When your MS symptoms suddenly get worse, it’s natural to panic. Did another relapse hit? Is your disease progressing? But here’s the thing: not every spike in symptoms means your MS is actively attacking your nervous system. Many times, it’s something called a pseudorelapse - a temporary flare-up with no new damage, no inflammation, and no need for steroids. Mistaking one for the other isn’t just confusing - it can be dangerous.
What’s Really Happening When Symptoms Get Worse?
A true MS relapse is when your immune system launches a new attack on the myelin sheath around your nerves. This causes fresh inflammation, new lesions on your MRI, and symptoms that last at least 24 to 48 hours without any obvious outside cause. These can include sudden vision loss, leg weakness, balance problems, or numbness that didn’t exist before. If you’ve had MS for years, you know how unsettling this feels - and you’ve probably been through it before. But here’s what most people don’t realize: up to a quarter of symptom flares aren’t relapses at all. They’re pseudorelapses. These aren’t caused by new damage. They’re caused by your body being under stress. Your nerves, already damaged from past MS attacks, are struggling to send signals. When something heats you up, gives you an infection, or pushes you too hard, those damaged pathways just can’t keep up. The result? Symptoms that feel exactly like a relapse - but they’re temporary.Heat, Infections, and Stress: The Real Triggers Behind Pseudorelapses
If you’ve ever stepped out of a hot shower and suddenly couldn’t see clearly, you’ve experienced Uhthoff’s phenomenon. That’s a classic pseudorelapse. About 60 to 80% of people with MS who’ve had optic neuritis get this. Your vision blurs, your muscles feel heavy, your coordination slips - all because your body temperature rose just a degree or two. No new lesions. No inflammation. Just your nerves temporarily failing under heat stress. But heat isn’t the only trigger. Infections are the biggest culprit. Urinary tract infections (UTIs) trigger pseudorelapses in nearly two out of every three cases. A cold, the flu, even a mild sinus infection can do it. Fever raises your core temperature, and suddenly, symptoms you thought were under control come roaring back. Physical exhaustion, emotional stress, and even extreme fatigue can do the same thing. One patient on MyMSTeam shared: “I thought I was having a relapse when my legs gave out. Turned out I had a UTI. Took antibiotics, cooled down, and within hours, I was walking again. No steroids needed.” That’s the difference.Why Steroids Don’t Work for Pseudorelapses - and Why They’re Risky
High-dose steroids like IV methylprednisolone are the go-to treatment for true MS relapses. They reduce inflammation, shorten the flare, and help you recover faster. About 70 to 80% of true relapses improve with steroids. But here’s the catch: steroids do nothing for pseudorelapses. Why? Because there’s no inflammation to calm down. Giving steroids for a pseudorelapse is like using a fire extinguisher on a steamy mirror. It doesn’t fix the problem - it just adds new ones. Studies show that around 30 to 40% of patients get unnecessary steroids for pseudorelapses. And the side effects? They’re real. One in four people develop high blood sugar. Four in ten get severe insomnia. Three in ten report mood swings, anxiety, or even panic attacks. Some end up in the hospital with steroid-induced psychosis - not because their MS got worse, but because they were treated for the wrong thing. A nurse with MS on Reddit wrote: “I’ve seen five patients get IV steroids for UTIs. One developed hallucinations. They didn’t need steroids. They needed antibiotics and rest.”
How to Tell the Difference - A Simple 3-Step Check
You don’t need an MRI or a neurologist to start ruling out a pseudorelapse. Here’s what to do the moment symptoms worsen:- Check your temperature. If you have a fever above 100.4°F (38°C), it’s likely a pseudorelapse. Infections are the #1 trigger.
- Look for recent triggers. Did you take a hot bath? Get caught in the sun? Run errands all day? Skip a meal? Feel overwhelmed? These are red flags.
- Wait 24 hours. True relapses don’t vanish quickly. If your symptoms start fading after you cool down, rest, or treat a UTI - it’s not a relapse.
What to Do When It’s a Pseudorelapse
The good news? Pseudorelapses don’t cause permanent damage. You won’t accumulate disability from them. The key is managing the trigger. - For heat: Use cooling vests, stay in air-conditioned spaces, drink cold fluids, avoid hot tubs and saunas. A study showed patients using cooling gear recovered in under two hours. - For infections: Treat UTIs early. Drink water, pee frequently, don’t ignore burning or urgency. A simple urine test can catch it before symptoms flare. - For stress and fatigue: Rest. Say no. Schedule downtime. Burnout doesn’t just make you tired - it makes your MS symptoms worse. Many patients keep a symptom diary. Write down what happened the day before the flare: Did you get sick? Were you hot? Did you sleep poorly? This helps you spot patterns. One woman in Exeter told me she noticed every time she skipped her morning coffee, her hands trembled more. Turns out, caffeine withdrawal was triggering her pseudorelapses.Who’s Most at Risk - and Why It Matters
Pseudorelapses become more common the longer you’ve had MS. That’s not because your disease is worse - it’s because you’ve accumulated more nerve damage. Those damaged pathways are more sensitive to stress. People over 55 with significant disability are especially vulnerable. One study found 15% of older patients didn’t fully bounce back after a pseudorelapse - not because of MS progression, but because they got too weak from the episode and didn’t recover their mobility. Also, people with progressive MS are more likely to experience pseudorelapses than true relapses. That’s because active inflammation slows down over time, but the damage stays. So even if your relapses are fewer, your symptoms can still spike - and you need to know why.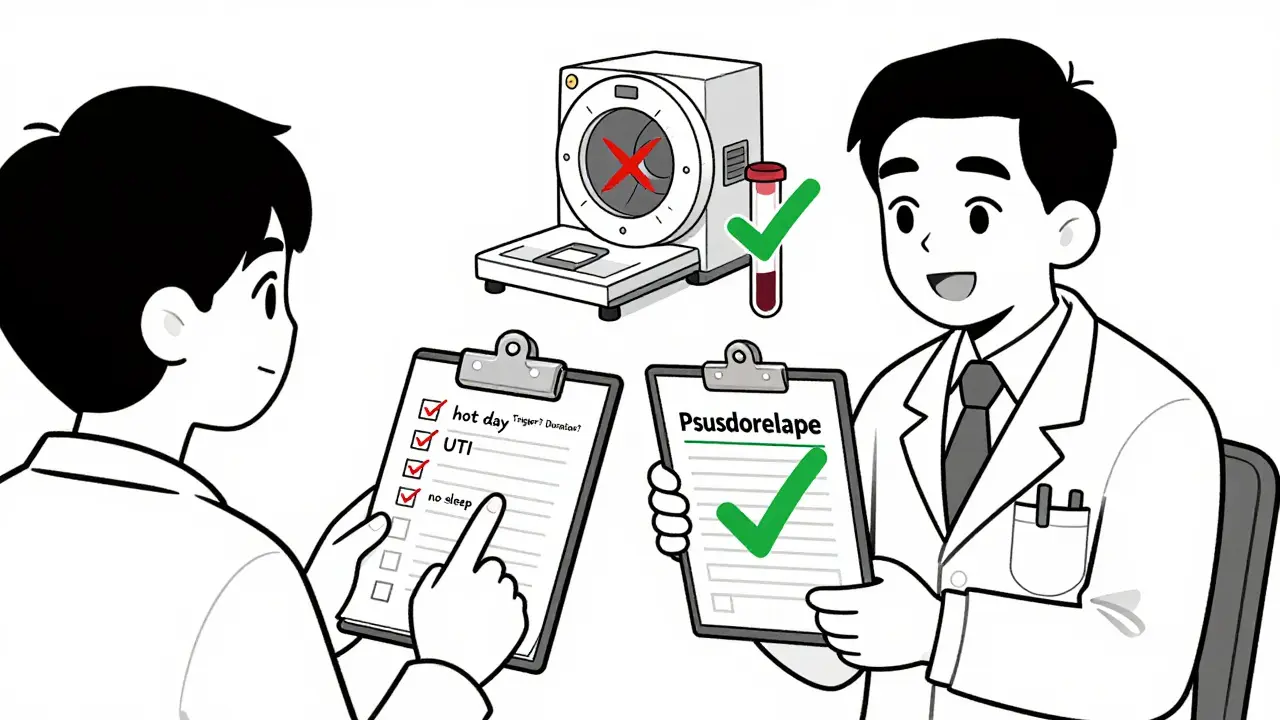
What’s New in Diagnosis - and Why It’s Better
A new tool called the MS-Relapse Assessment Tool (MS-RAT) is changing the game. It asks you questions about symptom duration, temperature changes, and how much your daily life is affected. It gives you a score - 92% accurate at telling true relapses from pseudorelapses. Some telehealth platforms now use it to help patients decide whether to go to the ER or just rest at home. Research is also looking at blood tests. Neurofilament light chain levels - a marker of nerve damage - rise during true relapses but stay normal in pseudorelapses. That could mean one simple blood test will soon replace the need for an MRI in many cases.Don’t Let Fear Drive Your Treatment
Too many people rush to steroids because they’re scared. But steroids aren’t a cure. They’re a tool - and only the right tool for the right problem. Treating a pseudorelapse like a relapse doesn’t help. It hurts. If you’ve had a pseudorelapse before, you know the relief when you realize: this isn’t my MS getting worse. It’s my body asking for rest. Cooling down. Drinking water. Treating that infection. Sometimes, the best medicine isn’t a needle - it’s a cold towel, a quiet room, and a good night’s sleep.When to Call Your Neurologist
Call your neurologist if:- Symptoms last more than 48 hours
- You can’t identify a clear trigger
- Your symptoms are new, severe, or affect your ability to walk, see, or control your bladder
- You’ve had two or more flares in the last three months
Can a pseudorelapse turn into a true relapse?
No. A pseudorelapse is not a warning sign that a true relapse is coming. It’s a separate event caused by temporary stress on damaged nerves. However, if you’re frequently experiencing pseudorelapses, it may mean your MS is progressing and your nervous system is more vulnerable - which is why tracking triggers and working with your neurologist matters.
Do I need an MRI every time my symptoms get worse?
Not always. If you’ve had a clear trigger - like a fever, hot weather, or a UTI - and your symptoms improve within 24 hours, an MRI isn’t needed. But if symptoms persist, worsen, or you can’t find a trigger, an MRI helps confirm whether there’s new inflammation. Your neurologist will guide you based on your history.
Are steroids ever used for pseudorelapses?
No, and they shouldn’t be. Steroids treat inflammation - which isn’t present in a pseudorelapse. Giving them is unnecessary and risky. Side effects like high blood sugar, insomnia, mood swings, and infections can be serious. The goal is to treat the trigger, not suppress inflammation that doesn’t exist.
Can stress really cause MS symptoms to flare?
Yes. Stress doesn’t cause MS, but it can trigger pseudorelapses. When you’re stressed, your body releases hormones like cortisol that raise your core temperature and affect nerve signaling. For someone with damaged nerves, this is enough to cause temporary weakness, tingling, or fatigue. Managing stress through rest, breathing exercises, or therapy can reduce these flares.
Is it normal for pseudorelapses to last more than a day?
Usually not. Most pseudorelapses resolve within hours to a day after removing the trigger. If symptoms last longer than 48 hours, it’s more likely a true relapse. But in rare cases, especially in older patients with high disability, recovery can take longer due to deconditioning - not because of new MS damage. That’s why staying active during recovery is important.

All Comments
Ryan Pagan January 29, 2026
Let me tell you something - I’ve been MSing for 12 years and I’ve seen more pseudorelapses than actual relapses. Steroids? Nah. I’ve got a cooling vest, a water bottle labeled ‘MS Survival Juice,’ and a strict no-hot-shower rule. Last month, I got a UTI, felt like I was falling apart, and panicked. Turned out? Just a little E. coli and a 101°F fever. Antibiotics, ice pack, and three hours of sleep - boom, walking again. No IV, no side effects, no drama. Your body’s not broken - it’s just tired. Listen to it.
Eli In January 30, 2026
Thank you for this. I’m a Filipina-American with MS and I’ve had relatives tell me I’m ‘just being dramatic’ when I can’t walk after a hot day. This post validates what so many of us live with daily. 💙 I keep a little notebook: ‘Heat? Check. Fever? Check. Stress? Triple check.’ It’s not weakness - it’s adaptation. 🌿
Paul Adler January 31, 2026
Interesting how the medical system defaults to steroids because it’s easier than asking questions. I’ve worked in neurology for 18 years. The real challenge isn’t diagnosis - it’s convincing patients not to fear their own bodies. A pseudorelapse isn’t failure. It’s feedback. Your nervous system is screaming, ‘Hey, I need rest!’ And we treat it like a glitch to fix - not a signal to honor.
Sheryl Dhlamini February 1, 2026
I had a pseudorelapse last week after binge-watching Netflix in a 90°F apartment. Felt like I was drowning in my own legs. Called my neurologist - she laughed and said, ‘Go drink water, turn on the AC, and don’t text me until tomorrow.’ I did. And by morning? I was fine. No steroids. No guilt. Just… life.
kabir das February 1, 2026
I’ve been waiting for someone to say this... I knew it... I KNEW IT...!!! The pharmaceutical industry doesn’t want you to know this... They profit from steroids... They profit from MRIs... They profit from fear... And now... now I’m not alone... 😭
ryan Sifontes February 2, 2026
i think this is all just a distraction from the real issue. why are we even talking about pseudorelapses? maybe ms is just a symptom of modern life. wifi. processed food. too much screen time. steroids are just a bandaid. we need systemic change. also i think my cat is judging me.
DHARMAN CHELLANI February 3, 2026
lol steroids? more like steriods. you guys act like this is rocket science. its not. if your legs are weak after a hot shower, you’re not having a relapse. you’re having a ‘oops i forgot to drink water’ moment. fix the water, not your immune system.
rajaneesh s rajan February 5, 2026
Let’s be real - pseudorelapses are just MS’s way of saying, ‘Hey, you’ve been ignoring your body for 3 years straight. Time to chill.’ I used to push through fatigue like a superhero. Now? I nap like it’s my job. And guess what? I haven’t had a true relapse in 18 months. Coincidence? Nah. My body’s finally getting the memo.
Megan Brooks February 7, 2026
There’s a quiet dignity in learning to distinguish between damage and discomfort. A true relapse is a storm - violent, unpredictable, and structural. A pseudorelapse is a ripple - caused by the wind, the heat, the weight of a long day. We don’t need to extinguish ripples. We need to learn how to sit with them. And sometimes, that’s the bravest thing we can do.
Jasneet Minhas February 9, 2026
OMG I just realized my morning coffee withdrawal triggers my hand tremors 😱 I’ve been blaming MS for 2 years. Turns out it’s just my caffeine addiction being dramatic. Also, I’m now carrying a tiny fan in my purse. #MSHacks #SarcasticButTrue 🍵🪩
Pawan Kumar February 10, 2026
It is, of course, entirely unsurprising that the medical establishment - steeped in reductionist paradigms and pharmacological dogma - continues to misdiagnose pseudorelapses as relapses. This is not merely a clinical error; it is a systemic epistemological failure. One must question: if the diagnostic framework is rooted in outdated neuroimmunological models, how can we expect accurate patient outcomes? The reliance on MRI as the sole arbiter of truth is a form of scientistic idolatry. The body, in its phenomenological richness, cannot be reduced to lesions on a screen. We must, therefore, embrace a hermeneutic approach - one that listens, observes, and contextualizes. Steroids? A crude instrument. A sledgehammer to a hummingbird’s nest.
Doug Gray February 11, 2026
Interesting. The ontological distinction between relapse and pseudorelapse hinges on a binary that may itself be epistemologically unstable. If symptomatology is identical, and the only differentiator is the presence of inflammatory markers - which themselves are probabilistic constructs - then isn’t the entire taxonomy a social artifact? We’re pathologizing homeostatic stress responses under the guise of neuroimmunology. The real question isn’t ‘Is this a relapse?’ - it’s ‘Why are we so afraid of transient dysfunction?’
paul walker February 11, 2026
This post saved my life. I was about to go to the ER for steroids. Now I’m drinking water, turning on the AC, and taking a nap. You’re all my heroes. 🙌💙