Every year, over 51 million dispensing errors happen in U.S. community pharmacies. Most of these mistakes never reach patients-not because of barcode scanners or double-check systems, but because a pharmacist asked a simple question: "What is this medication for?" That moment of conversation is the most powerful tool we have to stop errors before they hurt someone.
Why Patient Counseling Catches What Machines Can't
Barcode scanners catch about 53% of dispensing errors. Pharmacist double-checks catch 67%. But patient counseling? It catches 83%. That’s not a small edge-it’s the difference between a near miss and a preventable harm. Why? Because machines can verify the pill bottle matches the prescription. They can’t know if the patient thinks they’re taking a blood pressure pill when it’s actually for diabetes. They can’t hear the hesitation in a voice or notice a confused frown when the pharmacist says, "This is your new insulin." The key isn’t just talking. It’s asking the right questions in the right way. Closed questions like "Is this for your cholesterol?" miss more than half the errors. Open-ended ones like "What do you understand this medicine is supposed to do?" catch 3.2 times more mistakes. That’s not guesswork-it’s data from Pharmacy Times and the National Institutes of Health. When patients explain it in their own words, pharmacists hear gaps in understanding that no system flags.The Four-Step Verification Routine
There’s a proven structure for turning counseling into a safety net. It’s not complicated, but it requires discipline. Here’s what works, based on the American Pharmacists Association’s 2023 guidelines:- Confirm identity (27 seconds): "Can you please confirm your full name and date of birth?" This catches 12% of errors where the wrong patient’s script was filled.
- Verify purpose (43 seconds): "What condition are you taking this for?" If the patient says "for my knee pain" when it’s actually a blood thinner, you’ve just stopped a potential stroke.
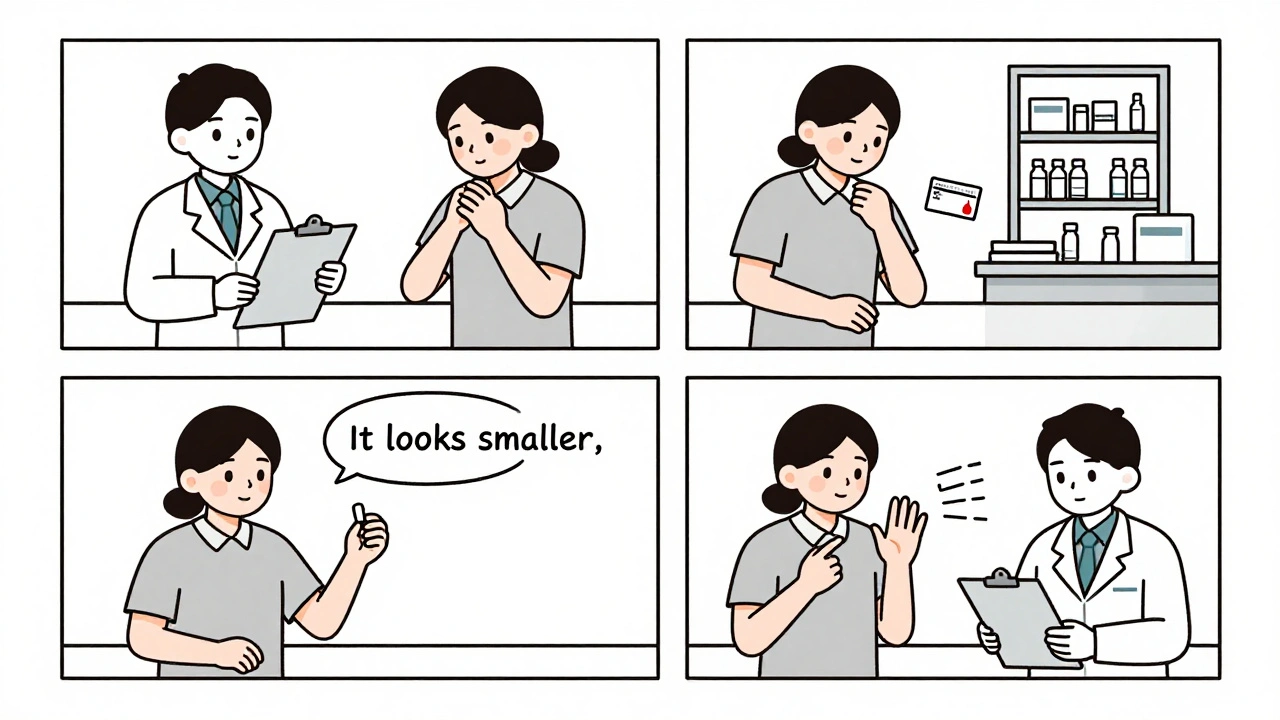
- Check appearance and instructions (52 seconds): Show the medication. Ask: "Does this look like what you’ve taken before?" Then ask them to demonstrate how they’ll take it. This catches look-alike pills, wrong strengths, and misunderstood dosing-like confusing once-daily with twice-daily. This step alone catches 29% of errors involving insulin, opioids, or anticoagulants.
- Review interactions and allergies (38 seconds): "Are you taking anything else? Even over-the-counter or herbal supplements?" Many errors happen because the patient didn’t mention fish oil, St. John’s wort, or a new blood pressure pill from another doctor.
That’s 2 minutes and 40 seconds per prescription. It’s not fast. But it’s the most cost-effective safety step in pharmacy. At $0.87 per prescription, it’s cheaper than barcode systems ($1.35) and far less expensive than the average malpractice claim from a dispensing error-which can run over $100,000.
Where Counseling Falls Short-and How to Fix It
Counseling isn’t magic. It only works if the patient is there, awake, and willing to talk. About 19% of patients decline counseling. Some are in a rush. Others think they already know what they’re taking. That’s where the gap opens.Here’s the reality: counseling works best on new prescriptions-catching 91% of errors. It’s less effective on refills, where patients may not notice a change in pill color or size. For refills, you need to be extra careful. Ask: "Has anything changed since your last fill?" Even if they say no, check the label. A change in strength from 5mg to 10mg? That’s a red flag.
Another problem? Time pressure. Pharmacists in chain stores average just 1.2 minutes per counseling session-far below the 2.3 minutes needed to catch most errors. Why? Corporate productivity targets. Techs are told to speed up the line. But here’s what independent pharmacies found: when they gave pharmacists more time for counseling, their malpractice insurance premiums dropped 19%. Patients noticed too. In 89% of reviews, people praised pharmacists who took the time to explain. "The pharmacist caught that my new blood thinner was the wrong strength when I said it looked smaller than before," one patient wrote on Healthgrades. That’s trust. That’s loyalty. That’s business.
Who Needs It Most-and Why
Not every patient needs the same level of counseling. High-risk groups need extra attention:- Patients over 65: Dosing errors are 3.7 times more likely to cause serious harm.
- Patients with low health literacy: They account for 42% of undetected errors. Use plain language. Avoid terms like "anticoagulant." Say "blood thinner."
- New users of high-alert medications: Insulin, opioids, warfarin, lithium. One mistake here can be deadly. The ISMP says 1 in 5 dispensing errors involve these drugs.
- Patients on 5 or more medications: Complex regimens are where mix-ups happen. Ask: "Can you walk me through your morning pills?"
These are the patients who benefit most from the "teach-back" method. Don’t just tell them. Ask them to repeat it back. "Can you tell me how you’ll take this pill?" If they can’t, you haven’t finished counseling.
Real Results from Real Pharmacies
CVS Health ran a pilot in 150 stores where technicians asked: "Does this look like what you’ve taken before?" In three months, they caught 1,247 errors that would’ve reached patients. Walgreens’ "Medication Checkpoint" protocol-showing the pill, asking purpose, and verifying instructions-cut dispensing errors by 58%.Meanwhile, independent pharmacies that implemented the full 2-minute-40-second protocol saw error detection jump from 61% to 85% in just six months. They didn’t hire more staff. They just changed how they talked to patients.

What’s Changing in 2025
Regulations are catching up. CMS now ties 8.5% of Medicare Part D reimbursement to documented counseling that includes error verification. Thirty-four states require counseling for new opioid prescriptions. The proposed 2024 Federal Pharmacy Safety Act would expand that to all high-alert meds.Technology is helping too. New tools like Surescripts’ "Counseling Checkpoint" API let pharmacists log verification steps directly into their workflow in seconds. Early adopters say it cuts counseling time by 22% without losing accuracy.
The message from the FDA, ISMP, and ASHP is clear: patient counseling isn’t just a nice-to-have. It’s the last, best line of defense against dispensing errors. No algorithm can replace a pharmacist who listens.
How to Start Today
You don’t need a new system. You don’t need a big budget. You just need to change how you talk.- Stop asking yes/no questions. Start asking "what" and "how."
- Use the four-step routine every time-new script or refill.
- Train techs to do preliminary checks. In 42 states, they can legally verify patient identity and medication purpose under pharmacist supervision.
- Document everything. Use NABP’s 2022 standards. If you didn’t write it down, it didn’t happen.
- Measure your results. Track how many errors you catch each month. You’ll be surprised.
Patients aren’t just recipients of medication. They’re the final quality check. When they speak up, you catch mistakes no machine ever could. That’s not just good practice. It’s the only way to truly keep people safe.

All Comments
Paul Dixon December 12, 2025
Man, I wish my pharmacist asked me what my meds were for instead of just handing over the bottle like I'm picking up coffee. I once got a blood thinner thinking it was for my knee. Didn't catch it till I nearly passed out on the subway. That 2-minute chat? It's not a luxury-it's a lifeline.
Courtney Blake December 13, 2025
Let’s be real-this whole ‘counseling’ thing is just corporate theater. Pharmacies do it because CMS is watching, not because they care. Most techs read from a script like they’re reading a grocery list. Patients aren’t stupid. They know when you’re just checking a box.
matthew dendle December 13, 2025
83% error catch rate? lol. you mean 83% of errors that were already caught by the barcode system and then the pharmacist just nodded and said 'yep thats right' and moved on. real world isnt a textbook. people dont talk. they just want their pills and leave. you think they gonna explain their whole medical history to a stranger in a white coat? dream on
Lisa Stringfellow December 14, 2025
And yet, every time I go in, they’re already yelling at the next person. The whole system is built to burn out pharmacists so they can’t actually do this. They get paid by the script, not by the lives saved. So yeah, great advice. Now tell me how to get a 2-minute window when the line’s out the door.
Monica Evan December 15, 2025
I work in a rural clinic. We don’t have fancy scanners. We have a whiteboard, a phone, and a pharmacist who remembers everyone’s grandkids’ names. We ask ‘what’s this for?’ and then we listen. One guy came in for his diabetes med-he thought it was for his heart. He’d been taking it wrong for 8 months. We caught it. No tech, no AI. Just a person who cared enough to ask. That’s the magic. Not the protocol. The human.
Mia Kingsley December 15, 2025
Wait wait wait-so you’re saying the solution to 51 million errors is… TALKING? Wow. Groundbreaking. Next you’ll tell us that wearing seatbelts reduces car crashes. I mean, duh. But why is this even a topic? If your job is handing out meds and you’re not verifying with the patient, you shouldn’t be allowed near a pharmacy. Period.
Katherine Liu-Bevan December 16, 2025
The four-step routine is spot-on. But what’s missing is training. Most pharmacy schools don’t teach communication skills like they teach pharmacokinetics. You can’t expect someone to do this well if they’ve never been shown how. Role-playing, feedback loops, empathy mapping-these aren’t fluff. They’re clinical skills.
Kristi Pope December 17, 2025
I’ve seen this work in my mom’s pharmacy. She started doing the full routine on refills after her neighbor had a bad reaction to a new pill color. Now she writes little notes in the script: 'Patient confused about dose-re-explained.' Patients leave with smiles. And guess what? She gets more referrals than anyone else in town. It’s not just safer-it’s better business.
Aman deep December 19, 2025
Coming from India, where pharmacists often double as doctors, this feels familiar. We don’t have the same systems, but we have the same problem-people take meds without understanding. I once saw a man take insulin like it was a vitamin. We stopped him. No scanner, no checklist. Just someone who asked, 'Why are you taking this?' That’s all it takes. Culture matters. Communication matters.
Eddie Bennett December 20, 2025
Big pharma doesn’t want this. Why? Because if patients actually understood their meds, they’d ask more questions. And if they ask more questions, they’d realize how many of these drugs are overprescribed. This whole system is designed to keep people passive. Counseling makes them active. And that’s scary for the machine.
Vivian Amadi December 20, 2025
Stop pretending this is about safety. It’s about liability. If you get sued, you say 'we counseled.' But nobody actually listens. You just read the label and move on. This whole post is a PR stunt dressed up as best practice.
Ariel Nichole December 21, 2025
Love this. My grandma’s pharmacist does this every time. She remembers her meds, her dog’s name, and that she hates grapefruit. That’s the kind of care that keeps people alive. Not scanners. Not apps. People.
john damon December 23, 2025
👏👏👏 this is why I always go to my local pharmacy. The guy there knows my name, my kid’s allergies, and that I hate blue pills. He once caught a 10x overdose because I said 'this looks different.' 💯
Jean Claude de La Ronde December 25, 2025
So we’ve reduced human error by replacing it with procedural error. Now instead of one mistake, we have fifteen checklists that nobody follows because they’re tired, overworked, and emotionally drained. The real problem isn’t the patient not talking-it’s the system making talking impossible.
Sylvia Frenzel December 25, 2025
They don’t want you to know this, but counseling is the only thing keeping pharmacy from becoming a Walmart auto-fill kiosk. If you think this is about patient safety, you’re naive. It’s about survival.