Anticoagulant Management Calculator
Manage Your Anticoagulants Before Surgery
This tool helps determine optimal timing for stopping and restarting anticoagulants based on the latest evidence and guidelines.
Recommended Timing
Anticoagulant Information
Stop anticoagulant:
Restart anticoagulant:
Bridging recommended:
Important: This tool uses evidence-based guidelines from CHEST, ASH, and ACC. Always follow institutional protocols and consider individual patient factors.
Stopping blood thinners before surgery sounds simple-until it isn’t. A patient on apixaban for atrial fibrillation needs a knee replacement. Do you stop the medication? When? Should you bridge with heparin? What if the surgery turns emergency? One wrong call can mean a stroke… or a spinal hematoma. There’s no one-size-fits-all answer, but there is a proven, evidence-based way to get it right.
Why This Matters More Than You Think
Every year, hundreds of thousands of people on blood thinners undergo surgery. For many, these are routine procedures-hip replacements, colonoscopies, even dental work. But managing anticoagulants during this time is anything but routine. The goal is simple: avoid bleeding during surgery and prevent clots after. But the balance is razor-thin.Studies show that 17-23% of patients on DOACs (direct oral anticoagulants) who have emergency surgery experience major bleeding. At the same time, 7-16% face a dangerous clot-like a stroke or pulmonary embolism-if anticoagulation is stopped too long. The old approach-stop everything, bridge with heparin, restart after-is outdated. And it’s dangerous.
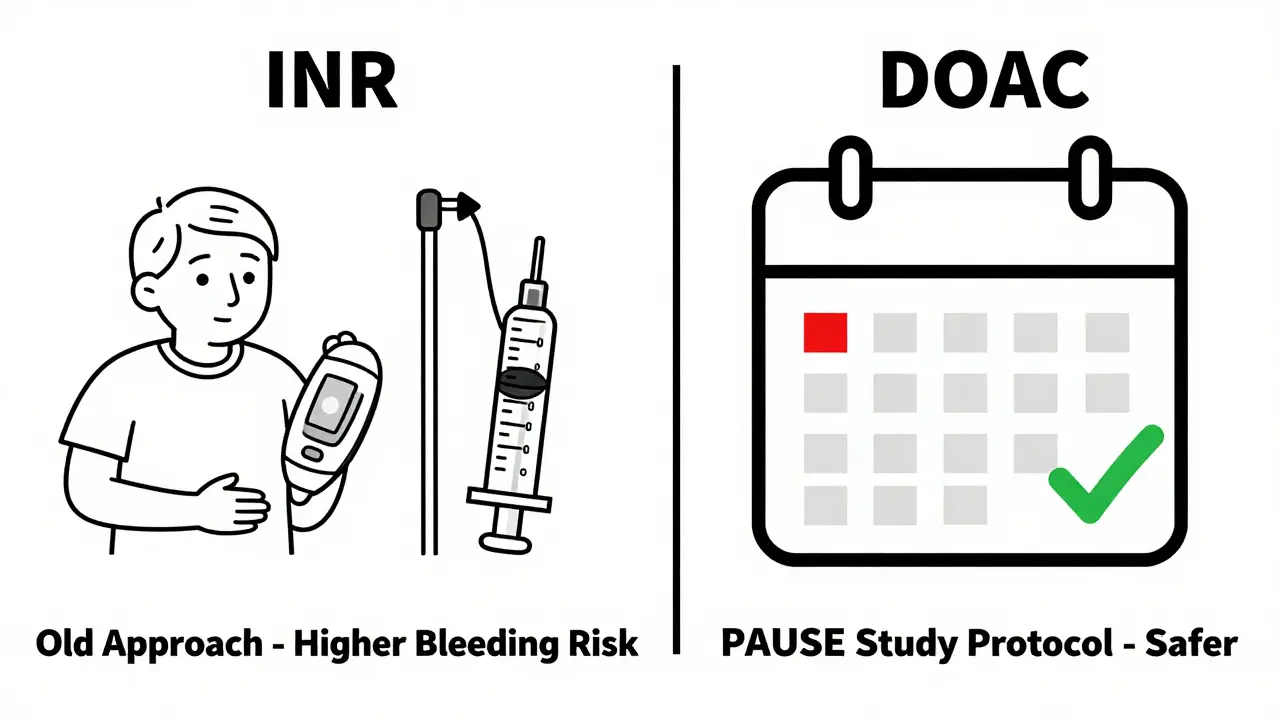
Since 2018, the PAUSE study changed everything. It proved that for most patients, bridging with heparin doesn’t prevent clots-it just causes more bleeding. That’s why major guidelines from the American College of Chest Physicians (CHEST), the American Society of Hematology (ASH), and the American College of Cardiology (ACC) now say: don’t bridge unless absolutely necessary.
DOACs vs. Warfarin: Two Different Worlds
Not all blood thinners are the same. The two main types today are DOACs and warfarin. They work differently, clear from the body differently, and need completely different handling.DOACs (like apixaban, rivaroxaban, dabigatran, edoxaban) are newer. They work fast, wear off fast. Most are gone from your system in 24-48 hours. That’s why you don’t need heparin bridges. You just stop them a few days before surgery, then restart after.
Warfarin is older. It takes days to build up and days to wash out. Your INR (a blood test) has to be checked. If you’re high risk for clots-like someone with a mechanical heart valve-you might still need bridging. But even here, the evidence is shifting. ASH 2022 guidelines say: for most patients, bridging does more harm than good.
Here’s what you need to know about timing:
- Apixaban, rivaroxaban, edoxaban: Stop 2-3 days before surgery
- Dabigatran: Stop 3-4 days before surgery (longer if kidney function is poor)
- Warfarin: Stop 5 days before surgery, check INR
And here’s the kicker: you don’t need to check DOAC levels before surgery. The ACC and CHEST both say routine blood tests for DOAC concentration aren’t useful. They don’t predict bleeding risk. Stop based on time, not numbers.
When to Restart After Surgery
Stopping is only half the battle. Restarting too soon? Bleeding risk. Too late? Clot risk.General rule: wait at least 24 hours after surgery before restarting. But the exact timing depends on how risky the surgery was.
- Low bleeding risk procedures (cataract surgery, dental extraction, skin biopsies): Restart anticoagulant the same day or next day
- High bleeding risk procedures (joint replacement, brain surgery, major abdominal surgery): Wait 48-72 hours
Some hospitals start with a lower dose first-like a prophylactic dose of apixaban (2.5 mg twice daily)-then move back to full therapeutic dose after 24-48 hours if there’s no bleeding. This is especially common in patients with high clot risk, like those with recent deep vein thrombosis.
For warfarin, restart 12-24 hours after surgery if bleeding is controlled. Then monitor INR every 2-3 days until it’s stable.
Special Cases: Neuraxial Anesthesia and Emergencies
If you’re having an epidural or spinal block, timing becomes critical. A single drop of blood in the spinal canal can cause permanent paralysis.ASRA guidelines are strict:
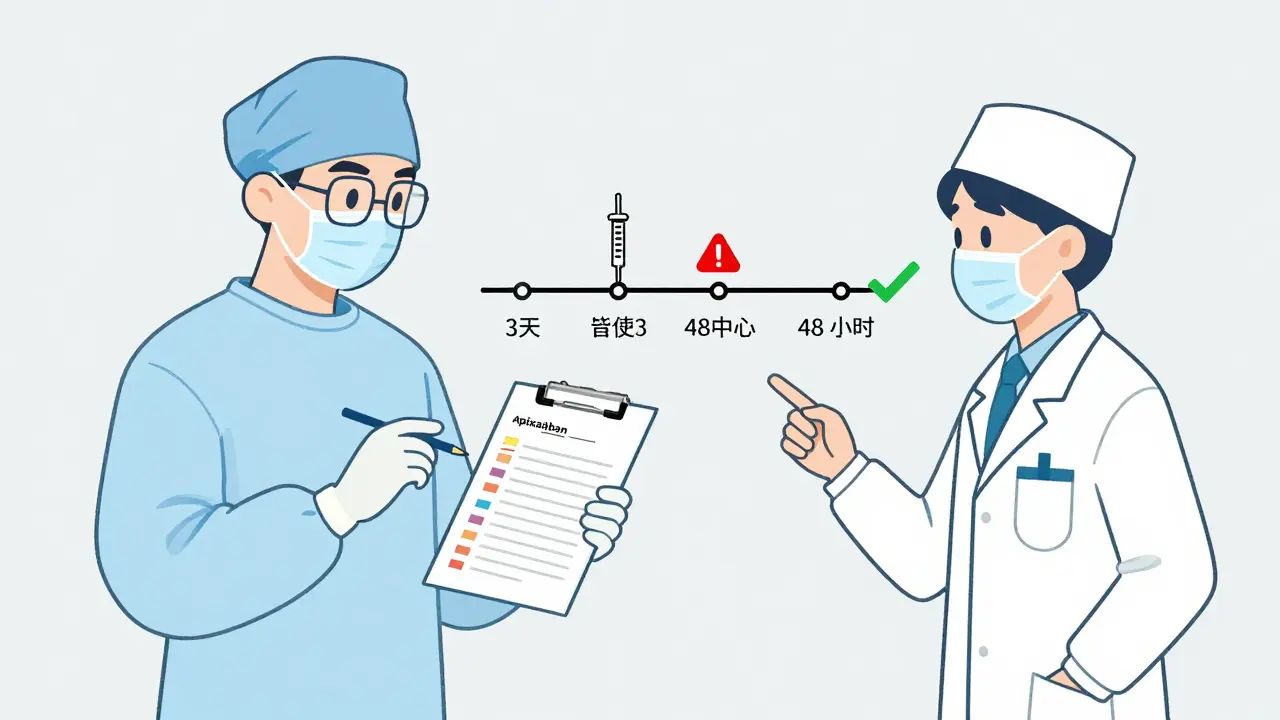
- Stop factor Xa inhibitors (apixaban, rivaroxaban, edoxaban) at least 3 days before neuraxial anesthesia
- Stop dabigatran at least 4 days before
- Wait at least 24 hours after the last dose of LMWH before placing the needle
And never restart anticoagulants until the catheter is removed and hemostasis is confirmed. Most hospitals wait 24-48 hours after catheter removal before giving the first post-op dose.
Now, what if someone shows up in the ER with a ruptured appendix and they’re on apixaban? You can’t wait. You need reversal.
Here’s what’s available:
- Dabigatran: Idarucizumab (Praxbind) - works in minutes. Cost: ~$3,700 per vial
- Factor Xa inhibitors (apixaban, rivaroxaban, etc.): Andexanet alfa (Andexxa) - works in minutes. Cost: ~$19,000 per dose
But here’s the catch: andexanet alfa carries its own risk. In the ANNEXA-4 trial, 13% of patients who got it had a stroke or heart attack within 30 days. That’s why it’s reserved for life-threatening bleeding, not routine cases.
Who’s at Highest Risk?
Not everyone needs the same plan. Risk stratification is everything.Use two simple scores:
- CHA₂DS₂-VASc: Measures stroke risk in atrial fibrillation. Score ≥2 means higher clot risk.
- HAS-BLED: Measures bleeding risk. Score ≥3 means high bleeding risk.
Here’s how they guide decisions:
- A 70-year-old with atrial fibrillation (CHA₂DS₂-VASc = 4) needs a colonoscopy. Low bleeding risk procedure. Don’t stop the DOAC. Keep going.
- A 65-year-old with mechanical mitral valve (high clot risk) needs hip surgery. Still, guidelines now say: no bridging. Stop DOAC 3 days out, restart 48 hours post-op.
- A 75-year-old with kidney disease and HAS-BLED = 4. Even a dental extraction may need extra caution. Consider delaying if possible.
Yet a 2021 survey found that 32% of management errors come from misapplying these scores. Don’t guess. Calculate.

Real-World Problems You Won’t Find in Guidelines
Guidelines look clean on paper. Real life? Messy.One patient on rivaroxaban needs urgent surgery for a bowel obstruction. No time to wait 3 days. The ER team gives andexanet alfa. Bleeding stops. But 10 days later, they have a pulmonary embolism. Why? The anticoagulant wasn’t restarted soon enough because the team was scared of re-bleeding.
Another case: a patient on warfarin with an INR of 5.5. The surgeon says, “We can’t operate.” But the INR is high because they missed doses. They didn’t need reversal-they needed vitamin K and a plan.
And cost? Andexanet alfa isn’t covered by all insurers. Some hospitals won’t stock it. Patients in rural areas may have to be transferred 100 miles away for reversal.
These aren’t edge cases. They’re daily challenges. That’s why training matters. A 2021 study of 127 hospitals found it takes 3-5 complex cases before clinicians feel confident managing anticoagulants perioperatively.
What’s Next? The Future of Blood Thinner Management
The next big thing? Ciraparantag. It’s a universal reversal agent-works on all anticoagulants, including DOACs and heparin. Phase 3 trials are ongoing. Early data shows it reverses clotting within 10 minutes. If approved, it could make emergency management much simpler.Also, registries like GARFIELD-AF are tracking over 75,000 patients across 35 countries. Real-world data will keep refining guidelines. We’re moving away from rigid timelines and toward personalized, dynamic decision-making.
But the core principle won’t change: stop anticoagulants only when the bleeding risk outweighs the clot risk. And even then, keep the interruption as short as possible.
Bottom Line: What You Need to Do
If you’re a patient on blood thinners and you’re scheduled for surgery:- Don’t stop your medication on your own.
- Ask your doctor: “Is this a high or low bleeding risk procedure?”
- Ask: “Do I need to stop my blood thinner? If so, when do I stop and when do I restart?”
- Ask: “Will I need bridging?” (Answer: Probably not.)
- Ask: “What’s my CHA₂DS₂-VASc and HAS-BLED score?”
If you’re a clinician:
- Stop using heparin bridging unless you have a mechanical mitral valve or recent VTE within 3 months.
- Use the PAUSE study protocol for elective cases.
- Never check DOAC levels.
- Know your reversal agents-and when to use them.
- Train your team. Mismanagement is still one of the top 10 preventable surgical complications.
Perioperative anticoagulation isn’t about following a checklist. It’s about understanding risk, timing, and the patient’s story. Do it right, and you prevent strokes and bleeds. Do it wrong, and the consequences can be permanent.
Should I stop my blood thinner before a minor dental procedure?
No, not usually. For low-bleeding-risk procedures like fillings, extractions, or root canals, guidelines from the American Heart Association and ACC say you can continue DOACs and warfarin without interruption. The risk of a clot from stopping is far greater than the risk of minor bleeding, which can be controlled with pressure and local measures.
Can I take aspirin instead of my blood thinner before surgery?
No. Aspirin is not a substitute for anticoagulants like apixaban or warfarin. It only affects platelets, not the clotting cascade. Stopping your prescribed anticoagulant and replacing it with aspirin leaves you unprotected against strokes and clots. Always follow your doctor’s specific instructions-never self-switch medications.
What if I forget to stop my DOAC before surgery?
If you’re on a DOAC and didn’t stop it on time, the surgical team may delay the procedure if possible. If it’s urgent, they’ll use reversal agents like idarucizumab (for dabigatran) or andexanet alfa (for factor Xa inhibitors). These aren’t perfect-they carry risks-but they’re the best tools available. Always inform your surgeon and anesthesiologist about your medication history.
Do I need to get my blood tested before surgery if I’m on a DOAC?
No. Major guidelines from CHEST and ACC explicitly say routine lab testing for DOAC levels is not recommended. These drugs have predictable half-lives, so stopping them 2-4 days before surgery based on the drug type is sufficient. Testing adds cost and delay without improving safety.
Why do some hospitals still use heparin bridging for DOACs?
Because old habits die hard. Some institutions haven’t updated their protocols since before the PAUSE study (2018). Others do it out of fear-even though evidence shows bridging increases major bleeding by 2-3 times without reducing clots. The 2023 CHEST guidelines clearly state: ‘We suggest against bridging for DOACs.’ If your hospital still uses it routinely, ask for the evidence behind their protocol.
Is it safe to restart my anticoagulant after major surgery?
Yes-but timing matters. For high-bleeding-risk surgeries like brain or abdominal operations, wait 48-72 hours. For lower-risk surgeries like hip replacements, 24-48 hours is usually safe. Always restart with your doctor’s guidance. Some patients get a lower dose first (e.g., apixaban 2.5 mg twice daily) before returning to full dose. Never restart without medical approval.
All Comments
Kegan Powell January 27, 2026
this is the kind of post that makes me feel like a better doctor just by reading it 🙌 no fluff, just facts. i've seen so many patients get hurt because someone was too scared to stop bridging. time to update our protocols.
Paul Taylor January 29, 2026
i remember when we used to bridge everyone like it was gospel and now we know that the real danger isn't the clot it's the bleeding from the heparin and nobody talks about how much this saves money too like imagine not paying 20k for andexanet every time someone needs a colonoscopy
John O'Brien January 29, 2026
stop being so soft on this stuff. if you're on apixaban and you show up for surgery late you dont get a free pass. you get delayed or you get reversal and if you're dumb enough to forget you deserve the consequences
Patrick Merrell January 30, 2026
they say dont bridge but what about the patients who get clots anyway? someone's gotta be the sacrifice for the guidelines to look good. i've seen it happen and the hospital never takes responsibility
Marian Gilan January 30, 2026
andexanet costs 19k but the pharma companies are hiding the real data. they know it causes strokes but they dont want you to know. ask yourself why they dont test it on people over 75. theyre lying to us
Desaundrea Morton-Pusey February 1, 2026
why do americans even need blood thinners anyway? we're all just sitting on couches eating chips and then we get surgery and act like it's a crisis. just move more and stop being weak
Kathy McDaniel February 2, 2026
this was so helpful!! i had a knee replacement last year and they stopped my rivaroxaban 3 days out and restarted it day 2 post-op and i was fine no issues at all 🙏
Conor Flannelly February 3, 2026
i've worked in rural ireland for 15 years and let me tell you the biggest problem isnt the guidelines its the lack of access. if you need andexanet and you're 80 miles from the nearest hospital? you're out of luck. we need better infrastructure not just better science
Conor Murphy February 4, 2026
this is why i love medicine. we're learning. we're changing. we're not clinging to old ways because they feel safe. thank you for writing this. it's a gift to the field
Kirstin Santiago February 5, 2026
i read this and thought about my mom who's on warfarin and had a tooth extraction last month. they told her to keep taking it. she was terrified but it worked. no bleeding. no clot. just quiet, smart care
Murphy Game February 6, 2026
they say dont check doac levels but what if your lab is wrong? what if the patient lied? what if the drug was counterfeit? we're trusting algorithms now not doctors. this is how people die
April Williams February 7, 2026
you think this is bad? wait until the insurance companies start dictating how long you wait to restart. they're already pushing for 72 hours on everything to save a buck. this isn't medicine anymore its accounting
Harry Henderson February 7, 2026
if you're not using the pause protocol by now you're not just behind you're dangerous. stop being lazy. learn it. teach it. implement it. your patients deserve better
suhail ahmed February 8, 2026
in india we dont even have access to half these drugs. we use aspirin and pray. i wish someone would send us a shipment of andexanet or even a simple reversal guide in hindi. we're not asking for fancy tech just basic survival tools
Candice Hartley February 9, 2026
just had my dad on apixaban for afib. doc said stop 2 days before his cataract surgery. restart next day. zero bleeding. zero stress. this is how it should be.