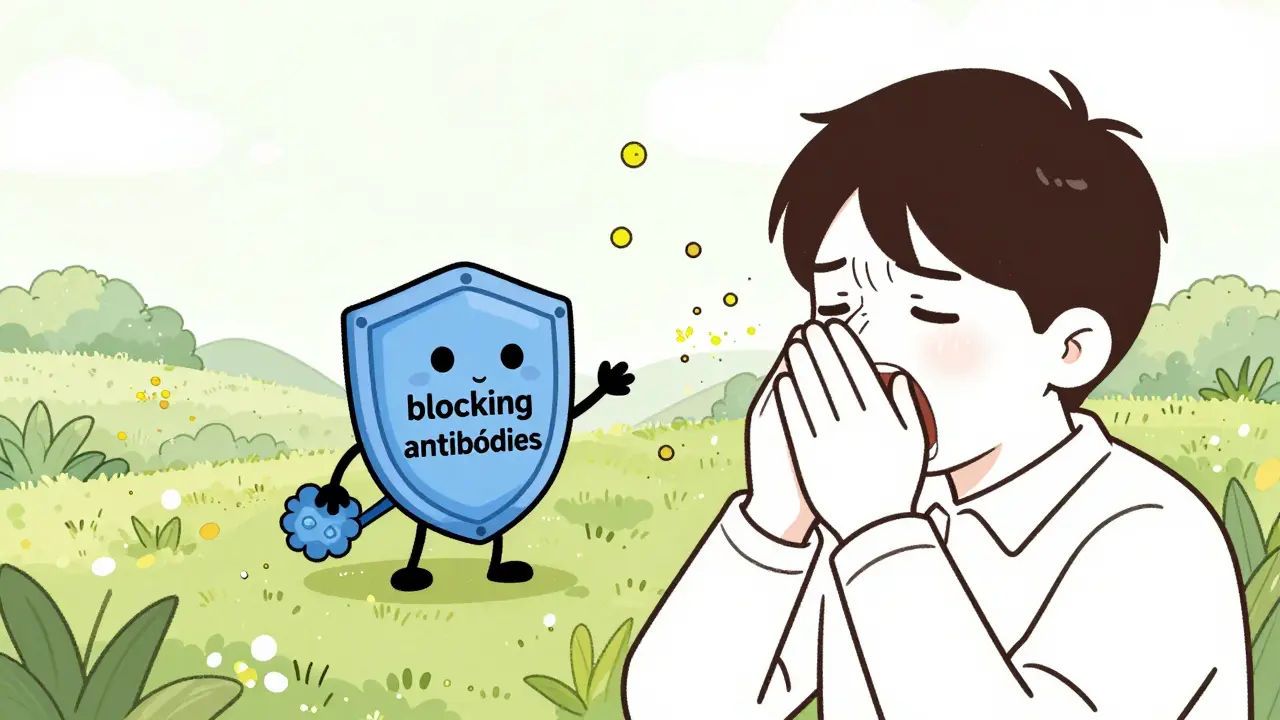
When your allergies turn spring into a nightmare-sneezing nonstop, eyes watering, nose clogged-you’ve probably tried antihistamines, nasal sprays, and air filters. But what if there’s a way to stop the reaction at its source? That’s where immunotherapy comes in. Unlike medications that just mask symptoms, immunotherapy trains your immune system to stop overreacting to allergens like pollen, dust mites, or bee venom. It’s not a quick fix. It’s a multi-year commitment. But for many, it’s the only thing that brings real, lasting relief.
How Immunotherapy Actually Works
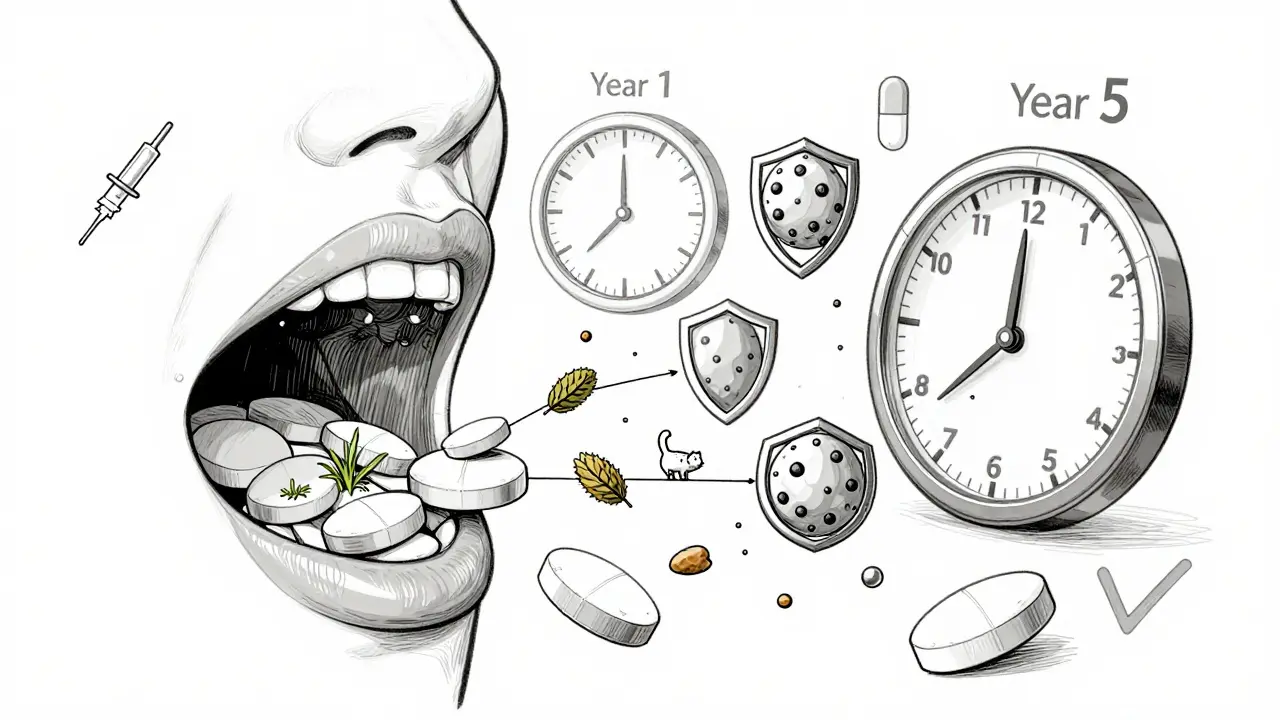
Immunotherapy doesn’t suppress your immune system-it reprograms it. Think of it like a vaccine, but for allergies. You’re exposed to tiny, controlled amounts of the things you’re allergic to. Over time, your body learns these aren’t threats. Instead of releasing histamine and causing inflammation, your immune system starts producing blocking antibodies. These antibodies act like shields, stopping allergens from triggering a full-blown reaction.
This isn’t new. The first allergy shots were given in London in 1911. Since then, science has refined the process, but the core idea stays the same: gradual exposure leads to tolerance. The goal? To reduce or even eliminate symptoms so you don’t need daily meds. Studies show that after 3 to 5 years of treatment, up to 85% of patients see major improvements. Some stay symptom-free for years after stopping treatment.
Allergy Shots: The Gold Standard
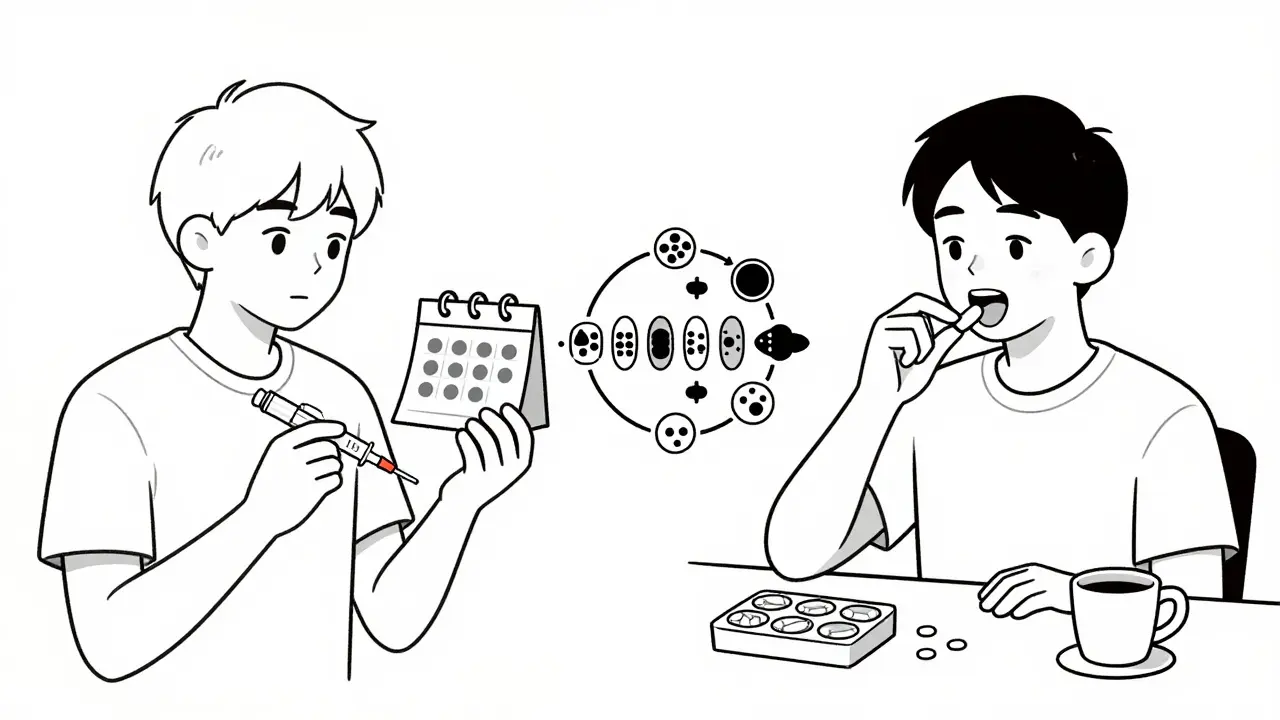
Allergy shots, or subcutaneous immunotherapy (SCIT), are still the most effective option. They’re custom-made for you. Your allergist tests you for sensitivities-maybe to ragweed, grass, dust mites, and cat dander-and creates a unique vial with those exact allergens. Each shot contains a tiny amount of each one. Over time, the dose increases.
The process has two phases. First, the build-up phase. You get shots once or twice a week for several months. This can take 3 to 12 months depending on your schedule. Then comes maintenance: you switch to monthly shots for 3 to 5 years. Each visit requires a 30-minute wait after the shot to watch for reactions. It’s inconvenient, yes. But the results? Powerful.
Why? Because allergy shots can handle multiple allergens at once. Most people are allergic to more than one thing. Research shows 78% of allergy sufferers react to three or more allergens. Shots can cover all of them in one vial. A 2021 study found SCIT reduced symptoms by 82% in multi-allergen patients. That’s higher than any tablet can achieve.
Doctors at the Cleveland Clinic and National Jewish Health agree: if you have multiple allergies or severe symptoms, shots are the best bet. They’re also the only treatment proven to prevent new allergies from developing and to reduce the risk of asthma in kids with allergic rhinitis.
Sublingual Tablets: Convenience Without Compromise?
Sublingual immunotherapy (SLIT) tablets are the newer, easier option. You place a small tablet under your tongue every day. No needles. No clinic visits. You can do it while brushing your teeth or eating breakfast.
The FDA has approved four tablets so far: Oralair and Grastek for grass pollen, Ragwitek for ragweed, and Odactra for dust mites. In April 2024, Cat-PAD became the first tablet approved for cat dander. That’s progress. But here’s the catch: each tablet covers exactly one allergen. No combinations. No custom mixes.
If you’re allergic to grass and dust mites? You’d need two tablets. One in the morning. One at night. That’s two daily doses. Two different bottles. Two chances to forget. And even then, you’re only treating two of the allergens you might react to.
Studies show SLIT tablets reduce symptoms by about 67% in single-allergen cases. That’s good-but not as good as shots. A 2022 patient survey found 58% of tablet users reported limited effectiveness, especially if they had multiple allergies. On Reddit, users who tried both often say shots worked better. One wrote: “After two years of Grastek with only 30% improvement, I switched to shots and got 80% relief by year two.”
But convenience matters. In the same survey, 92% of tablet users said they preferred it over weekly shots. For busy parents, travelers, or people without easy access to an allergist, that’s huge. Tablets also have fewer serious side effects. The most common? A tingling or itching under the tongue. Rarely, swelling or stomach upset. Severe reactions are extremely rare.
Which One Is Right for You?
There’s no one-size-fits-all answer. But here’s how to decide:
- Choose allergy shots if: You’re allergic to three or more allergens, your symptoms are severe, you want the strongest possible effect, or you’re trying to prevent asthma. You’re willing to commit to weekly visits for months, then monthly for years.
- Choose sublingual tablets if: You’re allergic to just one or two allergens (like grass or dust mites), you travel often, you hate needles, or you can’t find a clinic nearby. You’re okay with daily pills and slightly less dramatic results.
There’s also a middle ground: cluster immunotherapy. Instead of spreading build-up over months, you get several shots in one day, over 4 to 10 visits. This cuts the build-up phase from 6 months to under 2 months. It’s becoming more common-74% of clinics now offer it. It’s still shots, but faster.
Rush immunotherapy is another option-for people with life-threatening insect sting allergies. You get multiple doses in one 8-hour session. It’s intense. It carries higher risk. But for those who’ve been stung and nearly died, it’s worth it.
What to Expect During Treatment
With shots, you’ll need to plan your week. You can’t skip appointments. If you miss one, you might need to repeat the last dose. Side effects are usually mild: redness, swelling at the injection site. About 2% of people have a systemic reaction-hives, trouble breathing. That’s why you wait 30 minutes after every shot. Clinics are equipped to handle it.
With tablets, you take one daily. The first dose must be taken in a doctor’s office, just in case. After that, it’s home-based. You’ll feel a tingling under your tongue for the first few days. That’s normal. If you get swelling in your throat, trouble breathing, or vomiting, stop the tablet and call your doctor. That’s rare, but serious.
Adherence is everything with tablets. If you miss more than 20% of doses, the treatment fails. A 2021 trial showed effectiveness dropped to 45% in low-adherence patients. Set phone reminders. Keep tablets in your pill organizer. Don’t skip days.
Cost, Access, and Future Trends
Insurance usually covers both shots and tablets. But shots often cost more upfront because of clinic visits. Tablets are pricier per month, but you pay less for office time. In the U.S., shots make up 68% of the immunotherapy market. Tablets are growing fast-up to 27% now.
Access is still a problem. There are only about 5,300 board-certified allergists in the U.S. Many rural areas have none. That’s why tablets are gaining ground-even if they’re less effective for complex cases.
The future? Multi-allergen tablets are in Phase 3 trials. If approved by 2025, they could change everything. So could peptide-based therapies, which might shorten treatment from 5 years to 2. Doctors are also using component-resolved diagnostics to match allergens more precisely, making treatments smarter.
For now, the choice comes down to your life, your allergies, and your priorities. Shots are the strongest tool. Tablets are the easiest. Neither is perfect. But both are better than just living with sneezing every spring.
Is Immunotherapy Worth It?
Let’s say you spend $500 a year on allergy meds. That’s $2,500 over five years. Add up missed workdays, ruined weekends, sleepless nights. Now imagine cutting those symptoms by 80%. You’re not just saving money-you’re getting your life back.
People who stick with immunotherapy often say the same thing: “I wish I’d started sooner.”
Are allergy shots painful?
The needles used are very small, similar to a flu shot. Most people feel just a quick pinch. The discomfort is minor compared to the relief they get later. Swelling or redness at the injection site is common but usually fades within hours.
Can children get immunotherapy?
Yes. Children as young as 5 can receive allergy shots. Sublingual tablets are approved for kids 10 and older. Immunotherapy is especially helpful for kids with allergic rhinitis because it can reduce the risk of developing asthma later.
How long until I see results from immunotherapy?
Most people start noticing improvements after 6 to 12 months. Some feel better sooner. But full benefits usually take 2 to 3 years. Don’t expect instant relief. This is a long-term change, not a quick fix.
Do I have to take immunotherapy forever?
No. The standard course is 3 to 5 years. After that, most people stop treatment. Many stay symptom-free for years, even decades. Some may need a booster if symptoms return, but most don’t.
Can I switch from tablets to shots if tablets don’t work?
Yes. Many people start with tablets for convenience and switch to shots if they’re not getting enough relief. There’s no harm in switching. Your allergist will adjust your treatment plan based on your progress and needs.
Next Steps
If you’re tired of living with allergies, talk to an allergist. Ask about testing to find out exactly what you’re allergic to. Then ask about both options-shots and tablets. Don’t assume one is better just because it’s newer or easier. Your allergies are unique. Your treatment should be too.
Start with a consultation. Bring your symptom history. List what triggers you. Ask about cluster build-up if you want to speed things up. And don’t be afraid to ask about cost, insurance, and what happens if you miss a dose. The right treatment can turn your worst season into your easiest one.
All Comments
RAJAT KD January 8, 2026
Been on shots for 4 years. No more antihistamines. No more sleepless nights. Worth every minute.
Catherine Scutt January 8, 2026
Ugh, I tried the tablet for ragweed. Tasted like chalk and did nothing. Shot person here - don’t waste your time with tablets if you’re serious.
Darren McGuff January 10, 2026
As an allergist in London, I’ve seen this play out for 20+ years. The data’s clear: SCIT has superior long-term efficacy, especially for polysensitized patients. SLIT is convenient, yes - but it’s like using a bandaid on a broken leg. The immune modulation from subcutaneous exposure is just deeper, more durable. Don’t confuse ease with effectiveness. And yes, cluster protocols are game-changers - cuts the build-up phase by 70% without sacrificing safety.
Jeffrey Hu January 10, 2026
Everyone’s acting like this is some revolutionary breakthrough. Newsflash: immunotherapy’s been around since 1911. What’s new is the marketing. The real issue? Access. Most people can’t afford the time or money for shots, so they’re sold on tablets as the ‘modern’ solution. It’s capitalism disguised as progress. Also, 85% improvement? That’s not universal - it’s averaged across a population. My cousin did 5 years of shots and still sneezes in October. Don’t believe the hype.
Drew Pearlman January 10, 2026
I know it sounds like a huge commitment, but trust me - if you’ve been stuck in this cycle of sneezing, itchy eyes, and feeling like you’re constantly fighting your own body, this is the one thing that actually gives you your life back. I started shots when I was 28, was on Zyrtec daily, missed work, couldn’t go hiking - now I’m 34, I haven’t taken an antihistamine in over a year, and I just went on a 3-day camping trip in the woods with zero symptoms. It’s not magic, but it’s the closest thing we’ve got. The first year is rough, but the payoff? Life-changing. You’ll look back and wonder why you waited so long.
Chris Kauwe January 12, 2026
Let’s deconstruct the efficacy metrics here. The 82% reduction in multi-allergen patients? That’s from a retrospective cohort with selection bias - those who stick with shots are inherently more compliant and motivated. SLIT adherence rates are abysmal - 40% drop out by month 6. And let’s not pretend the 67% SLIT efficacy is comparable. It’s not. The immune tolerance curve from sublingual dosing is shallower, less sustained. Plus, the FDA-approved tablets are all monovalent - they’re not even designed for real-world polyallergen profiles. We’re optimizing for convenience, not immunological fidelity. The future’s in peptide-based desensitization - targeted epitope modulation without whole allergen exposure. That’s the real frontier.
Phil Kemling January 12, 2026
It’s funny how we treat allergies like a problem to be solved, rather than a symptom of a system out of balance. We inject or dissolve allergens to ‘train’ the immune system - but what if the immune system isn’t broken? What if it’s just reacting to a world full of synthetic chemicals, depleted microbiomes, and chronic stress? Maybe we’re not reprogramming immunity - we’re just numbing its signal. The real cure might be in soil, sleep, and silence - not vials or tablets.
Elisha Muwanga January 12, 2026
Look, I get that some people like their convenience, but this country’s falling apart because we’ve normalized mediocrity. Shots are the gold standard - period. If you can’t commit to a weekly visit, maybe you’re not serious about your health. Tablets are for people who want to feel like they’re doing something without actually doing anything. This isn’t a subscription service - it’s medicine. Get your act together.
Aron Veldhuizen January 13, 2026
You’re all missing the point. Immunotherapy doesn’t cure allergies - it just teaches your body to tolerate the very things that are poisoning your environment. That’s not healing - that’s surrender. Why not fix the air? Why not ban glyphosate-laced pollen? Why not regulate indoor mold exposure? We’re not treating the cause - we’re treating the symptom of a broken world. And now we’re monetizing it with multi-year treatment plans. The real question isn’t shots vs tablets - it’s why we’ve allowed our ecosystems to become so toxic that we need to inject our own allergens into our skin just to survive.