When you’re planning a pregnancy and managing an autoimmune disease, the question isn’t just can I get pregnant? It’s can I stay healthy while protecting my baby? For women with conditions like lupus, rheumatoid arthritis, or psoriatic arthritis, the answer used to be a cautious "maybe." But new evidence from 2024 and 2025 is changing everything. You don’t have to choose between your health and your baby’s safety - if you plan ahead and use the right data.
Most Medications Are Safe - If You Plan Ahead
The biggest myth? That you need to stop all your meds before getting pregnant. That’s not true. According to updated guidelines from the European Alliance of Associations for Rheumatology (EULAR) in February 2025, 87% of standard autoimmune treatments can be safely continued through conception, pregnancy, and breastfeeding. That’s a huge shift from just five years ago. The real danger isn’t the medication - it’s uncontrolled disease. Take rheumatoid arthritis. If your disease is active, your risk of preterm birth, preeclampsia, and low birth weight goes up. But if you keep taking hydroxychloroquine, your risk of flare drops by 66%. Hydroxychloroquine has been studied in over 12,450 pregnancies. Not one study found a higher rate of birth defects. It’s not just safe - it’s protective. Same goes for azathioprine. Used in lupus and other conditions, it’s been tracked in more than 5,800 pregnancies. Only 2.1% of babies born to moms on azathioprine were preterm - compared to 8.7% when the disease itself is active. That’s a clear signal: keeping your condition stable matters more than stopping the drug.Which Medications Are Safe? The Clear List
Not all drugs are created equal. Some are safe. Some are not. Here’s what the data says as of 2025:- Hydroxychloroquine - 98.7% safe. Recommended for all pregnant women with lupus or RA. Reduces flares by 66%.
- Azathioprine - 95.3% safe. Used for lupus, vasculitis, and more. Minimal risk to baby.
- Sulfasalazine - 97.1% safe. No birth defects linked. Safe for men too - no effect on sperm.
- Corticosteroids - Low-dose prednisone (≤10mg/day) is safe. Higher doses may raise risk of gestational diabetes or high blood pressure, but still better than uncontrolled inflammation.
- TNF inhibitors - 94.8% safe overall. Certolizumab pegol is the top choice because it barely crosses the placenta (just 0.2% of maternal levels). Adalimumab and infliximab cross more - but still safe. Many doctors now recommend continuing them through delivery.
- Antimalarials - Hydroxychloroquine is the star. Chloroquine is also safe.
The Medications You Must Stop - And When
Some drugs are absolutely unsafe during pregnancy. No exceptions.- Methotrexate - Absolute contraindication. Even small doses can cause severe birth defects like missing limbs, cleft palate, and skull abnormalities. Must be stopped at least 3 months before trying to conceive.
- Mycophenolate mofetil - High risk. Linked to 24.4% rate of major birth defects - including ear, eye, and heart problems. FDA has a black box warning. Must be stopped at least 6 weeks before conception - but 3 months is safer.
- JAK inhibitors (like tofacitinib, upadacitinib) - EULAR says avoid. Japan’s guidelines allow them in the first trimester based on 47 pregnancies with only 1.8% defect rate. But outside Japan? Play it safe. Stop before conception.
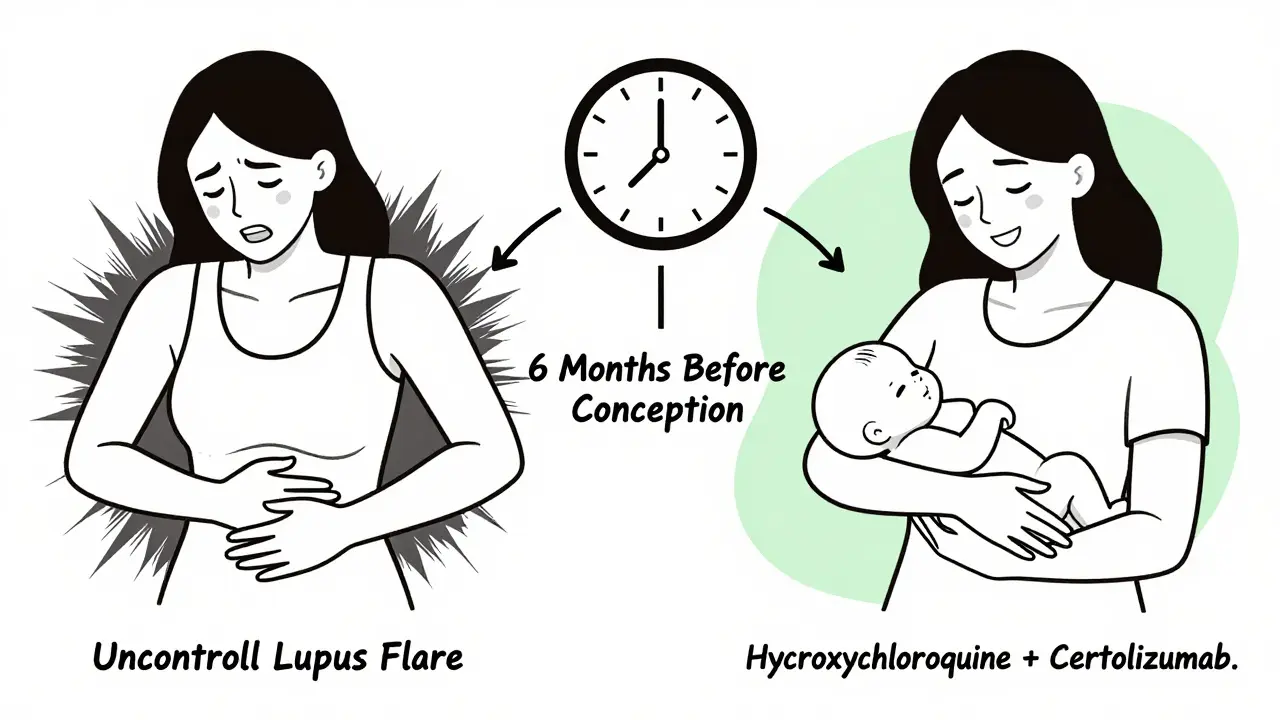
Timing Matters: Start Planning 6 Months Before
You wouldn’t start a new job without training. Why start a pregnancy without a medication plan? The best outcomes happen when you work with your rheumatologist at least six months before trying to conceive. That’s when you switch from risky drugs to safe ones. For example:- If you’re on methotrexate, switch to hydroxychloroquine or azathioprine 3 months out.
- If you’re on mycophenolate, switch 6 weeks out - but 3 months is better.
- If you’re on adalimumab and want to minimize placental transfer, switch to certolizumab pegol.
What About Breastfeeding?
Yes, you can breastfeed. Almost all biologics are safe. Adalimumab, infliximab, certolizumab - they barely pass into breastmilk. Studies show levels are 0.005% to 0.13% of the mother’s blood concentration. That’s less than what your baby would get from a single drop of medicine. The American Academy of Pediatrics says biologics are compatible with breastfeeding. You don’t need to pump and dump. You don’t need to wait hours after a shot. Just keep taking your meds. Your baby will be fine.Real Stories: What Happens When You Don’t Plan
One woman on Reddit shared: "I stopped adalimumab at 8 weeks because my OB said it was "too risky." I had a massive RA flare at 20 weeks. I needed 20mg of prednisone daily. I got gestational diabetes. My son was born at 34 weeks." Another wrote: "I stayed on hydroxychloroquine and certolizumab. My baby was born at 39 weeks, 7 lbs 10 oz. Zero complications." The difference? Planning. The first woman followed outdated advice. The second followed evidence.What About Biosimilars? Are They Safe Too?
Yes. Since Humira’s patent expired in January 2023, eight biosimilars entered the market - Amjevita, Hyrimoz, Hadlima, and others. The FDA says they’re identical in structure and function to the original. That means they’re just as safe in pregnancy. No need to switch back to the brand name unless your insurance forces you to.
Why You Need a Team - Not Just an OB
Your OB-GYN is amazing. But they’re not trained in autoimmune disease. A 2022 survey found that 41.7% of women stopped their meds without talking to their rheumatologist - because their OB didn’t know what to say. The gold standard? A team. A rheumatologist who knows the drugs. A maternal-fetal medicine specialist who knows pregnancy risks. And a pharmacist who can check interactions. Women who saw all three had 53% fewer unplanned medication stops and 37% more full-term births. That’s not a coincidence. That’s coordinated care.What’s Coming Next?
In January 2024, the NIH launched a $12.7 million research network to study JAK inhibitors and newer biologics in pregnancy. They’ll track 5,000 women over five years. That’s huge. EULAR is releasing a patient decision tool in November 2024 - a simple app to help you see your personal risk and options. And by 2026, we’ll likely have better data on drugs like belimumab and rituximab - which are already being used safely in thousands of pregnancies, but still lack large-scale studies.Key Takeaways
- Don’t stop your meds without talking to your rheumatologist.
- Hydroxychloroquine, azathioprine, and certolizumab pegol are safe - and often protective.
- Methotrexate and mycophenolate are dangerous - stop them months before trying to conceive.
- Plan ahead. Six months is the sweet spot.
- Continue TNF inhibitors through delivery and breastfeeding. No need to pause.
- Get care from a rheumatologist + maternal-fetal specialist. It changes outcomes.
Can I get pregnant if I have lupus or rheumatoid arthritis?
Yes. Most women with autoimmune diseases can have healthy pregnancies. The key is disease control. If your condition is stable for at least 3-6 months before conception, your chances of a full-term, healthy baby are very high. Active disease - not medication - is the biggest threat.
Is hydroxychloroquine safe during pregnancy?
Yes. Hydroxychloroquine is one of the safest drugs for pregnancy in autoimmune disease. It’s been studied in over 12,450 pregnancies with no increase in birth defects. It actually reduces lupus flares by 66% and lowers the risk of preterm birth and preeclampsia by half. It’s recommended for all pregnant women with lupus or RA.
What happens if I get pregnant while still on methotrexate?
Stop it immediately and contact your rheumatologist. Methotrexate can cause severe birth defects - including missing limbs, cleft palate, and skull abnormalities. The risk is 17.8% based on registry data. But if you stop early, many pregnancies proceed normally. Early detection and switching to a safer drug like hydroxychloroquine can make a big difference.
Should I stop my TNF inhibitor at 32 weeks?
No. There’s no evidence that continuing TNF inhibitors past 32 weeks increases infection risk in newborns. A 2021 study of 14,320 infants found identical infection rates (7.3% exposed vs. 7.1% unexposed). Certolizumab pegol is especially safe to continue through delivery. For adalimumab or infliximab, some doctors may pause after 30 weeks - but it’s not required. Always discuss this with your team.
Can I breastfeed while on biologics?
Yes. Biologics like adalimumab, infliximab, and certolizumab pegol transfer in tiny amounts to breastmilk - often less than 0.1% of the mother’s blood level. The American Academy of Pediatrics considers them compatible with breastfeeding. You do not need to pump and dump. You can continue your medication as usual.
Are biosimilars safe during pregnancy?
Yes. Biosimilars like Amjevita and Hyrimoz are exact copies of the original biologic (e.g., Humira) in structure and function. The FDA confirms they have the same safety profile. If you’re on a biosimilar, you don’t need to switch back to the brand name. They’re equally safe for pregnancy and breastfeeding.
Next Steps
- If you’re thinking about pregnancy: Schedule a visit with your rheumatologist now - even if you’re not trying yet.
- Bring a list of all your medications, including supplements.
- Ask: "Which of my drugs need to be switched? When? What’s the safest alternative?"
- Ask if your clinic offers preconception counseling with a maternal-fetal medicine specialist.
- Don’t rely on online forums or outdated OB advice. Use EULAR 2025 and BSR 2021 guidelines as your reference.
You don’t have to sacrifice your health to have a baby. You just need to plan. And you’re not alone - thousands of women have done this successfully. With the right team and the right data, you can too.
