Medication Hair Loss Recovery Estimator
Recovery Timeline Calculator
Enter when you stopped your medication to see when you might expect hair regrowth based on the type of hair loss you experienced.
When you start a new medication, you expect it to help - not hurt. But for some people, a common side effect shows up in the mirror: thinning hair, more strands in the brush, or a wider part than usual. This isn’t just bad luck. It’s a well-documented condition called medication-induced hair loss or drug-induced alopecia. And the good news? In most cases, it’s reversible.
Every year, about 4.7 million Americans deal with this issue, according to the National Institutes of Health. It’s not rare. It’s not always talked about. But if you’re noticing your hair shedding more than usual after starting a new drug, you’re not alone.
How Medications Cause Hair Loss
Not all hair loss from meds works the same way. There are two main mechanisms, and knowing which one you’re dealing with helps you understand what to expect.
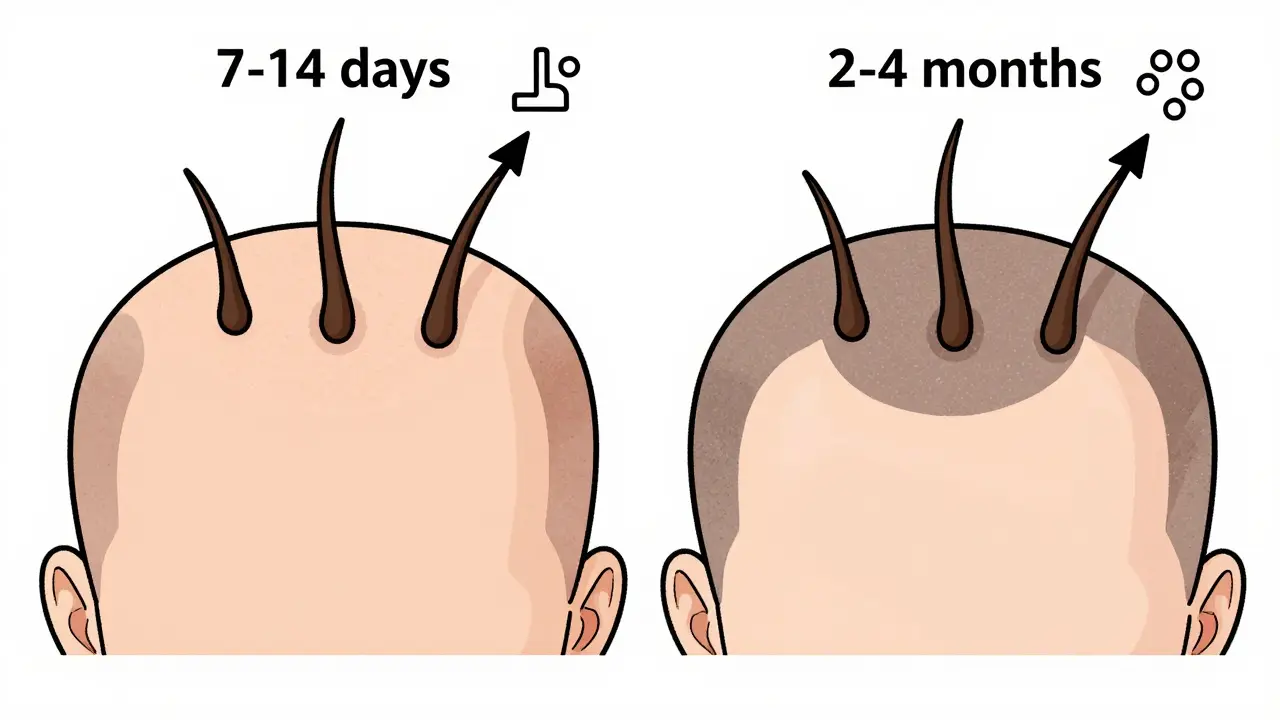
The most common type is telogen effluvium. This happens when a medication pushes a large number of hair follicles into their resting phase too early. Normally, hair grows for years before it sheds. But with telogen effluvium, those follicles stop growing and fall out - all at once. The timing is tricky: you might start a medication today, but not notice the hair loss until 2 to 4 months later. That’s because it takes time for the follicles to cycle through. Shedding usually peaks around month three and can last up to six months. But once the drug is stopped, hair typically grows back fully within 6 to 9 months.
The other type is anagen effluvium. This is more dramatic. It happens when drugs - usually chemotherapy - attack fast-growing cells, including hair follicles in their active growth phase. Hair doesn’t just thin; it falls out in clumps. This can start within 7 to 14 days of the first dose. About 65% of people on chemo experience this. The good part? Hair usually starts growing back 3 to 6 weeks after treatment ends. But sometimes, the texture changes - curlier, finer, or even a different color. That’s normal.
Which Medications Are Most Likely to Cause It?
Not every drug causes hair loss. But some classes have a clear pattern. Here are the most common culprits:
- Antidepressants - SSRIs like sertraline and fluoxetine cause hair loss in about 5-7% of users. Many people don’t realize this is a side effect until they’re already shedding.
- Blood pressure meds - Beta-blockers (like metoprolol) and ACE inhibitors (like lisinopril) are linked to telogen effluvium. It’s rare, but it happens.
- Arthritis drugs - Methotrexate affects 1-3% of users. Leflunomide? Up to 10%. That’s why many rheumatologists now recommend folic acid (1mg daily) alongside methotrexate - it reduces hair loss severity by about 25%.
- Oral retinoids - Drugs like isotretinoin (for acne) cause hair thinning in nearly 18% of users. It’s one of the most predictable side effects.
- Chemotherapy - This is the big one. Drugs like paclitaxel and doxorubicin cause anagen effluvium in most patients. That’s why scalp cooling systems like the DigniCap are now common in oncology clinics.
If you started a new medication within the last 7 months and your hair started thinning, it’s very likely connected. Dermatologists call this the “7-month rule.” It’s not perfect, but it’s a solid starting point.
What You Can Do - Real, Proven Steps
First, don’t panic. And don’t stop your medication without talking to your doctor. The key is to identify the cause - then act.
1. Give it time - and don’t rush
Most cases of telogen effluvium fix themselves. The American Academy of Dermatology recommends waiting at least 3 months after stopping the drug before trying anything else. Why? Because 85% of people see full regrowth naturally in that time. Jumping into treatments too early can waste money and time.
2. Try minoxidil (Rogaine)
This is the most studied topical treatment. A 5% solution, applied twice daily, shows 40-50% improvement in hair density after 6 months. It’s available over the counter. But here’s the catch: 89% of users experience more shedding in the first 2-8 weeks. That’s not a sign it’s not working - it’s a sign it is. Stick with it. If you stop at week 6 because you’re scared, you’ll never see results.
3. Consider finasteride or dutasteride (if appropriate)
These are oral drugs that block DHT, a hormone linked to hair loss. They’re not FDA-approved for medication-induced hair loss, but studies show they help when the shedding is mixed with genetic thinning. Finasteride works for 60-65% of users. Dutasteride is stronger (70-75% efficacy) but has more side effects. Always talk to a dermatologist before starting these.
4. Try low-level laser therapy
Devices like the iRestore Elite 780 and Capillus82 are FDA-cleared Class II medical devices. Clinical trials show 65-90% of users see measurable improvement after 26 weeks. You use them 20-30 minutes a day, every day. No pills. No creams. Just light. It’s not magic, but it’s science-backed.
5. Support hair health with nutrition
Hair needs fuel. If you’re deficient in iron, zinc, or biotin, your follicles can’t recover as fast. Dermatologists often recommend:
- Biotin: 5,000 mcg daily
- Zinc: 15 mg daily
- Iron: Only if your ferritin level is below 70 ng/mL (get tested)
Don’t just take random supplements. Get bloodwork done first. Too much zinc can cause nausea. Too much iron can be dangerous.
What About Chemo and Scalp Cooling?
If you’re on chemotherapy, scalp cooling is the most effective way to preserve hair. The DigniCap system cools the scalp to about 22°C (72°F) before, during, and after each infusion. Studies show it helps 50-65% of patients keep at least half their hair. For breast cancer patients on taxanes, retention rates are even higher - up to 65%.
But it’s not easy. The cooling cap is tight, cold, and worn for 90 minutes per session. Many patients rate the discomfort at 7.2 out of 10. Still, 82% say it’s worth it. If your oncology center doesn’t offer it, ask. It’s becoming more common.
What Doesn’t Work - And Why
There’s a booming market for hair supplements. Nutrafol, Viviscal, Hairburst - they’re everywhere. Amazon reviews for Nutrafol show 4.1 out of 5 stars. But here’s what the data says: 63% of users report improvement after 6 months. That sounds good - until you look at the ingredients. They contain marine collagen (5,000mg), ashwagandha (390mg), and curcumin (250mg). None of these have strong clinical proof for reversing drug-induced hair loss. They might help if you’re deficient in nutrients. But they won’t fix a medication problem.
Same goes for essential oils, scalp massages, or “natural” shampoos. They feel good. They might improve scalp health. But they won’t stop telogen effluvium or anagen effluvium.

What to Expect - Real Timelines
Here’s a simple timeline to help you track your progress:
- Weeks 1-4: You start a new medication. Nothing changes.
- Month 2-4: You notice more hair in the shower, on your pillow, in your brush.
- Month 5-6: Shedding peaks. Hair feels thinner overall.
- Month 7-9: Shedding slows. New hairs start to appear - fine, fuzzy, and lighter.
- Month 10-12: Hair thickens. Texture and color return to normal.
For chemo patients: Shedding starts in days. Regrowth begins in 3-6 weeks. Texture changes? Common. But hair usually looks normal again in 6-12 months.
When to See a Dermatologist
You don’t need to wait a year. If:
- Your hair loss lasts longer than 6 months after stopping the drug
- You’re losing hair in patches (not diffuse thinning)
- You have other symptoms - scalp redness, itching, scaling
- You’re not sure what’s causing it
Then it’s time to see a specialist. They can do a pull test, examine your scalp with a dermoscope, and order blood tests. Sometimes, what looks like drug-induced hair loss is actually something else - like thyroid issues, iron deficiency, or early androgenetic alopecia.
Emotional Impact - It’s Real
Hair loss isn’t just physical. In a 2023 survey by Medical News Today, 82% of people said it hurt their self-esteem. Nearly half withdrew socially. One woman on Reddit wrote: "I stopped going to family gatherings because I couldn’t handle the questions." It’s okay to feel this way. Talk to someone. Join a support group. Reddit’s r/HairLoss has over 247,000 members. Many share their recovery stories - and they’re full of hope.
Can medication-induced hair loss be permanent?
In most cases, no. Telogen effluvium from medications is almost always reversible. Anagen effluvium from chemo usually reverses too, though texture may change. Permanent hair loss is rare and usually only happens if the drug causes scarring (which is uncommon) or if you have an underlying condition like androgenetic alopecia that was triggered or worsened by the medication.
How long after stopping a medication does hair start to grow back?
It varies. For telogen effluvium, new hair often appears between 3 and 6 months after stopping the drug. Full regrowth can take 9-12 months. For anagen effluvium (chemo), regrowth can begin as early as 3-6 weeks after treatment ends. The speed depends on your body’s healing rate, age, and overall health.
Is minoxidil safe to use with other medications?
Yes, minoxidil is generally safe to use alongside most medications. It’s a topical treatment, so very little enters your bloodstream. But if you’re using other topical treatments (like steroids or retinoids), ask your dermatologist about possible interactions. Also, avoid using it if you have a rash or open sores on your scalp.
Do supplements like biotin help with drug-induced hair loss?
Only if you’re deficient. Biotin deficiency is rare. Taking extra biotin won’t fix hair loss caused by medication. But if your blood test shows low iron, zinc, or ferritin, correcting those deficiencies can help your hair recover faster. Always test before supplementing.
Can I prevent medication-induced hair loss before it starts?
For most medications, no. But for chemotherapy, scalp cooling (like DigniCap) can reduce hair loss by up to 65%. For methotrexate, taking folic acid daily reduces severity by 25%. Research is also moving toward genetic testing - in 2023, Mayo Clinic identified 17 SNPs linked to higher risk of drug-induced hair loss. In the future, doctors may test your genes before prescribing certain drugs.
Medication-induced hair loss is frustrating, but it’s rarely permanent. With the right approach - patience, the right treatments, and professional guidance - your hair can come back. And if it doesn’t? You’re not broken. You’re just one step away from the next solution.

All Comments
Haley DeWitt February 15, 2026
I started sertraline last year and lost like 30% of my hair... I thought I was going bald at 28 😭. Took me 8 months to realize it was the med. Stopped it, switched to bupropion, and my hair is finally coming back. Minoxidil helped a ton too. Don't panic, but DO talk to your doc!
John Haberstroh February 16, 2026
Honestly? This post is a godsend. I've been googling 'why is my hair falling out like confetti?' for weeks. The timeline breakdown alone? Gold. Also, the part about minoxidil shedding first? That's the kind of info you only get from someone who's been there. Thank you.
Carrie Schluckbier February 18, 2026
BUT DID YOU KNOW? The pharmaceutical industry KNOWS about this. They hide it. Why? Because if people knew how many drugs cause hair loss, they'd stop taking them. And then the profits drop. They'd rather you go bald than admit it. Scalp cooling? That's just a band-aid. The real solution? Ban all these drugs. #PharmaCoverUp
guy greenfeld February 18, 2026
Hair loss. It's not just biology. It's existential. You look in the mirror and the person staring back isn't you anymore. The follicles don't care about your resume, your relationships, your dreams. They just... stop. And suddenly, you realize how fragile identity is. We're all just a few strands away from becoming strangers to ourselves.
Adam Short February 20, 2026
This is why Britain's NHS should never be privatized. In the US, you need to pay for minoxidil, laser caps, blood tests... In the UK, we get it covered. We don't have to choose between eating and saving our hair. This is a healthcare crisis, not a personal failure.
Sam Pearlman February 20, 2026
Wait, so Nutrafol is a scam? But the reviews are so good! And the packaging looks so fancy! And the guy in the ad says he 'reclaimed his confidence'! I just spent $120 on it... 😭
Steph Carr February 21, 2026
So let me get this straight: we're being told to 'be patient' while our hair falls out, then spend hundreds on topical treatments, then get bloodwork, then maybe try lasers... Meanwhile, the drug that caused this is still on the market, still being prescribed, still making billions. And we're supposed to feel grateful for the 'proven steps'? 😂 I'm not mad. I'm just... disappointed.
Prateek Nalwaya February 22, 2026
I'm from India, and here, most people just use coconut oil and curry leaves. No one talks about minoxidil or lasers. But I tried both after my methotrexate started thinning my hair. The oil felt nice, but the minoxidil? Actually worked. The science wins. Also, folic acid is a game-changer. Took me 6 months to find this out. Glad someone wrote it clearly.
Philip Blankenship February 22, 2026
I had telogen effluvium from a beta-blocker after my heart surgery. Took me 10 months to grow it back. I didn't do anything except wait. No minoxidil. No supplements. Just time. And patience. And a hat. Lots of hats. The body heals itself. We just forget that sometimes. The real takeaway? Don't panic. Don't overreact. Just... wait. It'll come back. It always does.
Oliver Calvert February 22, 2026
Scalp cooling works. Saw it in action at my hospital. Patient on paclitaxel kept 80% of her hair. She cried when she saw herself. That's not science. That's dignity.
Linda Franchock February 24, 2026
I'm a nurse. I've seen this a hundred times. The most heartbreaking part? People blame themselves. 'I must be stressed.' 'I'm not eating right.' 'I'm not taking care of myself.' No. It's the drug. Not you. You're not broken. The system is just... weird.
Jonathan Ruth February 24, 2026
Minoxidil makes you shed more at first? That's not science. That's psychological warfare. They want you to keep buying it. I did 3 months. Then I stopped. My hair came back anyway. I'm not a lab rat for Big Pharma.
Digital Raju Yadav February 25, 2026
This is why America is failing. You get a drug that makes you lose hair, then you pay $200 for a laser cap? We in India get herbal oils for 50 rupees. You people overcomplicate everything. Just stop the drug. Let your body heal. Simple.
Liam Earney February 26, 2026
I just want to say... thank you for writing this. I didn't know anyone else felt this way. I've been hiding my hair loss for months. I stopped hugging people. I stopped taking selfies. I thought I was the only one. This... this made me feel less alone. Even if I don't use any of the treatments. Just knowing it's not my fault. That's enough.