When a patient in intensive care needs a life-saving shot of epinephrine or a dose of chemotherapy, they don’t get a warning. They don’t get a substitute from the shelf. And increasingly, they don’t get the medicine at all. Hospital pharmacies are the last line of defense in the U.S. drug supply chain-and they’re running out of options. While community pharmacies might see a few missing pills on the shelf, hospital pharmacies are dealing with entire classes of critical injectable drugs vanishing for months, sometimes years. This isn’t a temporary hiccup. It’s a systemic collapse, and the people paying the price are the sickest patients in the country.
Why Injectables Are the First to Go
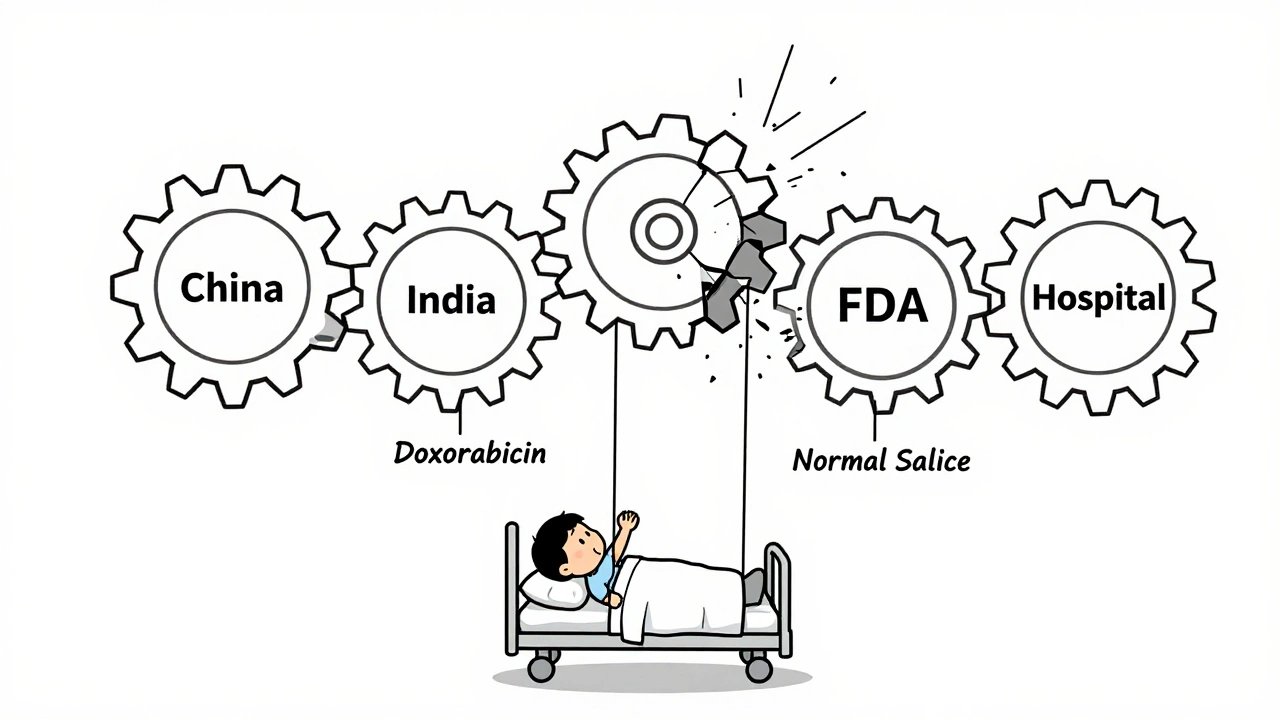
Not all drugs are created equal when it comes to supply risk. Sterile injectables-medicines you get through an IV or injection-are the most vulnerable. Why? Because making them is complicated, expensive, and low-margin. Unlike pills you swallow, injectables must be produced in sterile environments. One speck of dust, one flawed seal, one temperature spike during shipping, and the entire batch is destroyed. That’s why 55% of all drug shortages stem from manufacturing quality issues, according to FDA data analyzed by the National Association of Boards of Pharmacy. The problem gets worse because most of the active ingredients for these injectables come from just two countries: China and India. Eighty percent of the raw materials are sourced there. When a tornado hits a Pfizer plant in North Carolina, or when the FDA shuts down a facility in India over contamination, the ripple effect is immediate. In February 2024, a single quality issue halted production of cisplatin, a key chemotherapy drug. Hospitals across the country scrambled. Patients waited. Some treatments were delayed or changed. And these aren’t rare events. In 2024, 89% of the drug shortages were carryovers from 2023. That means the same drugs-like normal saline, potassium chloride, and anesthetics-were still missing over a year later. These aren’t new problems. They’re old ones that never got fixed.Hospital Pharmacies Are Hit Harder Than Anywhere Else
Retail pharmacies might lose 15-20% of their inventory to shortages. Hospital pharmacies? They lose 35-40%. And 60-65% of those missing drugs are sterile injectables. That’s not a coincidence. It’s by design. Why? Because hospitals rely on these drugs for everything. Anesthesia for surgery. Antibiotics for sepsis. Vasopressors for shock. Chemotherapy for cancer. There’s no oral version of epinephrine that works the same way. You can’t substitute a pill for a lifesaving IV drip. So when these drugs disappear, hospitals don’t just inconvenience patients-they delay surgeries, postpone cancer treatments, and sometimes send people home without proper care. Academic medical centers, which treat the most complex cases, report being hit 2.3 times harder than community hospitals. A nurse manager at Massachusetts General Hospital documented in June 2025 that 37 surgical procedures were postponed in just one quarter because of anesthetic shortages. That’s not a number. That’s 37 people who had to reschedule, worry, and wait-some with worsening conditions.The Most Affected Drugs: Anesthetics, Chemo, and Heart Medications
Some categories are hit harder than others. According to the U.S. Pharmacopeia’s 2025 report:- Anesthetics: 87% shortage rate
- Chemotherapeutics: 76% shortage rate
- Cardiovascular injectables: 68% shortage rate
The Human Cost: Ethical Dilemmas and Burnout
It’s not just about logistics. It’s about morality. A 2025 survey by the American Society of Health-System Pharmacists found that 68% of hospital pharmacists have faced ethical dilemmas because of shortages. Over 40% admitted they’ve had to use alternatives that weren’t as effective-medicines that might not work as well, or that carry higher risks. One pharmacist on Reddit, posting under the username ‘IVguy2025’, wrote: “Running out of normal saline for three weeks straight forced us to get creative with oral rehydration for post-op patients-never thought I’d see the day.” This isn’t just stressful. It’s traumatizing. Pharmacists are trained to deliver the right drug, at the right dose, at the right time. When they can’t, they feel like they’ve failed. A nurse at a Texas hospital told a colleague, “I had to tell a mom her child’s chemo was delayed because the drug didn’t arrive. She cried. I cried.” And the workload? It’s crushing. Hospital pharmacists now spend an average of 11.7 hours a week just managing shortages-tracking inventory, calling suppliers, documenting substitutions, training staff. That’s over two full workdays a week spent not on patient care, but on crisis management.Why the System Won’t Fix Itself
You’d think with all this pressure, someone would fix it. But the root causes are deeply entrenched. First, profit. Most sterile injectables are generics. That means manufacturers make very little money on them-often just 3-5% margins. Why invest in expensive sterile equipment, quality control, or backup supply lines when you can barely break even? Second, concentration. Just three companies control 65% of the market for essential injectables like sodium chloride and potassium chloride. If one fails, the whole system stumbles. There’s no competition. No backup. No safety net. Third, regulation is toothless. The FDA can’t force companies to make more drugs. They can’t fine them for shortages. They can’t require backup suppliers. The Drug Supply Chain Security Act only tracks where drugs go-it doesn’t make sure they’re made. The 2023 Consolidated Appropriations Act required earlier shortage notifications. But the Government Accountability Office found it only reduced shortage duration by 7%. Even the $1.2 billion federal investment in domestic manufacturing, announced in 2024, won’t help for years. Industry experts say it’ll take 3-5 years to see any real impact. By then, the damage will be done.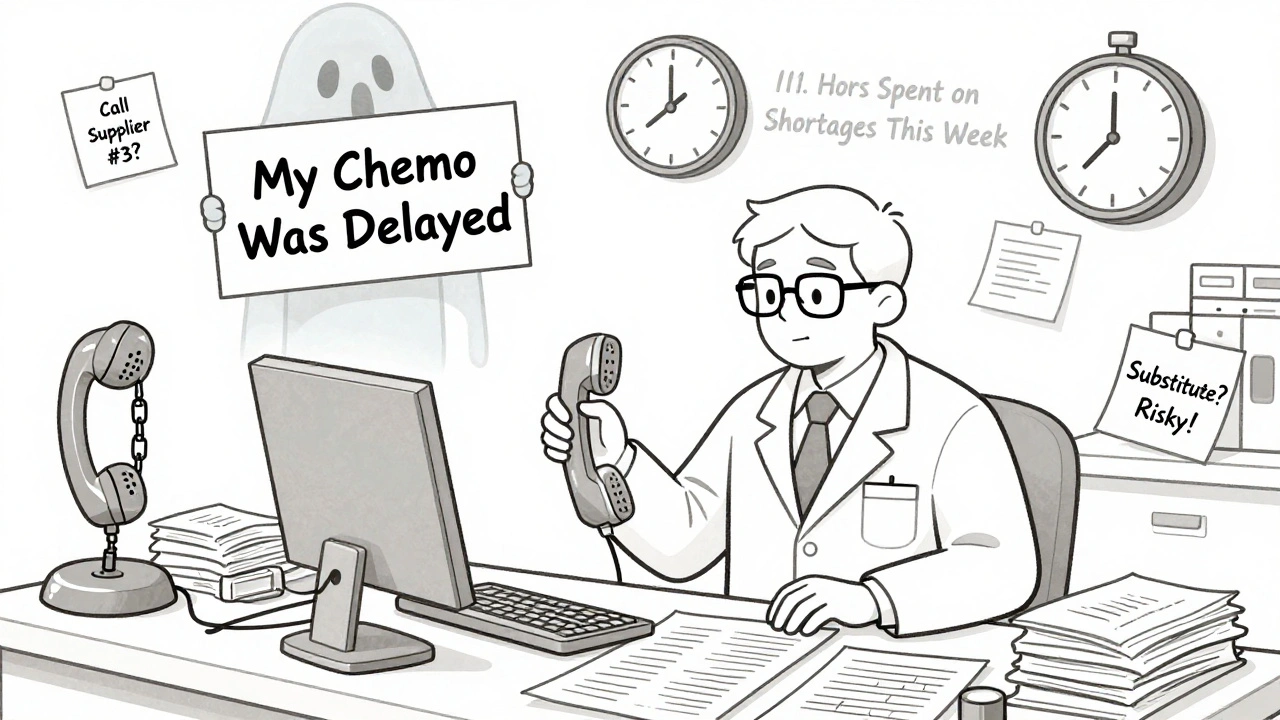
What Hospitals Are Doing-And Why It’s Not Enough
Hospitals aren’t sitting idle. Most have set up shortage management committees. 76% have formal plans. But only 32% feel those plans are properly funded or staffed. Some strategies are working-sort of:- Consolidating stock: Keeping all scarce drugs in one central location to prevent waste
- Therapeutic interchange: Getting approval to swap one drug for another, even if it’s less ideal
- Building relationships with alternative suppliers: Calling smaller manufacturers who might have stock
The Outlook: No Relief in Sight
The number of active shortages dropped from 270 in April 2025 to 226 in July 2025. That sounds like progress. But don’t be fooled. The same drugs are still missing. The same manufacturers are still struggling. The same patients are still at risk. Experts at IQVIA predict shortages will stay between 200 and 250 through 2027. Climate change is making extreme weather more common-more tornadoes, more floods, more plant shutdowns. Geopolitical tensions are disrupting supply chains from Asia. And generic drug prices? Still falling. Only 12% of sterile injectable manufacturers have adopted new technologies like continuous manufacturing, which could make production faster and more reliable. The rest are stuck in the same outdated, fragile system. Hospital pharmacies are doing everything they can. But they’re not manufacturers. They’re not regulators. They’re not policymakers. They’re the ones holding the bag when everything else breaks.What Needs to Change
Real solutions require systemic change:- Incentivize production: Pay manufacturers more for making high-risk injectables. Offer tax breaks, guaranteed purchases, or subsidies.
- Require redundancy: Mandate that critical drugs have at least two approved manufacturers.
- Invest in domestic capacity: Fund new sterile manufacturing plants in the U.S.-not just in the next five years, but right now.
- Empower the FDA: Give the agency authority to require quality improvements or temporarily suspend imports from unreliable sources.
- Support hospitals: Fund shortage management teams, not just in theory, but with real staffing and budget.

All Comments
Tejas Bubane December 10, 2025
Let’s be real-this isn’t a crisis, it’s capitalism playing Jenga with people’s lives. Generic injectables? Low margin. Why would any sane company invest in sterile production when they can just outsource to a factory in Chennai that doesn’t even have air filters? The FDA’s got no teeth, manufacturers got no incentive, and hospitals are left holding the bag while CEOs cash checks. We’re not talking about a glitch. We’re talking about a system designed to fail.
Lisa Whitesel December 12, 2025
It’s always the poor who die first. The rich get their drugs. The rest get rationed. No one cares until it’s their kid on the ventilator. Then suddenly it’s a national scandal. But by then it’s too late. We let this happen because we let corporations run healthcare. Simple as that.
Larry Lieberman December 14, 2025
So like… if we just paid manufacturers more to make these drugs, would that fix it? 🤔 I mean, I get that generics are low profit but like… if you’re literally watching someone die because they can’t get norepinephrine, maybe we need to stop pretending this is a market problem and start treating it like a public health emergency. Also, why are we still outsourcing 80% of the raw stuff to India and China? Like… we have the tech. We have the labs. We just don’t want to pay for it.
Courtney Black December 15, 2025
There is a deeper truth here, one that escapes the spreadsheet-driven policy wonks and the corporate lobbyists who sit in DC thinking in quarterly earnings. The system is not broken-it was never meant to work. It was designed to extract, not to heal. The sterile injectable is not just a drug-it is a symbol of our collective moral decay. We have turned life-saving medicine into a commodity, and in doing so, we have turned human beings into line items. The pharmacist who cries because she had to tell a mother her child’s chemo was delayed? That is not a tragedy. That is the inevitable outcome of a civilization that values profit over presence. We are not failing to fix this. We are choosing to fail.
Simran Chettiar December 16, 2025
It is truly unfortunate that the healthcare infrastructure in the United States has become so fragile. The reliance on foreign suppliers for critical active pharmaceutical ingredients is a strategic vulnerability that has been ignored for decades. One would think that after the pandemic, when every country realized the danger of supply chain dependence, the U.S. would have taken decisive action. But no. Instead, we continue to prioritize cost over safety, and efficiency over equity. The result? Patients suffer. Nurses burn out. Pharmacists are forced into ethical compromises they never signed up for. This is not a shortage. This is a failure of leadership.
Anna Roh December 18, 2025
why is this even a thing. like. we have the money. we have the tech. we have the hospitals. but we don’t have the will. sad.
Philippa Barraclough December 19, 2025
The data presented here is compelling, but it’s worth noting that the concentration of manufacturing in two countries is not unique to pharmaceuticals-it’s a global trend across high-precision industries. The issue is systemic vulnerability, not just pharmaceutical policy. The FDA’s inability to mandate redundancy or enforce quality standards is symptomatic of broader regulatory capture. Without structural reform in both manufacturing incentives and international trade policy, we’re merely rearranging deck chairs on the Titanic. The 2023 legislation’s 7% reduction in shortage duration confirms this: incrementalism is not a strategy.
Tiffany Sowby December 20, 2025
It’s all because we let foreigners control our medicine. If we just made this stuff in America like we used to, none of this would happen. We don’t need to pay more. We just need to stop outsourcing to countries that don’t care about our kids. This isn’t about profit-it’s about loyalty. And if American companies won’t make these drugs, then maybe we should ban imports until they do. We’ve got the land. We’ve got the people. We’ve got the will. We just need to stop being weak.
Asset Finance Komrade December 21, 2025
One might argue that the real issue is not the shortage of injectables, but the over-reliance on injectables in the first place. Why is IV administration the default for everything? Why not invest in oral bioavailability enhancements? Why not develop inhaled or transdermal alternatives? The entire paradigm is outdated. We’ve been treating symptoms for decades while ignoring the architecture of care. The problem isn’t just supply-it’s the entire medical model that equates potency with injection. Maybe the solution isn’t more factories… but fewer needles.
Brianna Black December 23, 2025
Let me tell you something about hospital pharmacies. I’ve worked in one for 18 years. I’ve watched nurses cry because they had to give a child a less effective chemo drug. I’ve stood in the supply room at 3 a.m. with a clipboard, calling every pharmacy in three states because we were out of propofol. I’ve seen patients die because the drug didn’t arrive. And you know what? No one in Congress has ever asked me how it felt. No one has ever thanked me for staying awake through another shortage. This isn’t a policy debate. It’s a funeral. And we’re all standing around, pretending we didn’t see the body.
Shubham Mathur December 25, 2025
Guys I’ve been in this game since 2015 and I’ve seen it all. The real problem? No one trains pharmacists to handle shortages. No one. We get zero coursework on therapeutic interchange protocols. No simulation labs. No funding for shortage teams. And yet we’re expected to be doctors, negotiators, and crisis managers all at once. And then people wonder why we’re burning out. We need real investment-not just in manufacturing, but in the people who are holding this thing together. And we need it yesterday. Not in 5 years. Now.
Stacy Tolbert December 26, 2025
I just read this whole thing and I’m so tired. I work in oncology. I’ve had to tell three patients this year their chemo was delayed because the drug wasn’t shipped. I don’t cry in front of them anymore. I just smile and say we’re doing everything we can. But I cry after my shift. I cry when I see my own mom take her pills and think-what if she needed an IV drug? What if it was gone? I’m not angry. I’m just… empty. And I don’t know how much longer I can do this.
Ronald Ezamaru December 27, 2025
There’s a lot of focus on manufacturing, but let’s not forget the role of distribution. Many shortages aren’t due to lack of production-they’re due to hoarding, panic buying, and gray market resellers. Hospitals in rural areas get left behind because the big chains buy up all the stock. And then we wonder why some places have zero norepinephrine while others have 3x the needed supply. We need a national allocation system, not just a patchwork of emergency calls. Also-yes, we need domestic manufacturing-but we also need better logistics. This isn’t just a drug problem. It’s a supply chain problem.
Rich Paul December 27, 2025
bro the whole system is just a scam. injectables are like the crypto of pharma-super complicated, zero transparency, and everyone’s just pretending they know what’s going on. FDA? More like FDA-just-wait-a-bit. Manufacturers? Lazy. Hospitals? Overworked. Patients? Screwed. And the only people who win are the ones who own the patents on the alternatives. Meanwhile, normal saline is harder to get than a concert ticket. This isn’t medicine. It’s a meme.