When your knees ache after walking the dog, or your fingers stiffen up in the morning, it’s easy to brush it off as just getting older. But osteoarthritis isn’t normal aging-it’s a disease. And it’s more common than you think. Right now, over 500 million people worldwide live with it. In the U.S. alone, nearly one in eight adults has been diagnosed. It doesn’t just hurt-it limits your life. You stop climbing stairs. You skip walks. You avoid gripping your coffee mug. And if you’re not careful, it can start pulling other health problems along with it-obesity, heart disease, diabetes.
What’s Really Happening in Your Joint?
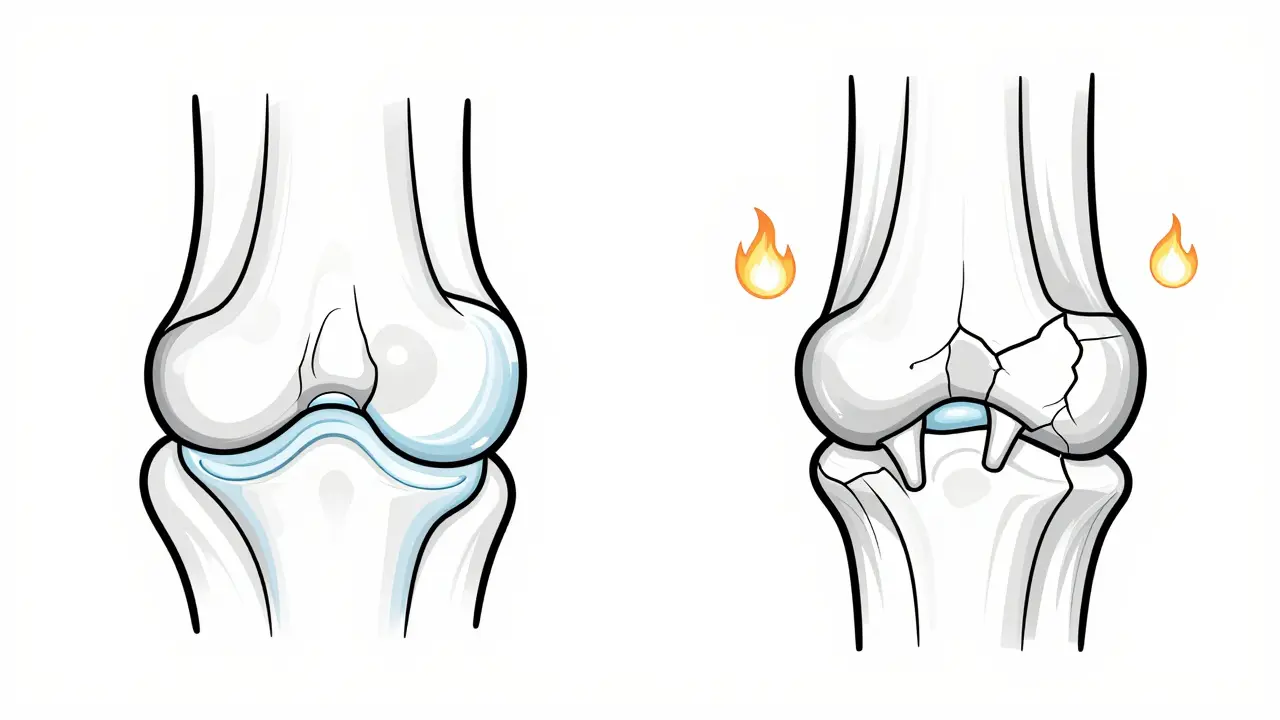
Most people think osteoarthritis is just cartilage wearing away like an old tire. But that’s outdated. Modern science sees it as a whole-joint disease. The cartilage? Yes, it breaks down. But so do the bones underneath. Ligaments loosen. The synovial fluid thickens. Even the fat around the joint starts releasing inflammatory chemicals. It’s not just friction-it’s a chemical fire inside your joint. The earliest damage starts with tiny cracks in the cartilage surface. Then, the cells inside (chondrocytes) go into overdrive, trying to repair it. But they can’t keep up. Instead of healing, they start making enzymes that chew up more cartilage. Bone responds by growing extra spurs-osteophytes-that you can see on X-rays. And because the joint isn’t moving smoothly anymore, inflammation sticks around. That’s why pain gets worse with activity and doesn’t fully go away even when you rest. Knees are the most common trouble spot-60% of cases. Then hips, hands, and spine. It usually hits one side harder than the other. That’s a clue: if both knees hurt equally, it might be something else. Osteoarthritis doesn’t wake you up at 3 a.m. like rheumatoid arthritis does. Its pain comes with movement, eases with rest. But over time, even resting doesn’t help as much.Why You’re More Likely to Get It (And What You Can Do)
You can’t change your age. But you can change other risks. The biggest one? Weight. Every extra pound puts four times the pressure on your knees. Lose 10% of your body weight, and studies show pain drops by up to 50%. That’s more than most pills can do. Another big factor? Past injury. A torn ACL from your 20s? That doesn’t just heal-it sets the stage for OA decades later. That’s why athletes and construction workers have higher rates. Even repetitive motions, like typing or playing violin, can add up. Women are more affected than men-60% of cases. Why? Hormones, joint shape, and muscle strength all play a role. Women also get more hand and knee OA; men get more severe hip OA. And it’s not just about being older. CDC data shows OA is rising fastest in people under 50, mostly because of obesity and lack of movement.The Real Pain Management Game: Three Pillars
There’s no magic cure. But there are proven ways to take control. The American College of Rheumatology says you need at least three of these to make a real difference:- Weight management - Even 5-10% loss helps. It doesn’t have to be extreme. Just moving more and eating less processed food.
- Structured exercise - Not just walking. You need strength training (quads and glutes for knees), flexibility (yoga or stretching), and low-impact cardio (cycling, swimming). The Arthritis Foundation found that 80% of people who did 45 minutes, three times a week, saw real pain reduction after 12 weeks.
- Physical therapy - A certified therapist teaches you how to move without hurting. They show you joint protection tricks-like using your arms to open jars instead of twisting your wrists. Six to eight sessions can change how you live.
What About Medications and Injections?
NSAIDs like ibuprofen are common, but they’re not the answer for long-term use. One in three people quit because of stomach issues or high blood pressure. And they don’t slow down the damage-just mask the pain. Intra-articular corticosteroid injections? They’re back in favor. OARSI’s 2023 guidelines say they’re one of the best options for sudden knee flare-ups. Studies show they cut pain by half for about four weeks. Good for getting you back on your feet. But not a permanent fix. Do them too often, and you risk cartilage damage. Newer drugs like tanezumab (FDA-approved in 2023) target nerve growth factor. In trials, it reduced pain 35% more than NSAIDs. But it’s not for everyone-it’s reserved for moderate-to-severe cases when other treatments fail. Topical creams (capsaicin, diclofenac gel) can help for hands or knees. They have fewer side effects. And don’t forget heat and cold. Heat loosens stiff joints. Cold numbs swelling after activity.What Doesn’t Work (And What’s Still Experimental)
Glucosamine and chondroitin? Most studies show they don’t do much more than a placebo. The NIH’s large trial in 2021 found no significant benefit over sugar pills. Save your money. Stem cell therapy? It’s getting a lot of hype. There are nearly 400 active clinical trials right now. But right now, there’s no solid proof it regrows cartilage in humans. Some clinics charge thousands for injections with no FDA approval. Proceed with caution. PRP (platelet-rich plasma)? Mixed results. Some patients report relief. Others feel nothing. It’s not yet a standard recommendation. Surgery? Joint replacement is highly effective-90% of patients report major improvement. But it’s not a first-line option. Wait until pain controls your life, not the other way around.Real People, Real Results
On Reddit, a user named ‘KneePainSince40’ wrote: “I could barely walk 10 minutes. Then I lost 22 pounds and started physical therapy. Now I hike on weekends. No surgery. No pills.” The Arthritis Foundation’s 2022 survey of 1,200 people found:- 72% improved after losing 10% of body weight
- 68% said pain interrupted their sleep
- 57% struggled with stairs
- 42% couldn’t button shirts or open jars
The Hidden Cost
Osteoarthritis isn’t just a health issue-it’s an economic one. In the U.S., it costs $140 billion a year in medical bills and lost wages. Employers lose $3.4 billion annually because workers can’t lift, stand, or move like they used to. Forty-three percent of people with OA cut back on work. That’s not laziness-it’s physical limitation. And here’s the trap: pain makes you inactive. Less movement means weaker muscles, stiffer joints, and weight gain. That makes OA worse. Which makes you move less. It’s a spiral. Breaking it means starting small. A 10-minute walk. Two sets of leg lifts. Standing up every hour.What’s Next?
Researchers are close to a breakthrough. Dr. Marc Hochberg predicts we’ll have a blood test within five years that can detect OA five to ten years before symptoms appear. That’s huge. Imagine catching it before the cartilage cracks. Preventing damage instead of treating it. For now, the tools we have work-if you use them. You don’t need expensive gear. You don’t need to run marathons. You need consistency. Movement. Weight control. And patience. The message isn’t ‘live with it.’ It’s ‘take it back.’ One step. One day. One change at a time.Is osteoarthritis the same as rheumatoid arthritis?
No. Osteoarthritis is caused by mechanical wear and biological breakdown in the joint. Rheumatoid arthritis is an autoimmune disease where your immune system attacks the joint lining. OA pain gets worse with activity and improves with rest. RA pain is often worse in the morning and improves with movement. RA also affects organs beyond joints and usually shows up symmetrically-both hands, both knees. OA is more likely to affect one side.
Can you reverse osteoarthritis?
No, you can’t reverse the damage already done to cartilage. But you can stop it from getting worse-and even feel better. Losing weight, staying active, and doing physical therapy can reduce pain, improve function, and delay the need for surgery. The goal isn’t to fix the joint, but to manage your life around it.
What exercises are best for osteoarthritis?
Low-impact activities are key: walking, cycling, swimming, and water aerobics. Strength training for muscles around the joint-like quadriceps for knees-is even more important than cardio. Flexibility work like yoga or stretching helps with stiffness. Aim for 45 minutes, three times a week. Start slow. Consistency beats intensity. A physical therapist can design a plan that fits your body.
Do I need an X-ray to diagnose osteoarthritis?
Not always. Doctors often diagnose OA based on symptoms and physical exam-pain with movement, stiffness after rest, joint swelling. X-rays are used to confirm severity, especially if surgery is being considered. But by the time changes show up on an X-ray, damage is already advanced. New research is focused on blood or imaging biomarkers to catch OA earlier.
Can diet help with osteoarthritis pain?
Yes-not because of specific foods, but because of weight control and inflammation. Eating whole foods, cutting sugar and processed carbs, and getting enough omega-3s (from fish or flaxseed) can reduce inflammation. Avoiding excess alcohol and red meat helps too. But no single food cures OA. The biggest dietary impact? Losing weight. Even 10 pounds can cut knee pain in half.
When should I consider a joint replacement?
When pain stops you from doing basic things-walking, sleeping, dressing-and other treatments have failed. Joint replacement is highly effective: 90% of patients report major improvement. But it’s major surgery. Recovery takes months. Most doctors recommend trying weight loss, exercise, physical therapy, and injections first. Don’t rush it. Wait until your quality of life is truly suffering.
Why does my OA pain get worse in cold weather?
There’s no clear scientific proof, but many patients report it. One theory: cold weather causes joint fluid to thicken, making movement stiffer. Another: barometric pressure changes may affect pressure inside the joint, irritating nerves. It’s not the cold itself damaging tissue-it’s how your body reacts. Staying warm, using heat packs, and moving gently can help.
Can osteoarthritis affect my mental health?
Absolutely. Chronic pain leads to sleep loss, reduced activity, isolation, and frustration. Studies show people with OA are twice as likely to develop depression or anxiety. It’s not just physical-it’s emotional. Talking to a counselor, joining a support group, or even just connecting with others who have OA can make a big difference. Your mental health is part of your treatment plan.
