Every year, thousands of seniors end up in the hospital-not because of a fall, heart attack, or infection, but because of a medication they were told to take. It’s not rare. It’s not an accident. It’s a pattern. And it’s entirely preventable.
Why Seniors Are More Vulnerable to Medication Risks
As we age, our bodies change in ways most people don’t realize until it’s too late. The liver doesn’t process drugs as quickly. The kidneys filter them out slower. Brain receptors become more sensitive. Even a normal dose of a drug that’s fine for a 40-year-old can be dangerous for someone over 65.On top of that, most seniors take multiple medications. The CDC says about 40% of older adults are on five or more prescriptions. That’s called polypharmacy. And with each new pill, the risk of harmful interactions, side effects, and confusion goes up. A drug that’s safe alone can turn risky when mixed with another. And many seniors don’t even know they’re taking something dangerous.
The Beers Criteria is the gold standard for spotting these risks. Developed by the American Geriatrics Society and updated every two years, it’s a list of medications that are more likely to harm seniors than help them. The 2023 version is the most current-and it’s not just a suggestion. Medicare Advantage plans use it to decide what drugs to cover. Pharmacies use it to flag prescriptions. Doctors who ignore it are putting lives at risk.
Top 5 High-Risk Medications for Seniors (And What to Use Instead)
1. Zolpidem (Ambien®) and Other Sleep Pills
Many seniors take zolpidem to help them sleep. But it doesn’t just help them sleep-it can make them sleepwalk, confuse them the next day, or cause them to fall. Studies show seniors on zolpidem have an 82% higher chance of falling than those who don’t. And those falls? They often lead to broken hips, long hospital stays, and even death.
The real problem? The drug lingers in the body. While a younger person might metabolize it in 6 hours, a 75-year-old can still feel its effects 11 hours later. That’s why so many seniors report feeling groggy, unsteady, or confused in the morning.
Better alternatives: Start with sleep hygiene-consistent bedtime, no screens before bed, avoiding caffeine after noon. If that doesn’t work, trazodone (a low-dose antidepressant) is often safer. Cognitive behavioral therapy for insomnia (CBT-I) works better than pills for most older adults and has no side effects.
2. Glyburide (Diabeta®) for Diabetes
Glyburide is an old-school diabetes pill that forces the pancreas to pump out more insulin. Sounds good, right? Except in seniors, it often pushes blood sugar too low. The result? Dizziness, confusion, fainting, seizures-even coma.
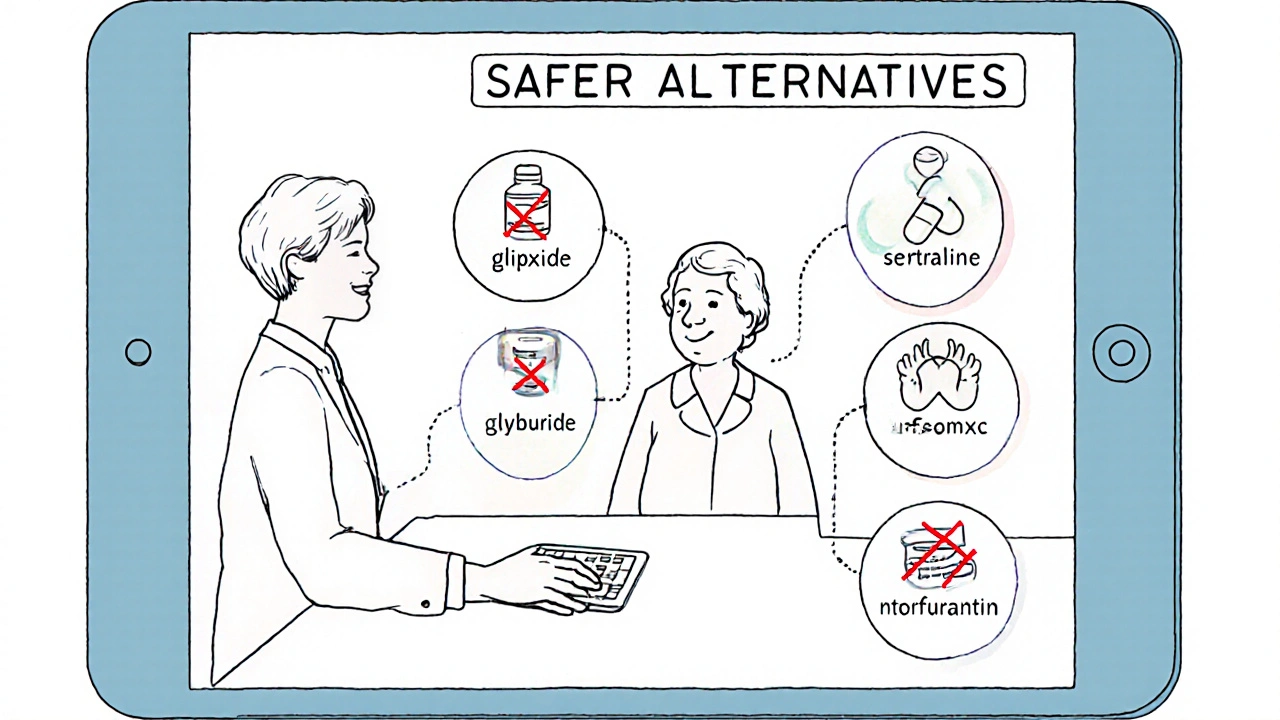
Studies show glyburide causes hypoglycemia in nearly 30% of elderly patients. That’s more than double the rate of newer drugs like glipizide. And because seniors often don’t feel the early warning signs of low blood sugar, they can crash without knowing it.
In 2023, the FDA added a boxed warning to glyburide labels specifically for patients over 65. That’s the strongest warning the agency gives.
Better alternatives: Glipizide, metformin, or GLP-1 agonists like semaglutide. These drugs are less likely to cause dangerous lows and have better safety records in older adults.
3. Diphenhydramine (Benadryl®) and Other First-Gen Antihistamines
It’s in sleep aids, allergy pills, cold medicines, and even some stomach remedies. Diphenhydramine is everywhere. But it’s also one of the most dangerous drugs for seniors.
It’s strongly anticholinergic-meaning it blocks a brain chemical called acetylcholine that’s vital for memory, focus, and muscle control. Long-term use increases dementia risk by 54%. A 2015 JAMA study found that seniors who took diphenhydramine for more than three years had a significantly higher chance of developing Alzheimer’s.
It also causes dry mouth, constipation, urinary retention, and blurred vision-all of which make falls more likely.
Better alternatives: For allergies, use loratadine (Claritin®) or cetirizine (Zyrtec®). For sleep, try melatonin or non-drug methods. For motion sickness, dimenhydrinate (Dramamine®) is still risky-better to use ginger or acupressure bands.
4. Nitrofurantoin (Macrobid®) for UTIs
It’s a common antibiotic for urinary tract infections. But for seniors with reduced kidney function-which is very common-it can cause serious lung damage.
Nitrofurantoin builds up in the body when kidneys can’t clear it. That leads to pulmonary toxicity: coughing, shortness of breath, fever, and sometimes fatal lung inflammation. The risk jumps 12.8 times in seniors with an eGFR below 60.
Many doctors still prescribe it because it’s cheap and widely available. But it’s not worth the risk.
Better alternatives: Fosfomycin or cephalexin. Both are safer for older adults with kidney issues. Always check kidney function before prescribing any antibiotic.
5. Benzodiazepines (Valium®, Xanax®, Ativan®)
These are prescribed for anxiety, insomnia, or muscle spasms. But they slow down the central nervous system. In seniors, that means dizziness, memory loss, confusion, and a 48% higher chance of a car crash if they’re still driving.
Long-term use increases fall risk by 60%. Withdrawal can be deadly-seizures, hallucinations, extreme anxiety. And because they’re so addictive, many seniors stay on them for years without realizing the danger.
The 2023 Beers Criteria now lists benzodiazepines as inappropriate for insomnia in seniors. Period.
Better alternatives: For anxiety, SSRIs like sertraline or citalopram. For insomnia, CBT-I again. For muscle spasms, physical therapy or non-drug options like heat or massage.
What You Should Do: A Simple 3-Step Review
Don’t wait for a crisis. Take control now.
- Do a brown bag review. Gather every pill, vitamin, supplement, and over-the-counter medicine you or your loved one takes. Put them all in a bag. Bring them to the doctor or pharmacist. Don’t just say, “I take this.” Show them.
- Ask the Beers Criteria question. Ask: “Is this medication on the Beers Criteria list for seniors?” If they don’t know what you’re talking about, ask for a pharmacist’s opinion. Pharmacists are trained to catch these risks.
- Ask about alternatives. Don’t accept “it’s always been this way.” Ask: “Is there a safer option? What happens if we stop this?”
Many seniors don’t know their meds are risky. A Kaiser Family Foundation survey found 58% of seniors on high-risk drugs had no idea safer options existed. And only 32% said their doctor ever talked to them about the risks.
Who Can Help? The Right Team Makes All the Difference
You don’t have to do this alone.
Pharmacists are your best ally. Medication therapy management (MTM) programs are free for Medicare beneficiaries. They’ll sit down with you, review every pill, and suggest changes. Ask your pharmacy if they offer MTM.
Geriatricians specialize in senior health. If your doctor doesn’t have experience with aging patients, consider seeing one. They know which drugs to avoid and which ones actually work.
Clinical pharmacists in hospitals and clinics can help with complex cases. Studies show when they’re involved, high-risk medication use drops by nearly 35% in just six months.
What’s Changing? New Tools Are Making It Easier
In 2023, electronic health records like Epic and Cerner started auto-flagging Beers Criteria drugs when doctors try to prescribe them to seniors over 65. If you’re on Medicare, your pharmacy’s system may already warn the pharmacist before dispensing a risky drug.
The CMS launched a new program in January 2024 that ties 5% of Medicare Advantage payments to how well plans reduce high-risk prescriptions. That means health plans are now financially motivated to help you switch to safer options.
And the FDA? They’ve started requiring stronger warnings on labels. Glyburide now has a black box warning. Benzodiazepines have clearer warnings about fall risk.
Final Thought: It’s Not About Stopping Meds. It’s About Choosing Wisely.
This isn’t about cutting pills just because they’re old. It’s about matching the right drug to the right person at the right time. Sometimes, the best medicine is no medicine at all.
Many seniors feel better-not worse-after switching off risky drugs. They sleep better without zolpidem. They’re more alert without diphenhydramine. Their balance improves. Their memory clears. They stop falling.
Don’t assume your meds are safe just because your doctor prescribed them. Ask. Review. Switch if needed. Your life depends on it.
What is the Beers Criteria and why does it matter for seniors?
The Beers Criteria is a list of medications that are potentially inappropriate for older adults, especially those over 65. Developed by the American Geriatrics Society and updated every two years, it identifies drugs that carry higher risks of side effects like falls, confusion, kidney damage, or dementia in seniors. It matters because many of these drugs are still commonly prescribed, even though safer alternatives exist. Medicare plans and pharmacies use it to guide prescribing and coverage decisions.
Can I stop taking a high-risk medication on my own?
No. Stopping certain medications suddenly-especially benzodiazepines, antidepressants, or steroids-can cause dangerous withdrawal symptoms like seizures, severe anxiety, or rebound insomnia. Always talk to your doctor or pharmacist first. They can help you taper off safely, often over several weeks, and replace the drug with a safer option.
Are over-the-counter drugs safe for seniors?
Not always. Many OTC meds contain diphenhydramine, pseudoephedrine, or NSAIDs like ibuprofen-all of which carry serious risks for older adults. Even “natural” supplements like melatonin or valerian root can interact with prescription drugs. Always check with a pharmacist before taking anything new, even if it’s sold without a prescription.
How often should seniors have their medications reviewed?
At least once a year, but every 3-6 months is better if you’re on five or more medications or have recently been hospitalized. Medicare requires annual medication reviews for beneficiaries in its MTM program. If you’re seeing multiple doctors, ask for a coordinated review-each provider may not know what the others prescribed.
What should I bring to a medication review appointment?
Bring every pill bottle, including vitamins, supplements, and over-the-counter drugs. Include any patches, inhalers, or creams. Write down when and why you take each one. If you’re unsure, bring a list of the names and dosages. Don’t rely on memory. The more complete the picture, the better the advice you’ll get.
Next Steps: Take Action Today
If you’re caring for an older adult, schedule a brown bag review this week. Call your pharmacy and ask if they offer free medication therapy management. Ask your doctor if any of your meds are on the Beers Criteria list. Write down the names of your top three medications and look them up on the American Geriatrics Society’s website.
Don’t wait for a fall, a hospital visit, or a memory lapse to act. The safest medicine is the one you never needed to take in the first place.

All Comments
shreyas yashas November 21, 2025
I never realized how many OTC meds are basically landmines for my mom. I thought Benadryl was harmless-turns out it’s basically a dementia accelerator. Time to do that brown bag review this weekend.
Suresh Ramaiyan November 23, 2025
It’s wild how medicine still treats older people like broken machines that just need more parts. We don’t fix a 30-year-old car by adding ten more fluids and ignoring the rust-we adjust. Why is aging treated differently? The Beers Criteria isn’t a suggestion-it’s a wake-up call.
Katy Bell November 24, 2025
My grandma was on glyburide for 8 years. One day she passed out at the grocery store. No one told us it was the med. They just said she "got weak with age." 😔 I wish I’d known this sooner.
Ragini Sharma November 25, 2025
so like… diphenhydramine = bad? but wait, isn’t that in every sleep aid?? like… why do they even sell it?? 😭 also i just took one last night for my allergies… oops??
Dalton Adams November 27, 2025
Let’s be honest-this article is basic. The Beers Criteria has been around since 1991. If your doctor doesn’t know it, they’re either lazy or unqualified. Also, CBT-I? Of course it works better than pills. But most people want a magic bullet, not behavioral change. That’s why we’re in this mess. 🤦♂️
Kane Ren November 29, 2025
This is exactly the kind of info we need to spread. My dad switched off zolpidem and started walking before bed-now he sleeps like a baby and hasn’t fallen in a year. Small changes, huge impact. You got this, seniors!
Charmaine Barcelon November 29, 2025
Stop giving seniors drugs. Just stop. They’re too old to handle them. Let them die naturally. No one needs to be on 10 pills. It’s just laziness. Doctors are too busy. Pharmacies are too greedy. It’s obvious.
Karla Morales November 30, 2025
⚠️ This is a public health emergency. The systemic failure here is catastrophic. Polypharmacy is not a side effect-it’s a structural flaw in geriatric care. The CDC data is underreported. The FDA’s warnings are toothless. We need policy reform, not blog posts. 🚨
Javier Rain December 1, 2025
My aunt was on benzodiazepines for 15 years. She didn’t even know she was addicted. We got her off it with a slow taper and now she’s hiking again. It’s not easy-but it’s worth it. Don’t wait for a fall. Start the conversation today.
Laurie Sala December 3, 2025
I just lost my mom to a fall. They said it was "just age." But I found the Ambien bottle under her bed. I know. I know. I should’ve checked sooner. I’m so sorry. I’m so sorry. I’m so sorry.
Lisa Detanna December 3, 2025
In my culture, elders are respected. But here? We treat them like medical projects. We don’t listen. We just prescribe. This article is a gift. Thank you. Let’s change how we see aging-not just how we dose it.
Richard Wöhrl December 5, 2025
One thing missing: the role of pharmacists. Most people don’t realize pharmacists are trained to catch dangerous interactions. Ask for a Medication Therapy Management (MTM) session-it’s free with Medicare. I’ve seen 3 seniors avoid hospitalization just because they got a 30-minute med review. It’s that simple.
Pramod Kumar December 6, 2025
My uncle took diphenhydramine for years-he thought it was "just for allergies." Then he started forgetting his own birthday. We switched him to Claritin. Three months later? He remembered his wedding anniversary. I swear to god, that stuff is a brain fog grenade. Don’t let your elders take it.
Brandy Walley December 7, 2025
Why are we acting like seniors are fragile glass animals? Maybe they just need to stop being so lazy. If they exercised more and ate better, they wouldn’t need all these pills. This is just fear-mongering dressed up as care.
Kezia Katherine Lewis December 9, 2025
From a clinical pharmacology standpoint, the Beers Criteria represents a necessary but insufficient intervention. The real issue lies in fragmented care coordination and the absence of longitudinal pharmacovigilance in outpatient geriatric populations. Without EHR integration and standardized deprescribing protocols, awareness alone will not reduce polypharmacy-related morbidity.