For years, cancer treatment meant surgery, radiation, or chemotherapy-harsh, blunt tools that attacked the body as much as the disease. But since 2011, a quiet revolution has been unfolding. Checkpoint inhibitors and CAR-T cell therapy are two of the most powerful tools in this new era: they don’t poison cancer. They teach the body’s own immune system to find and kill it.
How Checkpoint Inhibitors Work
Your immune system has built-in brakes. That’s a good thing-it stops your body from attacking itself. But cancer learned how to flip those brakes on. Tumors coat themselves in proteins like PD-L1, which latch onto PD-1 receptors on T cells, telling them: "You’re safe. Don’t attack." Checkpoint inhibitors are monoclonal antibodies that block this signal. Drugs like pembrolizumab (Keytruda) and nivolumab (Opdivo) block PD-1. Ipilimumab (Yervoy) blocks CTLA-4. Once those brakes are released, T cells wake up and start hunting cancer cells again. This isn’t magic. Only 20-40% of patients respond, and it depends heavily on the cancer type. Melanoma, lung cancer, and kidney cancer often respond well. But in many tumors, especially solid ones like pancreatic or ovarian, the immune system still can’t find the cancer-even with the brakes off. Why? The tumor microenvironment is hostile. It’s full of suppressive cells, low oxygen, and chemical barriers that shut down T cells before they even get close.CAR-T Therapy: Engineering Your Own Soldiers
CAR-T therapy takes a completely different route. Instead of removing brakes, it builds a new army. First, doctors take a sample of your blood and pull out your T cells. These are sent to a lab, where they’re genetically modified using a virus to add a synthetic receptor: the chimeric antigen receptor (CAR). This CAR is designed to recognize one specific protein on cancer cells-like CD19 on B-cell leukemias. The modified T cells are grown in big bioreactors until there are hundreds of millions. Then, after you get a round of chemo to clear space in your bone marrow, they’re infused back into you. These engineered cells don’t just attack-they multiply inside your body. Some patients see complete remission where nothing else worked. In kids with relapsed acute lymphoblastic leukemia (ALL), CAR-T therapy achieves remission in 60-90% of cases. That’s unheard of in advanced cancer. But it only works for blood cancers so far. In solid tumors, CAR-T cells struggle to get inside, get tired quickly, or get shut down by the same immune-suppressing signals that block checkpoint inhibitors.Side Effects: The Price of Activation
Both therapies come with serious risks. Checkpoint inhibitors can trigger autoimmune reactions. Your immune system, no longer restrained, may attack your thyroid (causing fatigue and weight gain), your colon (leading to severe diarrhea), or your lungs (causing pneumonitis). About 30-40% of patients get a rash. Around 10% develop colitis. These side effects are manageable-if caught early. CAR-T therapy is more intense. Nearly half of patients develop cytokine release syndrome (CRS). That’s when the engineered T cells go wild, flooding the body with inflammatory signals. Symptoms: high fever, low blood pressure, trouble breathing. In 20-40% of cases, patients get neurotoxicity too-confusion, seizures, trouble speaking. This is called ICANS. It’s scary, but most patients recover with the right care. Both therapies cause fatigue and fever. But CAR-T side effects hit harder, faster, and need hospital-level monitoring. That’s why only specialized centers can give it.
Why CAR-T Is So Hard to Access
CAR-T therapy isn’t just expensive-it’s complicated. Each dose is custom-made. It takes 3 to 5 weeks to grow your cells. During that time, your cancer might keep growing. The cost? Between $373,000 and $475,000 per treatment. Insurance covers it, but getting approval can take months. And access isn’t equal. A 2020 review found Black patients were 31% less likely to get CAR-T than white patients. Medicaid patients were 23% less likely. Only 15% of U.S. cancer centers offer CAR-T, but they handle 87% of all treatments. Rural patients often can’t travel. Even if they qualify, they might not make it in time. Checkpoint inhibitors? They’re pills or IV infusions. Available in most oncology clinics. Much easier to get.The Future: Combining the Two
The smartest move isn’t choosing one or the other-it’s using them together. Imagine CAR-T cells that don’t just hunt cancer, but also fight back against the tumor’s defenses. Researchers are now engineering CAR-T cells to produce their own checkpoint-blocking proteins right inside the tumor. These "armored" CAR-T cells secrete anti-PD-1 antibodies locally. That means the immune boost happens where it’s needed-without flooding the whole body and causing dangerous side effects. In mouse studies, this approach cut immune pneumonitis by 42% and improved tumor killing. It’s like giving your T cells a built-in shield and a weapon. Other tricks are coming too. Scientists are testing CAR-T cells that release IL-12 to attract more immune cells, or that target multiple cancer proteins at once. There’s even work on "off-the-shelf" CAR-T from healthy donors-bypassing the wait and cost of personalized therapy. The goal? Make these treatments work for solid tumors. Right now, only 10% of patients with lung, breast, or colon cancer respond to CAR-T. But with smarter designs and smarter combinations, that number could rise.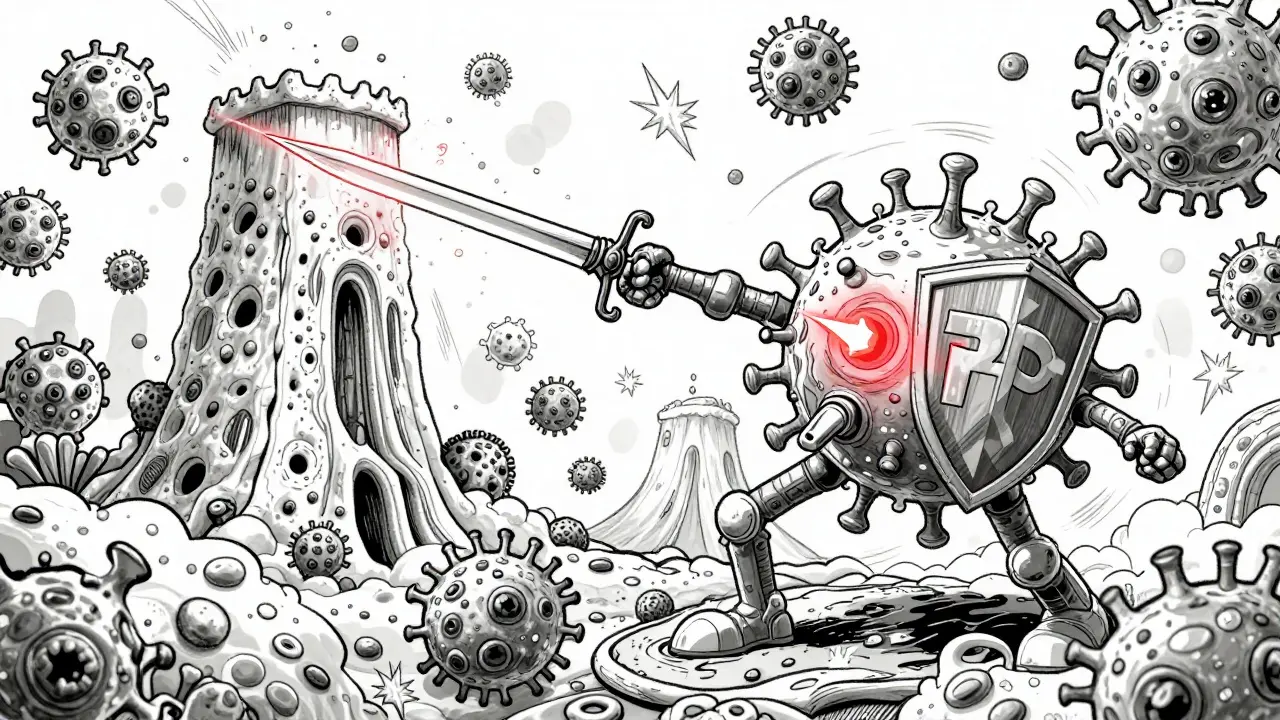
What’s Holding Back Progress?
The biggest roadblock isn’t science-it’s biology. Solid tumors are surrounded by a fortress: fibrous tissue, suppressive immune cells, low oxygen, and signals that exhaust T cells. Even the best CAR-T cells get tired. Even the strongest checkpoint inhibitors can’t wake up immune cells that aren’t there. That’s why the next breakthroughs aren’t just about better drugs. They’re about understanding the tumor’s environment. Researchers are now looking at proteins like PTP1B, an internal brake inside T cells. Blocking it in mice boosted CAR-T effectiveness by 2.3 times. We’re also learning why some patients respond and others don’t. It’s not just about the cancer. It’s about your genetics, your gut bacteria, your previous treatments. One patient might respond to PD-1 blockers. Another won’t-even if their tumor looks identical under a microscope.Where We Are in 2026
By 2026, checkpoint inhibitors are standard care for many cancers. They’re not perfect, but they’ve turned terminal diagnoses into chronic conditions for some. CAR-T therapy is still rare. But it’s no longer experimental. It’s a lifeline for kids with leukemia and adults with certain lymphomas. The market for it is growing faster than any other cancer treatment-projected to hit $30 billion by 2030. The real promise? The combination. Clinical trials as of early 2024 show 47 active studies mixing CAR-T with checkpoint inhibitors. Two-thirds of them are targeting solid tumors. That’s where the biggest unmet need is. We’re not there yet. But for the first time, we’re seeing a path forward-not just for one type of cancer, but for many. The immune system isn’t just a defense. It’s a precision weapon. And we’re finally learning how to use it.What’s the difference between checkpoint inhibitors and CAR-T therapy?
Checkpoint inhibitors are drugs that block signals cancer uses to hide from your immune system. They’re given as IV infusions and work on any T cell in your body. CAR-T therapy takes your own T cells, changes them in a lab to target cancer, and puts them back. It’s personalized, one-time treatment designed to hunt specific tumors.
Which cancers respond best to checkpoint inhibitors?
Melanoma, non-small cell lung cancer, kidney cancer, and some types of head and neck cancers respond best. Response rates are higher when tumors have lots of mutations or express PD-L1. But even in these cancers, only about 20-40% of patients benefit long-term.
Why doesn’t CAR-T therapy work for solid tumors yet?
Solid tumors create a hostile environment. They’re surrounded by physical barriers, suppressive cells, and chemicals that shut down T cells. CAR-T cells can’t get inside easily, get exhausted quickly, or get blocked by the same signals that stop natural T cells. Researchers are now engineering CAR-T cells to fight back against this environment.
Are the side effects of CAR-T worse than checkpoint inhibitors?
Yes, often. Checkpoint inhibitors can cause autoimmune issues like thyroid problems or colitis, which are serious but usually manageable. CAR-T therapy commonly causes cytokine release syndrome (CRS) and neurotoxicity (ICANS), which can be life-threatening. Both require expert care, but CAR-T side effects come faster and need hospital-level monitoring.
Is immunotherapy available everywhere?
Checkpoint inhibitors are widely available in most cancer centers. CAR-T therapy is not. Only specialized centers with trained staff can deliver it. Access is also unequal-Black and Medicaid patients are significantly less likely to receive CAR-T, even when eligible. Cost and manufacturing delays add to the barrier.
What’s the future of these therapies?
The future is combination. Engineering CAR-T cells to release checkpoint blockers right at the tumor site reduces side effects and boosts effectiveness. Other advances include "off-the-shelf" CAR-T from donor cells, targeting new proteins like LAG-3, and using drugs to block internal immune brakes like PTP1B. The goal is to make these treatments work for more cancer types, especially solid tumors.
All Comments
Matthew Morales February 4, 2026
this is wild tbh i had no idea our own cells could be turned into cancer hunters 😮
just read about a buddy who got CAR-T for lymphoma and he’s been in remission for 2 years. like… science fiction becoming real.
Diana Phe February 6, 2026
they’re lying about this. the real reason immunotherapy works is because Big Pharma injected nanobots to control your immune system. they don’t want you to know the truth. #cancerisabusiness
Carl Crista February 6, 2026
checkpoint inhibitors dont work for most people and everyone acts like its magic when the data says otherwise
Andre Shaw February 6, 2026
oh please. CAR-T is just the pharmaceutical industry’s glittery new toy to charge $500k for a glorified gene hack. Meanwhile, real cures like vitamin C infusions and ozone therapy are buried under FDA red tape. They don’t want cheap. They want profitable. And you’re the profit.
Dr. Sara Harowitz February 7, 2026
I’ve reviewed over 300 clinical trials. The data is clear: immunotherapy is a band-aid on a bullet wound. You're not curing cancer-you're delaying death while bankrupting families. And don't get me started on the racial disparities. This isn't progress. It's exploitation dressed in white coats.
Joyce cuypers February 8, 2026
i just want to say to anyone going through this: you're not alone. i watched my mom do this and even on the rough days, she said it felt like she had a fighting chance. keep going. you're stronger than you think 💪❤️
Georgeana Chantie February 10, 2026
why is it always the rich who get the cool new treatments? 🤡 we all know the system is rigged. they’ll make a pill that cures cancer… then charge $1 million for it. and say it’s "research costs". lol
Carol Woulfe February 11, 2026
The notion that these therapies represent a "revolution" is profoundly misleading. The underlying biology remains insufficiently understood, and the clinical outcomes are statistically marginal when applied to the broader oncological population. One must consider the opportunity cost of diverting resources toward such high-cost, low-yield interventions while basic immunological research languishes for funding.
Kieran Griffiths February 11, 2026
I’ve worked in oncology for 18 years. What’s exciting here isn’t just the tech-it’s the shift in mindset. We’re not just killing cells anymore. We’re teaching the body to fight. And yeah, it’s expensive. And yeah, access is messed up. But this? This is the first time we’ve had real hope for solid tumors. Don’t let the noise drown out the progress. We’re still learning. But we’re learning fast.