Linezolid & Antidepressant Risk Checker
Based on the latest medical research, the risk of serotonin syndrome with linezolid and most antidepressants is much lower than previously thought. This tool helps you understand your individual risk factors.
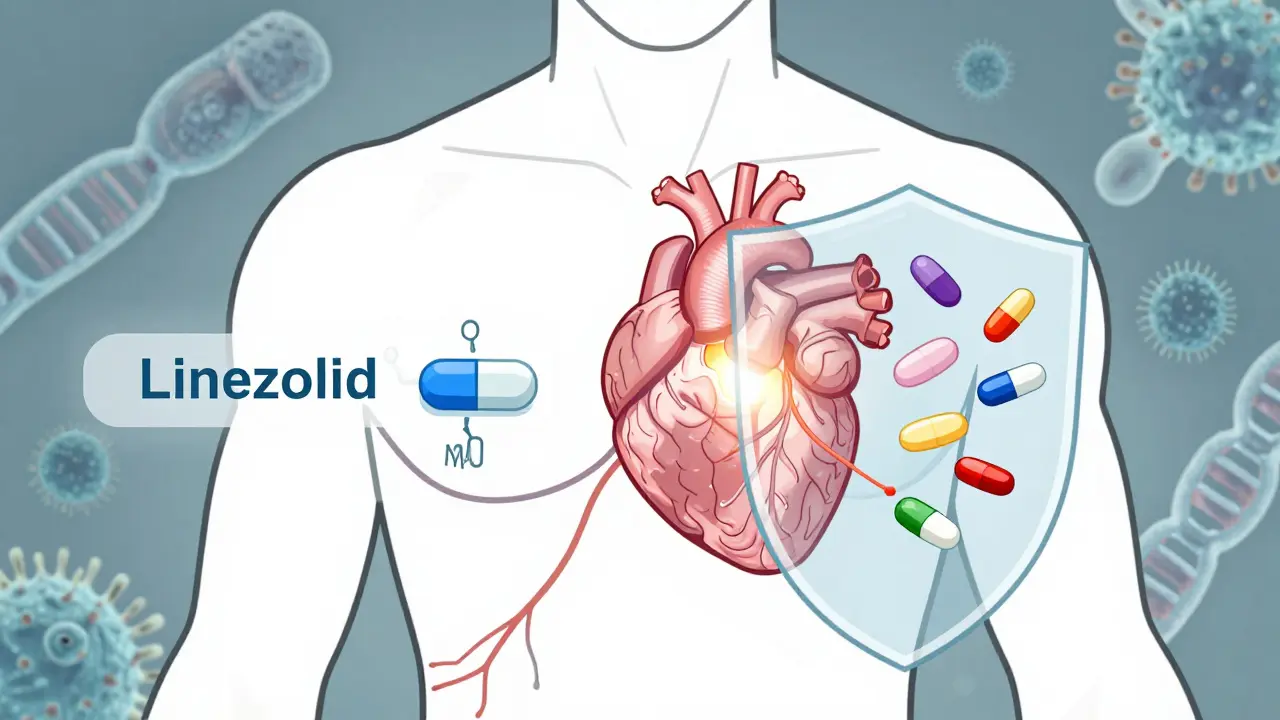
When you're fighting a serious infection like MRSA or VRE, linezolid can be a lifesaver. But if you're also taking an antidepressant, you might have heard warnings about serotonin syndrome-a rare but dangerous reaction. So, is it safe? Or should you avoid linezolid altogether? The answer isn't as simple as it sounds.
What Is Linezolid, Really?
Linezolid is an antibiotic used for tough bacterial infections, especially those resistant to other drugs like MRSA and VRE. It was first approved by the FDA in 2000 and is still on the WHO’s list of essential medicines today.
Unlike most antibiotics, linezolid doesn’t attack bacteria by breaking down their cell walls. Instead, it stops them from making proteins by binding to their ribosomes. This unique trick makes it one of the few options left when other antibiotics fail.
But here’s the twist: linezolid was originally developed as a potential antidepressant. It weakly blocks monoamine oxidase (MAO), the enzyme that breaks down serotonin in the brain. That’s why it can affect mood-and why it might interact with antidepressants.
What Is Serotonin Syndrome?
Serotonin syndrome is a potentially life-threatening condition caused by too much serotonin in the nervous system.
It doesn’t happen from one pill. It builds up-usually within 24 to 72 hours after starting a new drug. Symptoms come in three groups:
- Cognitive: Agitation, confusion, restlessness
- Autonomic: Sweating, fast heartbeat, high fever, shivering
- Neuromuscular: Muscle twitching, tremors, stiff muscles, overactive reflexes
In severe cases, it can lead to seizures, kidney failure, or even death. But most cases are mild and go away once you stop the drug causing it.
Why Do Doctors Worry About Linezolid and Antidepressants?
The fear started in the early 2000s. Case reports popped up: a 70-year-old woman on linezolid for pneumonia developed serotonin syndrome-even without any antidepressants. Another patient on fluoxetine and linezolid had a seizure. The FDA issued a warning in 2011, listing SSRIs, SNRIs, MAO inhibitors, and even some painkillers and herbal supplements as risky.
That warning stuck. Even today, many doctors avoid combining linezolid with antidepressants. But here’s the problem: those early reports were rare. One case here, another there. No big studies. Just fear.
The Real Risk: What the Data Actually Shows
In 2023, a major study changed the game. Researchers looked at over 1,100 patients given linezolid. Nearly 200 of them were also taking antidepressants. The results? Only 5 cases of serotonin syndrome total-and none happened in the group taking antidepressants.
The adjusted risk difference? -1.2%. That means patients on antidepressants actually had slightly lower rates of serotonin syndrome than those who weren’t. The study authors concluded: “Linezolid is likely safe for patients receiving antidepressants.”
Another 2024 study of 3,852 patients found the same thing: no increase in serotonin syndrome risk when linezolid was combined with SSRIs or SNRIs. The odds ratio? 0.87-meaning the risk was actually lower, not higher.
So why the disconnect? Linezolid is a weak MAO inhibitor. Its power to block serotonin breakdown is about 50 to 100 times weaker than older antidepressants like phenelzine. That’s why it doesn’t cause tyramine reactions (like the famous “cheese effect”) as often. And why serotonin syndrome is so rare.
Who’s at Real Risk?
Not everyone. The danger spikes when you combine linezolid with:
- MAO inhibitors: Like phenelzine or tranylcypromine. These are strong, and the combination is dangerous.
- High-dose linezolid: 600 mg twice daily (used in severe infections) increases exposure.
- Multiple serotonergic drugs: Taking linezolid + an SSRI + dextromethorphan + St. John’s wort? That’s a recipe for trouble.
- Older adults or kidney problems: Linezolid builds up in the body if kidneys aren’t working well. Older patients are more sensitive to CNS effects.
Most people on standard doses of linezolid (600 mg once daily) with one antidepressant face almost no risk.
What Should You Do?
If you’re on an antidepressant and your doctor says you need linezolid:
- Don’t panic. The evidence says it’s safe for most.
- Ask about alternatives. If you have other options (like vancomycin), weigh the risks.
- Watch for symptoms. Especially in the first 3 days. If you feel unusually agitated, sweaty, or your muscles start twitching, call your doctor immediately.
- Know the treatment. If serotonin syndrome happens, stopping linezolid is step one. Benzodiazepines calm the nervous system. Cyproheptadine blocks serotonin receptors. Supportive care (cooling, fluids) helps the body recover.
Many clinicians still avoid the combo out of habit. But the science is clear: the fear was overblown. The real danger isn’t the antidepressant-it’s not treating the infection.
The Bottom Line
Linezolid and antidepressants? For most people, it’s fine. The risk of serotonin syndrome is less than 0.5%. That’s lower than the risk of a bad reaction to a common painkiller.
The FDA hasn’t updated its warning. Some guidelines still say “use caution.” But the latest data-published in top journals like JAMA and Clinical Infectious Diseases-shows that the benefits outweigh the risks in almost all cases.
If you’re on an SSRI or SNRI and need linezolid for a serious infection, don’t refuse it. Talk to your doctor. Get monitored for a few days. But don’t let outdated warnings keep you from a life-saving antibiotic.
Can linezolid cause serotonin syndrome without antidepressants?
Yes, but it’s extremely rare. There are documented cases where patients developed serotonin syndrome on linezolid alone, usually at high doses (600 mg twice daily) or with other risk factors like older age or kidney issues. However, these cases are outliers. Most people on linezolid, even without antidepressants, never develop serotonin syndrome.
Which antidepressants are safest with linezolid?
SSRIs like sertraline or escitalopram and SNRIs like venlafaxine are the most commonly used and studied with linezolid. They carry the lowest risk. Avoid combining linezolid with MAO inhibitors (phenelzine, tranylcypromine) or drugs like dextromethorphan, meperidine, or St. John’s wort. These raise the risk more significantly.
How long should I wait after stopping linezolid before starting an MAO inhibitor?
Linezolid’s effect on MAO lasts about 2 weeks after the last dose because it takes time for the body to make new enzyme. Most experts recommend waiting at least 14 days before starting an MAO inhibitor like phenelzine. For SSRIs or SNRIs, no waiting period is needed if you’re switching from linezolid to them.
Does linezolid interact with food like older MAO inhibitors?
Linezolid can theoretically interact with tyramine-rich foods like aged cheese, cured meats, or tap beer, but the risk is very low. Unlike older MAO inhibitors, linezolid’s inhibition is weak and temporary. Most patients can eat these foods without issue. Still, if you’re on high-dose linezolid or have other risk factors, it’s safer to avoid them.
What should I do if I think I have serotonin syndrome?
Stop linezolid and any other suspected drugs immediately. Call emergency services or go to the ER. Mild cases can be managed with benzodiazepines and close monitoring. Severe cases need intensive care-cooling, IV fluids, and sometimes cyproheptadine. Recovery usually happens within 24 hours if caught early.
All Comments
Chima Ifeanyi February 7, 2026
Let’s deconstruct this like a pharmacokinetic model: linezolid’s MAO-A inhibition is ~10^-5 M Ki, which is 100x weaker than phenelzine’s sub-micromolar affinity. The 2023 JAMA study’s adjusted OR of 0.87 isn’t just statistically insignificant-it’s biologically noise. You’re talking about a drug with a half-life of 5 hours, dosed Q12H, and even at 600mg BID, plasma concentrations barely breach 12 µg/mL. Serotonin syndrome requires sustained, supra-therapeutic MAO inhibition. This isn’t a contraindication-it’s a myth perpetuated by risk-averse clinicians who haven’t read a paper since 2005.
Also, the FDA’s 2011 warning was based on case reports with confounders: polypharmacy, renal impairment, unrecognized serotoninergic agents. Zero prospective trials. Zero meta-analyses. Just fearmongering dressed up as clinical guidance. If we applied that logic to every weak MAOI, we’d ban coffee, chocolate, and decongestants.
Tori Thenazi February 8, 2026
Okay, but… what if… the FDA is lying?? 🤔 I mean, think about it-pharma companies fund all the studies, right? And linezolid is EXPENSIVE. What if they’re hiding the real data? I read a Reddit thread where someone said their uncle died after taking linezolid with Zoloft… and then the hospital said ‘it was just pneumonia’… 😳
Also, I saw a documentary about how the WHO is controlled by Big Pharma. And what about the 2024 study? Was it peer-reviewed? Or just a corporate press release? I’m not saying it’s fake… but I’m not saying it’s real either. 🤷♀️
And what if serotonin syndrome is just… the government’s way of controlling our moods?? 🤯
Elan Ricarte February 8, 2026
Oh, so now we’re pretending that ‘weak MAO inhibition’ means ‘safe’? Bro, you’re one missed dose of dextromethorphan away from turning into a human seizure machine. I’ve seen guys on linezolid + citalopram go full-on ‘I’m a god, I can fly’ mode. One guy tried to lick the ceiling. Another thought his cat was a CIA drone.
And don’t get me started on the ‘low risk’ narrative. That’s not science-that’s wishful thinking wrapped in a JAMA bow. You think 0.5% is low? Try telling that to the guy whose kidneys shut down because he was ‘just fine.’
Here’s the truth: if you’re on an SSRI and you’re dumb enough to take linezolid, you deserve what you get. This isn’t a risk-it’s a gamble with your brain. And I don’t play Russian roulette with neurotransmitters.
Susan Kwan February 9, 2026
Wow. So we’re just gonna ignore the fact that linezolid’s MAO inhibition is cumulative? That’s not ‘weak’-it’s sneaky. You don’t get serotonin syndrome on day one. You get it on day 5, when your doctor says ‘you’re fine’ and you’re already hallucinating your IV bag is talking to you.
And let’s be real: ‘most cases are mild’ is a lie. Mild cases still mean ICU. Mild cases still mean 3 days of muscle spasms so bad you pee yourself. Mild cases still mean your family thinks you’re psychotic.
Stop romanticizing this. You’re not ‘saving lives’ if you’re turning people into human panic attacks. There’s vancomycin. There’s daptomycin. There’s even teicoplanin. Why risk it? Because you’re too lazy to look up alternatives?
MANI V February 11, 2026
People like you think science is about data. But science is about responsibility. You talk about ‘low risk’ like it’s a math problem. But human lives aren’t percentages. I’ve seen a 72-year-old woman convulse for 14 hours because someone thought ‘it’s probably fine.’
And now you want to normalize this? What’s next? Combining MAOIs with MDMA because ‘the studies say it’s safe’? You’re not a doctor-you’re a cheerleader for arrogance.
Every time we lower the bar on safety, someone dies. And then we call it ‘rare.’ Rare doesn’t mean ‘not worth caring about.’ It means ‘we didn’t care enough to stop it.’
Random Guy February 12, 2026
yo so like… i got linezolid for a staph infection last year and was on lexapro. thought i was gonna die. kept thinking my toaster was whispering to me. turned out it was just anxiety… but also maybe not?? idk. point is: if your brain feels weird, stop it. no cap.
Monica Warnick February 14, 2026
I’m not a doctor, but I’ve read a lot of papers. The 2023 study had a small sample size. And what about the patients who had serotonin syndrome but didn’t report it? Or got misdiagnosed? Or were too sedated to say anything?
Also, linezolid is given in hospitals. What about the patients who are on 5+ serotonergic meds? The study didn’t stratify by polypharmacy. That’s a massive confounder.
And the ‘lower risk’ finding? That’s probably because the antidepressant group was monitored more closely. Of course they had fewer cases-they were watched. That’s not safety. That’s surveillance bias.
Just because it’s statistically neutral doesn’t mean it’s safe. We need more data. Not just ‘trust the numbers.’
Tom Forwood February 15, 2026
As a guy who’s lived in 7 countries and worked in 3 ERs, I’ve seen this play out. Linezolid + SSRI? In Nigeria? In India? In rural Ohio? You don’t even know what meds people are taking. Some take St. John’s wort ‘cause it’s cheap. Some take tramadol ‘cause it’s in their medicine cabinet. Some take fluoxetine ‘cause their cousin said it helped.
So yeah, in a controlled trial? Maybe it’s fine. But in the real world? It’s a minefield. And the people who get hurt? They’re not in the studies. They’re the ones without insurance. Without follow-up. Without a voice.
Don’t call it ‘safe.’ Call it ‘risky but worth it in emergencies.’ That’s the truth.
Chelsea Cook February 15, 2026
Y’all are overcomplicating this. If you’re on an antidepressant and you need linezolid? You’re probably fighting a life-threatening infection. So yeah, take it. But monitor. Like, actually monitor. Not ‘oh, you’re fine’-but ‘did you sleep? Did you feel hot? Did your leg jerk?’
And if you’re a doctor? Stop being scared of liability. Start being scared of death. MRSA doesn’t care if your paperwork says ‘avoid.’ It just kills you.
Science says: use it. Common sense says: watch. That’s not a contradiction. That’s called being human.
Karianne Jackson February 16, 2026
My mom took linezolid with Zoloft and got really weird. She kept hugging the walls. Said the fridge was singing. We thought it was dementia. Turned out it was serotonin syndrome. She’s fine now. But I’ll never trust ‘low risk’ again.