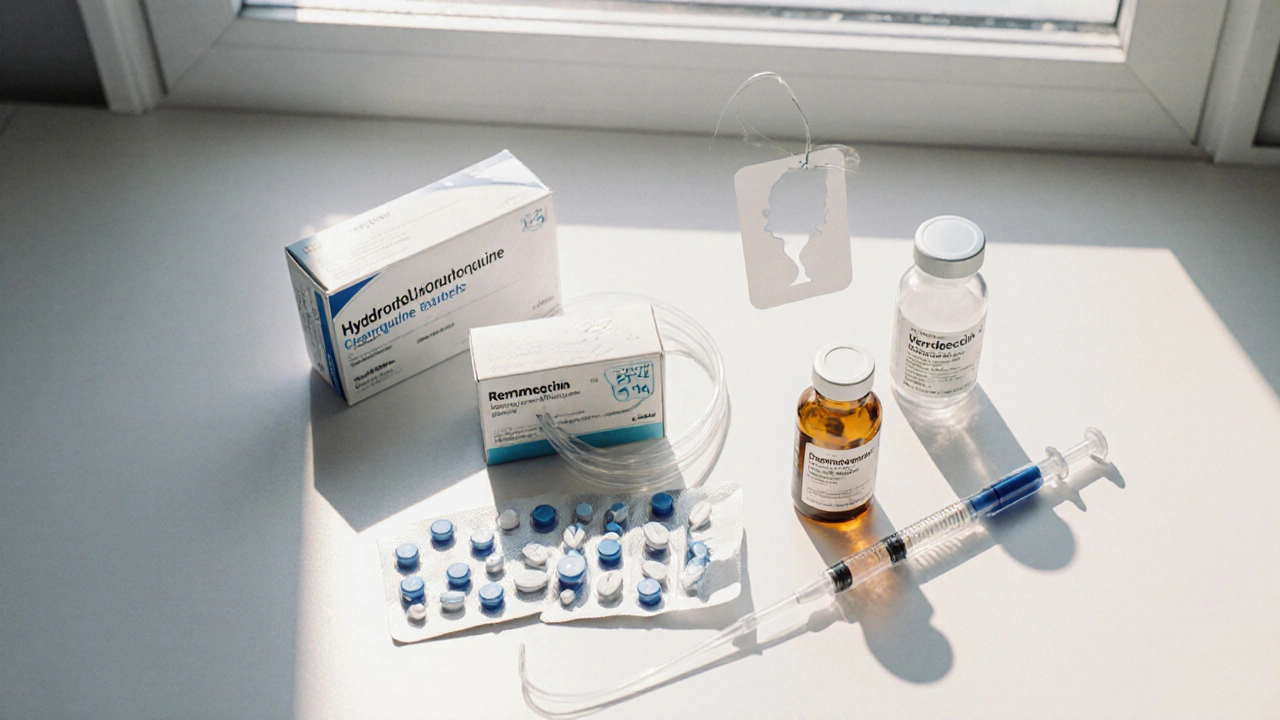
When evaluating treatment options, Hydroxychloroquine is a synthetic antimalarial also used for autoimmune diseases like lupus and rheumatoid arthritis. It surged into the spotlight during the COVID‑19 pandemic, prompting countless headlines and a flood of questions about how it stacks up against other drugs.
Key Takeaways
- Hydroxychloroquine is approved for malaria and certain autoimmune conditions, not for COVID‑19.
- Most alternatives (e.g., remdesivir, ivermectin) have different mechanisms and varying levels of clinical evidence.
- Safety profiles differ markedly: hydroxychloroquine can affect the heart, while remdesivir may impact liver function.
- Cost and accessibility range from inexpensive generic pills to pricey IV formulations.
- Choosing a drug depends on the specific disease, severity, and individual risk factors.
Hydroxychloroquine is often confused with its older cousin chloroquine, but the two are not interchangeable. Below we break down how hydroxychloroquine works, then compare it with the most talked‑about alternatives.
How Hydroxychloroquine Works
The drug interferes with the parasite’s ability to digest hemoglobin, which is why it treats malaria. In autoimmune disorders, it modulates the immune system by dampening cytokine production and reducing the activity of toll‑like receptors. Dosage for malaria typically starts at 800mg on day1, followed by 400mg daily for two days. For rheumatoid arthritis, the usual dose is 200-400mg daily, taken with food to lessen stomach upset.
Common Alternatives and Their Core Traits
When doctors look for substitutes, they consider the disease target, evidence base, and side‑effect profile. The following drugs are the most frequently mentioned alternatives to hydroxychloroquine in recent medical discussions.
Chloroquine is a first‑generation antimalarial that shares a similar chemical backbone with hydroxychloroquine. It was once used for lupus but fell out of favor due to higher toxicity, especially retinal damage.
Ivermectin is a broad‑spectrum antiparasitic approved for river blindness and certain worm infections. Early lab studies hinted at antiviral activity, sparking off‑label use for COVID‑19, though large trials have not confirmed a benefit.
Remdesivir is an RNA‑dependent RNA polymerase inhibitor originally developed for Ebola. It received Emergency Use Authorization for hospitalized COVID‑19 patients after showing modest reductions in recovery time.
Favipiravir is a viral RNA polymerase inhibitor used in Japan for influenza. Some trials in COVID‑19 have reported faster viral clearance, but data remain mixed.
Dexamethasone is a potent glucocorticoid that suppresses inflammation. It is not an antiviral but has saved lives in severe COVID‑19 by curbing the cytokine storm.
Tocilizumab is an IL‑6 receptor antagonist used for rheumatoid arthritis and cytokine release syndrome. It’s sometimes added to severe COVID‑19 protocols when inflammation spikes.
Azithromycin is a macrolide antibiotic with anti‑inflammatory properties. Early COVID‑19 regimens paired it with hydroxychloroquine, but subsequent studies showed no added benefit and highlighted cardiac risks.
Side‑Effect Snapshot
Understanding safety is crucial. Below is a quick guide to the most common adverse events each drug can cause.
- Hydroxychloroquine: QT‑interval prolongation, retinal toxicity (rare with short courses), gastrointestinal upset.
- Chloroquine: Higher risk of cardiac arrhythmia and retinal damage, especially at doses >1g/day.
- Ivermectin: Skin rash, dizziness, rare neurotoxicity at high doses.
- Remdesivir: Elevated liver enzymes, infusion‑related reactions, occasional kidney injury.
- Favipiravir: Elevated uric acid, teratogenic potential, mild liver enzyme rise.
- Dexamethasone: Hyperglycemia, mood swings, increased infection risk with prolonged use.
- Tocilizumab: Upper‑respiratory infections, liver enzyme elevation, neutropenia.
- Azithromycin: QT prolongation (especially with other QT‑prolonging drugs), diarrhea.

Cost and Accessibility Overview
Affordability can dictate real‑world use, especially in low‑resource settings.
- Hydroxychloroquine: Generic oral tablets cost £0.10-£0.30 per pill in the UK.
- Chloroquine: Similar price point to hydroxychloroquine, though availability has decreased.
- Ivermectin: Widely available as a cheap oral formulation; ~£0.20 per tablet.
- Remdesivir: Intravenous therapy costing several thousand pounds per treatment course; often limited to hospital formulary.
- Favipiravir: Not approved in the UK, but where available, price can exceed £100 per course.
- Dexamethasone: Inexpensive steroid, ~£0.05 per tablet.
- Tocilizumab: Expensive monoclonal antibody, £1,200-£1,800 per infusion.
- Azithromycin: Generic tablets cost around £0.15 each.
Comparison Table
| Drug | Primary Mechanism | FDA/EMA Approval (as of 2025) | Typical Indication | COVID‑19 Evidence | Common Side Effects | Cost (UK, per typical course) |
|---|---|---|---|---|---|---|
| Hydroxychloroquine | Alkalinises lysosomes; immunomodulation | Approved for malaria, lupus, RA | Malaria prophylaxis; autoimmune disorders | Large RCTs show no benefit for COVID‑19 | QT prolongation, retinal toxicity (long‑term) | £15‑£30 (10‑day course) |
| Chloroquine | Inhibits heme polymerisation in malaria parasite | Approved for malaria only (few countries) | Uncomplicated malaria | Similar to hydroxychloroquine - no proven benefit | QT prolongation, retinopathy | £12‑£25 (10‑day course) |
| Ivermectin | Glutamate‑gated chloride channel agonist | Approved for parasitic infections | River blindness, strongyloidiasis | Observational data inconclusive; major trials negative | Dizziness, skin rash | £8‑£20 (5‑day course) |
| Remdesivir | RNA‑polymerase inhibitor | Approved for hospitalized COVID‑19 (EU, US) | Severe COVID‑19 | Modest reduction in recovery time; not mortality benefit | Liver enzyme rise, infusion reactions | £3,000‑£5,000 (5‑day IV course) |
| Favipiravir | Viral RNA‑polymerase inhibitor | Approved in Japan for influenza; off‑label elsewhere | Influenza (Japan); investigational COVID‑19 | Mixed results; some early trials positive | Hyperuricemia, teratogenic risk | £100‑£150 (10‑day course) |
| Dexamethasone | Glucocorticoid receptor agonist | Approved for many inflammatory conditions | Severe inflammation, COVID‑19 (hospitalized) | Reduces mortality in ventilated patients | Hyperglycemia, mood changes | £5‑£10 (10‑day oral course) |
| Tocilizumab | IL‑6 receptor blockade | Approved for rheumatoid arthritis, cytokine release syndrome | Severe COVID‑19 with high IL‑6 | Improves outcomes in selected high‑inflammation patients | Infection risk, liver enzyme rise | £1,500‑£1,800 (single infusion) |
| Azithromycin | Protein synthesis inhibitor (macrolide) | Approved for bacterial infections | Respiratory bacterial infections | No proven antiviral benefit; combined trials negative | QT prolongation, GI upset | £12‑£20 (5‑day course) |
When to Choose Hydroxychloroquine Over Alternatives
If a patient already has a prescription for lupus or rheumatoid arthritis, hydroxychloroquine remains the drug of choice for disease control. Its oral form, low cost, and long safety record for chronic use make it hard to replace in these contexts. However, for acute viral infections or hospitalized COVID‑19 cases, the evidence points to other agents-remdesivir for early hospitalization, dexamethasone for patients needing oxygen, and tocilizumab for those with a cytokine surge.
Decision Checklist for Clinicians and Patients
- Identify the primary condition. Autoimmune disease → hydroxychloroquine; severe COVID‑19 → dexamethasone ± tocilizumab.
- Check regulatory status. Is the drug approved for the indication in your country?
- Assess cardiac risk. Review ECG for QT interval; avoid hydroxychloroquine or azithromycin if QT >450ms.
- Review liver and kidney function. Remdesivir and favipiravir need normal labs.
- Consider cost and administration route. Oral cheap drugs suit outpatient care; IV expensive drugs need hospital setting.
Frequently Asked Questions
Frequently Asked Questions
Is hydroxychloroquine effective for preventing COVID‑19?
Large randomized trials have consistently shown no protective benefit. Health agencies worldwide recommend against using it for COVID‑19 prophylaxis.
Can I take hydroxychloroquine and azithromycin together?
Both drugs can prolong the QT interval, increasing the risk of serious heart rhythm problems. Unless a doctor monitors your heart closely, the combination is generally discouraged.
What are the main side effects of remdesivir?
Patients may experience elevated liver enzymes, nausea, and occasional infusion‑related reactions. Kidney function should be checked before starting.
Is ivermectin safe for COVID‑19 treatment?
When used at approved doses for parasitic infections, ivermectin is safe. However, doses used in some COVID‑19 trials exceed approved levels and have caused neurotoxicity. Major health bodies advise against its use for COVID‑19.
When should dexamethasone be given to COVID‑19 patients?
Dexamethasone benefits patients who need supplemental oxygen or mechanical ventilation. Giving it too early, before oxygen is required, does not improve outcomes and may suppress viral clearance.
Bottom line: hydroxychloroquine remains a valuable drug for specific chronic conditions, but for acute viral illnesses-especially COVID‑19-other agents have clearer evidence or better safety. Always discuss with a healthcare professional before switching or combining medications.
All Comments
Ramanathan Valliyappa October 12, 2025
Hydroxychloroquine's cardiac risk is overstated by hype, but the data still show QT prolongation in susceptible patients.
lucy kindseth October 20, 2025
Hey folks, here's a quick rundown: hydroxychloroquine is cheap and works well for lupus, but it hasn't shown any benefit for COVID‑19. The alternatives like remdesivir or dexamethasone have stronger evidence in hospitalized patients, though they can be pricey or require IV infusion. Always match the drug to the disease and the patient's risk profile.
Nymia Jones October 28, 2025
It must be underscored, dear readers, that the prevailing narrative surrounding hydroxychloroquine is, in my view, a calculated orchestration by clandestine pharmaceutical conglomerates seeking to divert scrutiny from their own experimental biologics. The suppression of dissenting data, I contend, is not merely an oversight but a deliberate stratagem. Consequently, any recommendation lacking transparent peer review warrants profound skepticism. One must therefore uphold the highest standards of epistemic vigilance.
Karen McCormack November 5, 2025
One could argue that such alarmism itself mirrors the very dogma it purports to dismantle, for in the labyrinth of modern medicine, the quest for certainty often begets new forms of certainty. The epistemic humility we seek is eclipsed by the echo chamber of authority, where dissent is branded as heresy. Yet, paradoxically, it is within this crucible of contested truths that genuine progress is forged. Perhaps the true antidote lies not in vilifying a single molecule, but in cultivating a pluralistic discourse that honors both data and dissent.
Earl Hutchins November 13, 2025
When choosing a therapy, start with the indication: lupus or rheumatoid arthritis? Then check cardiac history – hydroxychloroquine can prolong QT. If the patient needs a fast‑acting antiviral, remdesivir may be better but watch liver enzymes. Cost and administration route also matter.
Tony Bayard November 21, 2025
Reading the data can feel like navigating a stormy sea, but take heart – you’re not alone in this voyage. If your loved one is battling an autoimmune flare, hydroxychloroquine remains a reliable anchor, provided the heart is monitored. For severe COVID‑19, the tide turns toward dexamethasone and, when inflammation spikes, tocilizumab. Never hesitate to ask your clinician about side‑effect profiles; informed decisions are the clearest compass.
Jay Crowley November 29, 2025
Hydroxychloroquine’s retinal risk is rare with short courses.
sharon rider December 6, 2025
From a global health perspective, accessibility often dictates real‑world usage; a cheap oral pill can save more lives in low‑resource settings than an expensive IV drug.
joba alex December 14, 2025
Sure, the "evidence" says hydroxychloroquin is junk for Covid, but let's not ignore the pharmacokineic nuances that some "mainstream" papers omitt. The metabolite pathways are complex, and dismissing them outright is a simplistic reductiionism. In short, keep an open mind.
Rene Lacey December 22, 2025
The philosophical underpinnings of medical decision‑making beckon us to examine not just the biochemical mechanisms but the very nature of truth itself. When a drug like hydroxychloroquine becomes a cultural flashpoint, it forces clinicians to confront the limits of evidence and the sway of public opinion. We must ask whether efficacy should be measured solely by randomized trials or also by lived patient experiences. Moreover, the ethical dimension of prescribing a medication with known cardiac risks, albeit rare, cannot be ignored. As we weigh cost against benefit, the socioeconomic context of the patient emerges as a crucial variable. Ultimately, the art of medicine resides in balancing rigorous data with compassionate judgment, a synthesis that transcends mere numbers.
johnson mose December 30, 2025
The stakes are high, and every prescription feels like a moral crossroads. Yet, remember that science evolves, and today's consensus may be tomorrow's footnote. Keep the dialogue alive, and let compassion guide the pen.
Charmaine De Castro January 7, 2026
Great summary! Just a quick tip: always double‑check the latest dosing guidelines, as they can shift with new trial data.
Mark Mendoza January 15, 2026
👍 Absolutely, staying updated is key. 📚💊
Dan Tourangeau January 23, 2026
In practice, I find the cost‑benefit analysis simplifies the choice for many patients.
Bernard Valentinetti January 31, 2026
Ah, the sweet symphony of pharmacoeconomics, where every penny sings a tale of access, efficacy, and-let us not forget-those ever‑present bureaucratic hurdles! 😂 Yet, when we speak of hydroxychloroquine, we must also invoke the grand tapestry of immunomodulation, a topic that simply cannot be reduced to mere spreadsheets. So, dear colleagues, let us toast to nuanced discussions, tempered with a dash of humor! 🍷📈
Kenneth Obukwelu February 7, 2026
When we weave together perspectives from pharmacology, economics, and patient stories, the narrative becomes richer than any single study alone could convey. This collaborative spirit is what drives innovation in treatment pathways. Let us champion open dialogue and shared wisdom as we navigate these complex choices.
Josephine hellen February 15, 2026
Choosing the right medication can feel daunting, but remember that every patient’s journey is unique and full of potential. Hydroxychloroquine has stood the test of time for autoimmune conditions, offering a stable, affordable option for many. When paired with careful cardiac monitoring, its risks are manageable and often outweighed by its benefits. Meanwhile, newer agents like remdesivir or tocilizumab provide powerful tools for acute viral inflammation, especially in hospital settings. Their higher costs and IV administration mean they are best reserved for those who truly need that level of intervention. Cost‑effectiveness analyses consistently show that oral, inexpensive drugs can dramatically improve outcomes in low‑resource environments. This underscores the importance of tailoring therapy not just to disease severity but also to socioeconomic context. Clinicians who stay abreast of evolving guidelines empower patients to make informed choices. Open communication about side‑effects, monitoring plans, and alternative options builds trust and adherence. Even if a drug like hydroxychloroquine isn’t the hero for COVID‑19, it remains a cornerstone for lupus and rheumatoid arthritis. Patients on stable regimens often report better quality of life than those constantly switching medications. Thus, continuity of care, combined with periodic reassessment, can prevent unnecessary complications. Remember, the ultimate goal is to reduce disease burden while preserving dignity and financial stability. With a collaborative approach involving doctors, pharmacists, and patients, the best therapeutic path emerges naturally. Stay hopeful, stay informed, and trust that the medical community is continuously working to refine these options for everyone’s benefit.