When chronic pain won’t go away, pills and physical therapy often aren’t enough. That’s when many patients turn to nerve blocks and radiofrequency ablation (RFA)-two interventional pain procedures that target the source of pain, not just the symptoms. These aren’t surgeries. They’re precise, minimally invasive treatments done in outpatient settings, often with just local anesthesia and mild sedation. But they’re not the same. Understanding the difference can make all the difference in your pain relief journey.
How Nerve Blocks Work (And When They Help)
A nerve block is exactly what it sounds like: a doctor injects medication-usually a local anesthetic like lidocaine, sometimes combined with a steroid-right next to a nerve that’s sending pain signals to your brain. The goal? To temporarily block those signals. Think of it like hitting pause on pain.
It’s fast. The procedure takes about 10 to 20 minutes. You’re awake, maybe a little drowsy from light sedation. You’ll feel a small pinch when the needle goes in, then a warm sensation as the medicine spreads. Within minutes, the area that’s been hurting for months might feel numb or completely pain-free.
But here’s the catch: that relief doesn’t last. Most nerve blocks offer hours to a few weeks of relief. For some people with acute flare-ups-like a sudden pinched nerve or post-surgical pain-that’s enough. For others with chronic conditions like arthritis or spinal facet joint pain, it’s just a temporary fix.
That’s why nerve blocks are often used as a diagnostic tool. If you get 80% or more pain relief after a nerve block, it tells your doctor: Yes, this nerve is the problem. If you don’t feel much difference? Then the pain is coming from somewhere else. That’s critical. You don’t want to go ahead with a more involved procedure like RFA if the nerve block didn’t work.
What Is Radiofrequency Ablation (RFA)?
RFA is where things get more permanent. Instead of temporarily numbing the nerve, RFA uses heat to disable it. A thin needle, guided by real-time X-ray imaging (fluoroscopy), is placed right next to the nerve causing pain. Then, a small electrical current is sent through the needle, heating the tip to between 80°C and 90°C. That heat creates a tiny lesion on the nerve-just big enough to stop it from sending pain signals.
It’s not destroying the nerve permanently. Nerves can regenerate over time, which is why relief typically lasts 6 to 24 months. But for many, that’s a game-changer. You’re not curing arthritis or degenerative disc disease. You’re cutting off the pain signal it produces.
The procedure takes 20 to 45 minutes, depending on how many nerves are treated. You’re awake, but you won’t feel the heat because the area is numbed. Before the heat is applied, your doctor will test the needle’s position by sending small electrical pulses. You’ll feel a tingling or muscle twitch-this confirms the needle is touching the right nerve and not a motor nerve that controls movement.
Afterward, you might feel soreness or aching at the injection site for a few days. That’s normal. Full pain relief usually builds over 2 to 4 weeks as the nerve fully stops sending signals. Most people are back to light activity within 24 hours and back to work in 2 to 3 days.
Why RFA Beats Nerve Blocks for Long-Term Relief
Let’s compare them side by side.
- Nerve blocks: Lasts hours to weeks. Good for diagnosis or short-term flare-ups. Low cost, low risk.
- RFA: Lasts 6 to 24 months. Good for chronic pain that hasn’t responded to other treatments. Higher upfront cost, but fewer repeat procedures needed.
According to data from the Hospital for Special Surgery, RFA works for 70% to 80% of patients with chronic low back pain from facet joints. That’s significantly higher than the 30% to 50% success rate you see with repeated nerve blocks over time.
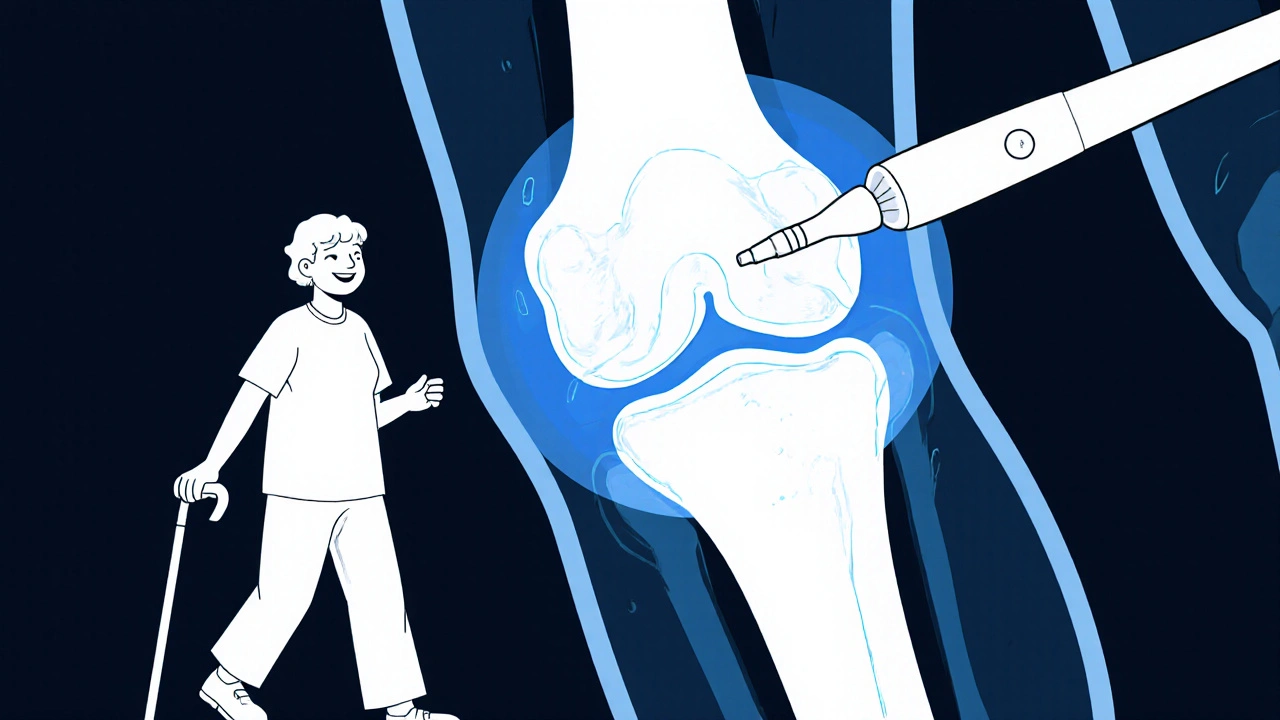
For knee osteoarthritis, a 2023 study showed that cooled RFA-using a special electrode that creates a larger treatment zone-helped 65% of patients maintain pain relief for six months. Standard cortisone injections? Only 45% saw improvement at three months.
And compared to surgery? RFA is a no-brainer. Spinal fusion requires weeks of recovery, carries a 10% to 15% risk of complications, and costs $20,000 to $50,000. RFA? Around $3,000 to $5,000. Outpatient. No general anesthesia. No hospital stay.

Who Is a Good Candidate for RFA?
Not everyone qualifies. The biggest rule? You must have had a successful diagnostic nerve block first. If you didn’t get at least 80% pain relief from that initial injection, RFA is unlikely to help. That’s not just a suggestion-it’s standard practice backed by the Spine Intervention Society and the American Society of Anesthesiologists.
Good candidates usually have:
- Chronic low back or neck pain from facet joints
- Knee osteoarthritis that hasn’t responded to physical therapy or injections
- Sacroiliac joint pain
- Occipital neuralgia (headaches from irritated nerves at the base of the skull)
- Plantar fasciitis that won’t quit
Age matters too. People between 45 and 65 with degenerative joint changes respond best. Younger patients often have pain from injury or inflammation, which may respond better to other treatments. Older patients may have too many other health issues to be ideal candidates.
And if you’re on opioids? RFA can help you cut back-or even stop. One study from Gardner Orthopedics found 70% of patients reduced or eliminated opioid use after RFA.
What About Pulsed RFA and Newer Technologies?
Traditional RFA uses heat. But there’s a newer version called pulsed radiofrequency (PRF). Instead of heating the nerve to 80°C, PRF sends short bursts of high-voltage energy. It doesn’t destroy the nerve-it just resets how it sends pain signals. Think of it like rebooting a glitchy computer.
PRF is great for people who can’t tolerate heat, like those with sensitive nerves or who’ve had complications before. It’s also being used for conditions like trigeminal neuralgia and chronic headaches. Recovery is faster, and there’s almost no risk of nerve damage. But the relief doesn’t last as long-usually 3 to 6 months.
Then there’s cooled RFA. This uses a special needle that circulates coolant around the tip, allowing a larger area of nerve tissue to be treated without burning surrounding tissue. It’s especially useful for bigger nerves, like those around the knee. Studies show cooled RFA gives longer-lasting relief than traditional RFA for knee pain.
In 2022, the FDA approved the first pulsed-field ablation system for spinal pain. It uses electrical pulses instead of heat to disrupt nerves. Early results show faster recovery and less post-procedure soreness. It’s still new, but it’s the next step forward.
What Are the Risks?
RFA and nerve blocks are both low-risk. But nothing’s risk-free.
The most common side effect? Temporary soreness at the injection site. It usually fades in 3 to 7 days. Some people get a brief flare-up of pain-called neuritis-where the nerve becomes irritated. That lasts about 1 to 2 weeks and responds well to ice and over-the-counter painkillers.
Bigger risks are rare. Infection happens in less than 1% of cases. Nerve damage that causes numbness or weakness is extremely uncommon-especially when done by an experienced provider using real-time imaging. The biggest mistake? Treating the wrong nerve. That’s why the diagnostic block is non-negotiable. Without it, about 20% to 30% of RFA procedures don’t work.
And if you have a pacemaker or other implanted device? Tell your doctor. Some RFA equipment can interfere with those devices.
What Happens After the Procedure?
You’ll go home the same day. No driving for 24 hours. Rest the first day. Light walking is encouraged. Avoid heavy lifting or strenuous activity for 48 hours.
Don’t expect instant relief. Pain relief builds over time. Some people feel better in a week. Others take 3 to 4 weeks. That’s because the nerve needs time to fully stop sending signals after being heated.
Keep a pain diary. Note when the relief starts, how strong it is, and if anything triggers a return of pain. That info helps your doctor decide if and when you might need another RFA.
Most patients return to normal activity within 2 to 3 days. Many say they can finally sleep through the night, walk without a cane, or play with their grandkids again.
Is RFA Right for You?
If you’ve tried physical therapy, NSAIDs, and steroid injections-and you’re still in pain-RFA might be your next step. But only if you’ve had a successful diagnostic nerve block.
It’s not a cure. You still have arthritis. You still have degenerated discs. But you don’t have to live with the pain they cause.
It’s also not a last resort. The American Society of Anesthesiologists now recommends RFA as a standard second-line treatment after conservative therapies fail-before you even consider surgery.
And with the global RFA market growing at 14.3% per year, it’s clear: more people are choosing it. More doctors are offering it. More insurance plans are covering it.
If you’re tired of pain controlling your life, ask your pain specialist: Have I had a proper diagnostic nerve block? Am I a candidate for RFA? That simple question could change everything.
How long does pain relief last after RFA?
Pain relief from radiofrequency ablation typically lasts between 6 and 24 months, depending on the nerve treated, the type of RFA used (traditional vs. cooled), and individual healing factors. Most patients experience 6 to 12 months of significant relief, with some lasting up to two years. Nerves gradually regenerate over time, which is why the procedure can be repeated if pain returns.
Is RFA better than a nerve block?
It depends on your goal. Nerve blocks offer short-term relief (hours to weeks) and are best for diagnosing pain sources or managing flare-ups. RFA provides longer-lasting relief (6-24 months) by disabling the nerve’s ability to send pain signals. If you’ve had a successful diagnostic nerve block and want lasting relief without surgery, RFA is the better option.
Does RFA hurt?
The procedure itself isn’t painful. The area is numbed with local anesthetic, and most patients report only mild pressure or a warm sensation during the treatment. Afterward, you may feel soreness or achiness at the injection site for a few days-similar to a muscle strain. Most people manage this with ice and over-the-counter pain relievers.
Can RFA be done on the knee?
Yes. Cooled radiofrequency ablation is now a proven treatment for knee osteoarthritis. It targets the genicular nerves that carry pain signals from the knee joint. Studies show 65% of patients experience significant pain relief for at least six months, compared to 45% with steroid injections at three months. It’s a non-surgical alternative for those who can’t or don’t want joint replacement.
Will I need to take opioids after RFA?
Many patients reduce or stop opioid use after successful RFA. One study found that 70% of patients were able to lower or eliminate their opioid intake because their pain was better controlled. RFA doesn’t cure the underlying condition, but it removes the constant pain signal that often leads to long-term medication dependence.
What if RFA doesn’t work for me?
If RFA doesn’t help, it’s likely because the wrong nerve was targeted-often because the diagnostic nerve block wasn’t done properly or the pain source wasn’t clearly identified. Other options include pulsed RFA, spinal cord stimulation, or physical therapy focused on neuromodulation. Your doctor will reassess your pain pattern and explore alternatives based on your specific condition and response history.
All Comments
John Power November 28, 2025
I had RFA on my lower back last year after years of steroid shots that barely helped. First week was sore as hell, but by week three I was walking my dog without wincing. Now I can play with my grandkids without needing a nap afterward. Seriously changed my life. 🙌
Richard Elias November 29, 2025
nerve blocks are a scam. if u dont get instant relief its a waste of time. rfa is the only real fix. i had 3 nerve blocks and still couldnt tie my shoes. rfa? 2 weeks later i was lifting weights again. dont waste ur money on temp fixes.
Scott McKenzie December 1, 2025
Just want to add a quick note for anyone thinking about cooled RFA for knee pain - it’s a game changer. I had it done last fall and still going strong at 11 months. The doc used the 8mm probe and it felt like a miracle. Also, make sure your provider is certified in genicular nerve ablation. Not all clinics do it right. 💪
Jeremy Mattocks December 2, 2025
Let me tell you why so many people get disappointed with RFA - they don’t understand the timeline. It’s not like popping a pill and feeling better in 20 minutes. The nerve doesn’t just shut off overnight. It takes weeks for the inflammation to settle and for the axons to fully stop firing. I had mine done in January and didn’t feel real relief until late February. If you give up at day 10, you’re quitting too early. Patience isn’t optional here - it’s part of the treatment. And yeah, the soreness sucks for a few days, but it’s the kind of soreness that says ‘your body is healing, not breaking.’
Jill Ann Hays December 2, 2025
The fundamental flaw in this entire paradigm is the assumption that pain is a signal rather than a system. Nerve blocks and RFA are merely bandages on a broken feedback loop. The body doesn't malfunction because of a single nerve it malfunctions because of chronic stress inflammation and poor movement patterns. Fix the system not the symptom
Mike Rothschild December 2, 2025
Agree with Jill but let me add this - if you’ve tried everything and still hurting RFA is the smartest next move. I was on opioids for 5 years. After RFA I cut my dose in half in 3 months. Now I’m off them entirely. It’s not magic but it’s science. And it works. Don’t let fear stop you from asking your doctor about it.
Ron Prince December 3, 2025
Why are we letting some hippie doc stick needles in our spine like its yoga? In my day we worked through pain. Now everyone wants a quick fix. You think your spine is fragile? Get off the couch and lift something heavy. Real men don’t need RFA they need discipline.
King Splinter December 4, 2025
So let me get this straight - you’re telling me that if I pay $5k I can numb a nerve for 2 years instead of taking a pill every day? That’s it? That’s the big innovation? We’re paying for temporary relief because the medical system won’t fix the root cause. And don’t even get me started on how they upsell you on cooled RFA like it’s the latest iPhone. Meanwhile my insurance won’t cover physical therapy. Classic.
Kristy Sanchez December 5, 2025
Oh wow so RFA is the answer? Cool. So what happens when your nerve regenerates and the pain comes back? Do you just get it done again? And again? And again? Like a hamster on a wheel? Meanwhile your body is slowly turning into a collection of scar tissue and dead nerves. You’re not curing anything. You’re just outsourcing your pain to a needle. 🤡
Jerrod Davis December 6, 2025
It is imperative to underscore that the efficacy of radiofrequency ablation is contingent upon the precision of diagnostic nerve block localization. Without rigorous adherence to standardized protocols the procedural outcome is statistically compromised. Furthermore the potential for iatrogenic neural injury necessitates a comprehensive preoperative risk-benefit analysis.
Dominic Fuchs December 6, 2025
People treat pain like it's a bug to be deleted but it's more like a warning light. RFA turns off the light but the engine's still overheating. I had it done. Felt great for 14 months. Then the pain crept back. Now I'm doing mobility work and yoga. Turns out the body doesn't like being ignored just because a nerve got zapped
Asbury (Ash) Taylor December 8, 2025
For anyone reading this and feeling overwhelmed - you’re not alone. I was terrified before my RFA. Thought I’d be stuck with needles forever. But the team walked me through every step. I cried after the procedure - not from pain but from relief. I slept through the night for the first time in 7 years. This isn’t just a procedure. It’s a second chance. Don’t rush it. Don’t skip the diagnostic block. And don’t give up. You’ve already survived 100% of your worst days. This is just the next one.