this is how they start replacing our meds with something that makes us sick on purpose?
They’re not trying to save money-they’re trying to control us.
Vicki Yuan January 12, 2026
Every single point in this article is backed by peer-reviewed evidence-and yet, so many pharmacists still default to ‘It’s cheaper.’
It’s not laziness. It’s systemic neglect.
We’ve turned healthcare into a transaction, not a relationship.
The Ask-Tell-Ask method isn’t just effective-it’s ethical.
And the fact that Kaiser Permanente saw an 81% acceptance rate? That’s not magic.
That’s what happens when you treat patients like people who deserve to understand their own bodies.
Let’s stop pretending we’re just pill dispensers.
We’re the last line of defense against misinformation.
And we’re failing.
Uzoamaka Nwankpa January 13, 2026
I come from Nigeria, where generics are the only option-and people still die because they don’t trust them.
But here’s the truth: in places with no brand names, people just take what’s given.
It’s not about the pill.
It’s about having enough to eat, clean water, and someone who looks at you like you matter.
When you’re hungry, you don’t care what color the pill is.
But when you’re comfortable, you start worrying about shapes and names.
That’s not science. That’s privilege.
Chris Cantey January 13, 2026
What if the reason generics ‘don’t work’ for some people isn’t perception?
What if it’s because the inactive ingredients-fillers, dyes, binders-are different?
And we know those can trigger reactions in sensitive people.
But no one talks about that.
Because the FDA doesn’t require equivalence for those.
So we’re told to trust the ‘active ingredient’-but what about the rest?
It’s not paranoia.
It’s biology.
And we’re ignoring it because it complicates the narrative.
Abhishek Mondal January 15, 2026
Let’s be brutally honest: this entire ‘VALUE’ framework is a Band-Aid on a hemorrhage.
Pharmacists are being asked to perform emotional labor while being paid minimum wage to dispense pills.
Meanwhile, pharmaceutical conglomerates profit from brand-name monopolies, then lobby to force generic substitution.
The system is rigged.
You can’t fix a broken machine with a PowerPoint slide titled ‘Listen and Empathize.’
And don’t even get me started on the FDA’s ‘free digital tools’-they’re a PR stunt.
Real reform requires dismantling patent laws, not teaching pharmacists to smile more.
Oluwapelumi Yakubu January 16, 2026
Man, this is the kind of content that makes me proud to be in healthcare.
You know what’s wild? In Lagos, we don’t even have brand names-just generics, all day, every day.
But here’s the thing: when you explain it right, people get it.
Not because you’re a genius.
But because you didn’t treat them like a number.
I tell my patients: ‘The medicine is the same. The bottle is just a new jacket.’
They laugh. Then they take it.
It’s not rocket science.
It’s just being human.
And honestly? That’s the most powerful thing we’ve got left.