Rifampin Interaction Calculator
When you’re on rifampin for tuberculosis or to prevent meningitis, you might not think about how it affects your other meds. But if you’re taking blood thinners like warfarin, rivaroxaban, or apixaban-or antivirals like HIV meds or hepatitis C treatments-rifampin can seriously lower their levels in your body. This isn’t a minor issue. It can lead to blood clots, strokes, or even treatment failure. And it happens fast: within days of starting rifampin, your anticoagulant or antiviral might stop working the way it should.
Why Rifampin Changes How Other Drugs Work
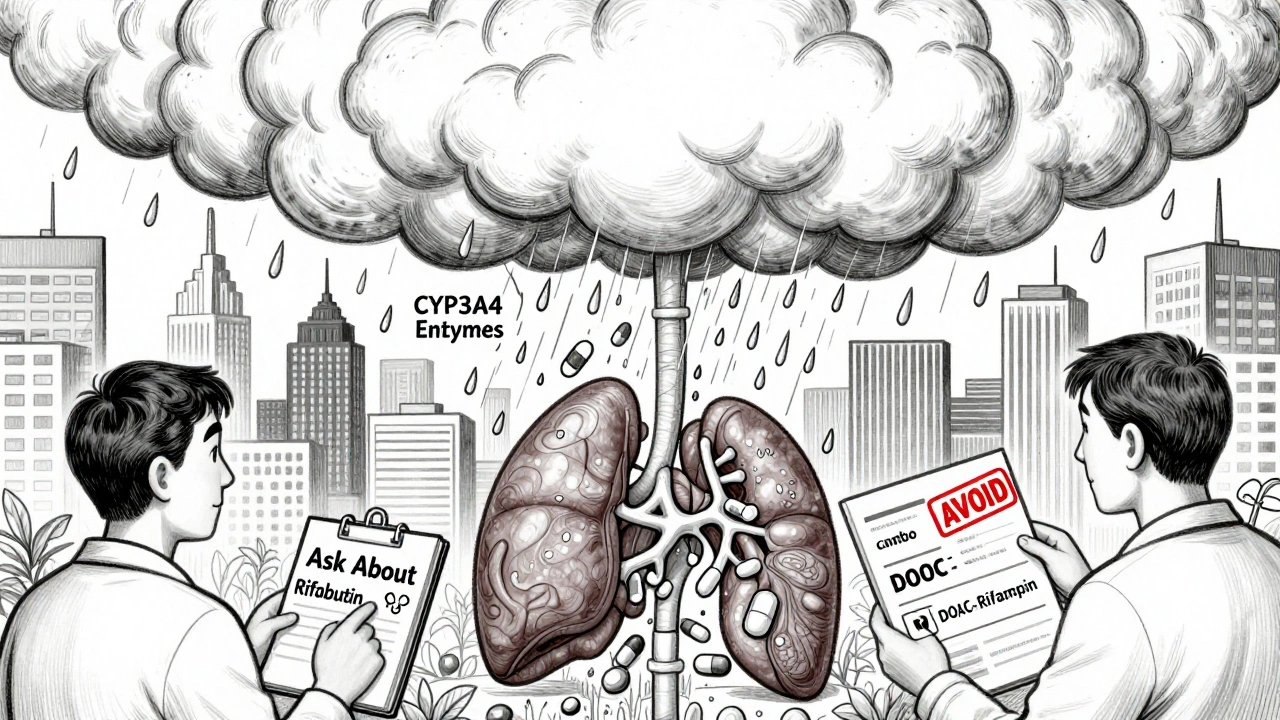
Rifampin doesn’t just kill bacteria. It flips a switch in your liver that tells your body to make more of certain enzymes-mainly CYP3A4 and CYP2C9. These enzymes break down drugs. When there’s too much of them, your blood thinners and antivirals get cleared out way too quickly. It’s like turning up the faucet on a drain: the water (your medicine) just flows out before it can do its job.
This isn’t guesswork. The U.S. FDA classifies rifampin as a strong inducer-meaning it can drop the concentration of some drugs by 80% or more. Studies show that after just 24 to 48 hours of rifampin, enzyme levels start rising. By day five to seven, they peak. And even after you stop rifampin, it can take two to three weeks for your body to calm down and return to normal. That’s a long time to be at risk.
How Rifampin Hits Anticoagulants
If you’re on warfarin, rifampin can slash your INR levels-the measure of how long your blood takes to clot. A 2020 review in Pharmacotherapy found that warfarin’s effectiveness dropped by 15% to 74% when taken with rifampin. That’s not a small dip. It’s enough to make someone with a mechanical heart valve suddenly vulnerable to a clot. One case report described a 57-year-old woman whose INR dropped from 2.8 to 1.2 after starting rifampin for suspected endocarditis. She had no bleeding, but she was at high risk of a stroke. Her doctors had to switch her to heparin injections until rifampin cleared from her system.
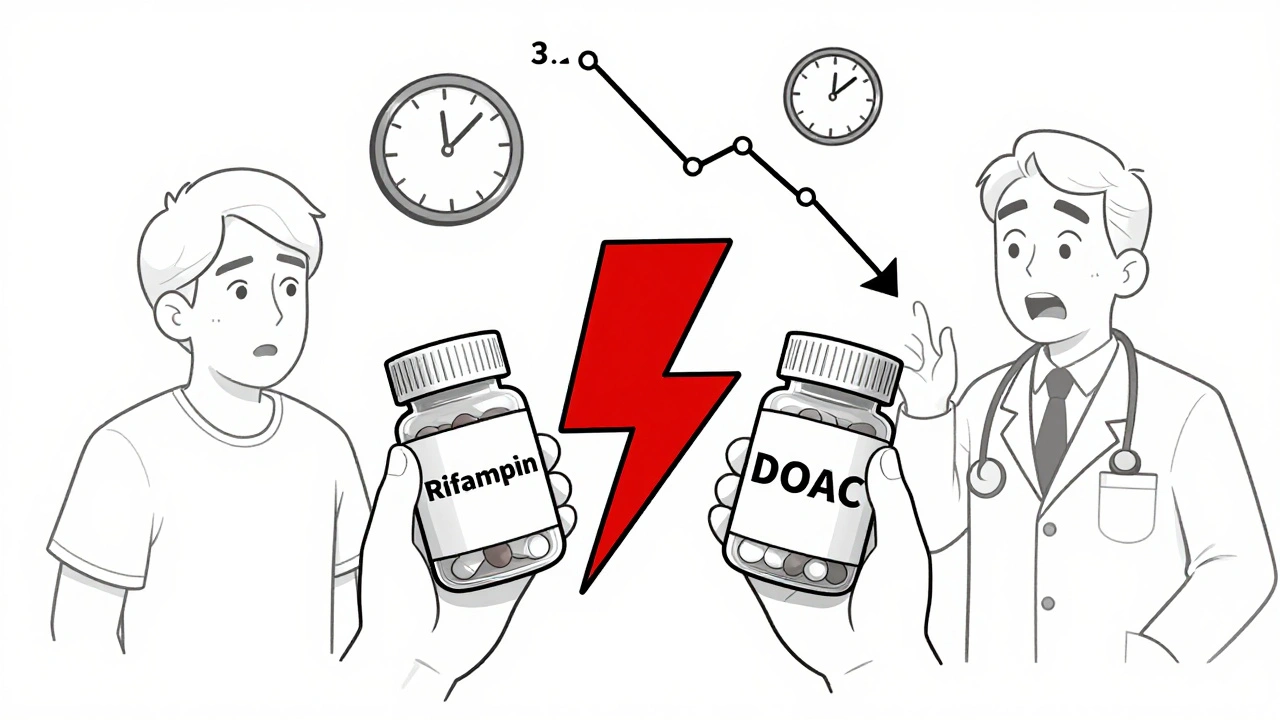
It’s not just warfarin. Direct oral anticoagulants (DOACs) like rivaroxaban, apixaban, and dabigatran are also hit hard. Studies show:
- Rivaroxaban: AUC dropped by 50-67%
- Apixaban: AUC dropped by 50-60%
- Dabigatran: AUC dropped by 60-67%
- Edoxaban: AUC dropped by 35%, but its active metabolites rose, making the outcome unpredictable
The European Heart Rhythm Association says combining DOACs with rifampin is generally not recommended. Why? Because unlike warfarin, you can’t easily check DOAC levels with a blood test. There’s no INR to monitor. So you’re flying blind.
Rifampin and Antivirals: A Dangerous Mix
The same enzyme surge that messes with blood thinners also wrecks antivirals. HIV medications like darunavir, atazanavir, and raltegravir are metabolized by CYP3A4. When rifampin is added, their levels can crash by up to 80%. That’s not just inconvenient-it’s dangerous. Subtherapeutic levels mean the virus can bounce back, develop resistance, and become harder to treat.
For hepatitis C, drugs like grazoprevir and elbasvir are also affected. A 2021 study in Frontiers in Pharmacology showed that patients on rifampin for TB and antivirals for hepatitis C had viral loads that didn’t drop as expected. Some even had treatment failure.
There’s one exception: some newer antivirals like sofosbuvir are less affected because they’re not primarily broken down by CYP3A4. But even then, experts still recommend caution and close monitoring.
What Clinicians Do When Rifampin Is Needed
When someone needs rifampin-say, for TB-and they’re on a blood thinner, guidelines are clear: avoid the combo if possible. The American College of Chest Physicians recommends switching from warfarin to low molecular weight heparin (like enoxaparin) during rifampin treatment. Heparin doesn’t rely on liver enzymes the same way, so it’s safer.
But what if you can’t switch? For warfarin, you might need to triple or even quadruple the dose. One study found patients needed 3 to 5 times more warfarin to keep INR in range. That’s risky. Too much can lead to bleeding. Too little, and you get clots. Frequent INR checks-sometimes daily-are required. Point-of-care devices help, with accuracy within ±0.5 INR units, but they’re not a fix. Just a tool.
For DOACs, the answer is usually: don’t use them together. But there’s a gray area. A 2021 study in Frontiers in Pharmacology looked at six patients with prosthetic joint infections who needed both rifampin and rivaroxaban. With careful, gradual dose adjustments and close follow-up, some managed to stay on both. But this wasn’t standard care. It was tailored, high-risk management. Only a handful of hospitals in the U.S. have protocols for this. As of 2022, just 12% did.
The Bigger Picture: New Drugs and Better Safety
Drugmakers are learning from these interactions. The FDA now requires new anticoagulants to be tested against strong inducers like rifampin before approval. That’s why newer drugs like milvexian (a factor XIa inhibitor) are being studied specifically for their resistance to CYP3A4 induction. Early data suggests they might be safer.
Meanwhile, the way we treat patients is changing. Between 2010 and 2020, the percentage of people on DOACs instead of warfarin jumped from 15% to 85%. That’s progress. But many of these patients still get rifampin for infections. The mismatch is dangerous. Older adults, especially those with cancer or heart issues, are at highest risk. And we’re still not great at catching these interactions in time.
What You Should Do
If you’re on any anticoagulant or antiviral and your doctor adds rifampin, ask these questions:
- Is there an alternative to rifampin? (Like rifabutin, which is a weaker inducer)
- Can I switch to heparin during rifampin treatment?
- How often will my levels be checked?
- What signs of clotting or bleeding should I watch for?
Don’t assume your pharmacist or doctor already knows. Many don’t. A 2022 survey found that nearly half of primary care providers didn’t know rifampin could wipe out DOAC effectiveness. That’s a gap. You have to be your own advocate.
What’s Next?
Research is moving toward drugs that don’t rely on CYP enzymes. Until then, the best defense is awareness. Rifampin isn’t just an antibiotic. It’s a metabolic storm. It doesn’t just interact-it overrides. And if you’re on a blood thinner or antiviral, that storm can be life-threatening.
The good news? With careful planning, monitoring, and communication, you can manage it. But you need to act before it’s too late. Don’t wait for symptoms. Don’t assume it’s fine. Talk to your care team. Document everything. And never start or stop rifampin without reviewing every other drug you’re taking.
Can I take warfarin with rifampin?
Yes, but it’s risky and requires major adjustments. Rifampin can reduce warfarin levels by up to 74%, causing your INR to drop dangerously low. You’ll likely need to triple or quadruple your warfarin dose and check your INR daily. Most experts recommend switching to heparin injections instead, which aren’t affected by rifampin. Only use warfarin with rifampin if no other option exists-and only under close supervision.
Are DOACs safer than warfarin when taking rifampin?
No. DOACs like rivaroxaban, apixaban, and dabigatran are just as vulnerable to rifampin’s enzyme-inducing effects. Studies show their levels drop by 50-67%. Unlike warfarin, there’s no routine blood test to monitor DOAC levels, making it harder to detect when they’re too low. The European Heart Rhythm Association advises avoiding DOACs with rifampin altogether. If absolutely necessary, it requires expert management and frequent clinical review.
Does rifampin affect HIV medications?
Yes, severely. Rifampin cuts levels of key HIV drugs like darunavir, atazanavir, and raltegravir by up to 80%. This can lead to treatment failure and drug resistance. Guidelines recommend switching to rifabutin, a weaker inducer, when possible. If rifampin is unavoidable, HIV meds may need higher doses-but only under expert supervision. Never combine them without a specialist’s input.
How long does rifampin’s effect last after stopping it?
Rifampin’s enzyme-inducing effects can last 2 to 3 weeks after you stop taking it. That’s because your liver needs time to break down the extra enzymes it made. If you’re on an anticoagulant or antiviral, you can’t just stop rifampin and return to your old dose. Levels may remain low for weeks, and you’ll need to adjust your meds slowly under medical supervision.
Is there a safer antibiotic than rifampin for people on blood thinners?
Yes-rifabutin. It’s a close relative of rifampin but a much weaker enzyme inducer. For patients on HIV meds or anticoagulants, rifabutin is often preferred when treating TB. It still has interactions, but they’re less severe. Always ask your doctor if rifabutin is an option. It’s not always available or approved for every use, but it’s a safer alternative when possible.
Why don’t all doctors know about this interaction?
Because it’s complex and not always taught in medical training. Many providers focus on the infection being treated, not the hidden drug interactions. A 2022 survey found nearly half of primary care doctors didn’t realize rifampin could wipe out DOAC effectiveness. Also, with DOACs being newer, guidelines are still catching up. Always bring your full med list to every appointment-don’t assume your doctor knows what you’re on.

All Comments
Himmat Singh December 13, 2025
While the post presents a clinically accurate overview, it fails to address the broader pharmacoeconomic implications of rifampin-inducer interactions in low-resource settings. In India, where tuberculosis is endemic and DOACs remain prohibitively expensive, warfarin remains the de facto anticoagulant. The suggestion to switch to LMWH is not merely impractical-it is ethically untenable for the majority of patients who cannot afford daily subcutaneous injections or frequent INR monitoring. The real issue is not the pharmacokinetics, but the systemic neglect of patient-centered alternatives. Rifampin’s induction is a known entity since the 1970s; why are we still treating this as a novel clinical dilemma?
Jamie Clark December 14, 2025
Let’s be brutally honest-this isn’t about drug interactions. It’s about pharmaceutical capitalism. Drugmakers don’t want you to know that rifampin is 100x cheaper than DOACs and just as effective for TB. They push expensive anticoagulants, then act shocked when a $5 antibiotic ruins their $1,000/month drug’s efficacy. The FDA’s ‘strong inducer’ classification? A legal shield. The real danger isn’t rifampin-it’s the medical-industrial complex that profits from complexity. If they wanted safety, they’d ban the combo outright. They don’t. They just make you jump through hoops. Wake up.
Webster Bull December 15, 2025
Y’all need to chill. Rifampin’s a beast, yeah-but it’s not magic. If you’re on blood thinners and get TB, your doc’s gonna fix this. Heparin for a few weeks? Totally fine. Switch back? Easy. Don’t panic. Just tell your pharmacist EVERYTHING you’re on. Seriously. I had a cousin on apixaban, got rifampin for TB-doc swapped her to Lovenox for 6 weeks. She’s fine now. No drama. Just communication. 🙌
And yes, rifabutin’s a better option if you can get it. But if you’re in a rural clinic with 1 pill left? Rifampin’s your only shot. Don’t let fear stop treatment.
Michael Gardner December 15, 2025
Interesting how the post frames this as a clinical problem when it’s fundamentally a regulatory failure. If rifampin’s been known to induce CYP3A4 since the 80s, why are we still approving new anticoagulants without mandatory induction testing? Why is there no black box warning on DOAC packaging? The system isn’t broken-it’s designed this way. Patient safety is secondary to speed-to-market and patent extensions. The fact that only 12% of U.S. hospitals have protocols for this? That’s not negligence. That’s policy.
Willie Onst December 15, 2025
Hey everyone-just wanted to say this is such a critical topic, especially for older folks juggling meds. I’ve seen my grandma’s INR crash after starting rifampin, and it was terrifying. But here’s the thing: you’re not alone. Talk to your pharmacist, bring your pill bottles, ask for a med review. Seriously, they’re the unsung heroes. And if your doctor doesn’t know? That’s okay-just say, ‘I read this article, can we talk about alternatives?’
Also, rifabutin exists! It’s not magic, but it’s gentler. And hey, if you’re on HIV meds, please, please, please find an infectious disease specialist. They’re the real MVPs here. 💪❤️
Jennifer Taylor December 16, 2025
WAIT. So you’re telling me rifampin is being used by the government to LOWER antiviral levels on purpose?? Like… is this a hidden agenda? Think about it-HIV meds cost thousands. TB meds cost pennies. What if this isn’t an accident? What if they WANT people on antivirals to fail so they’ll buy newer, more expensive drugs? And DOACs? They’re designed to be unmonitored so you can’t track the drop-so you never know until you have a stroke! It’s all connected. The FDA, Big Pharma, the WHO-they all profit when you get sick again. I’ve seen the documents. They’re hiding this. I’m not crazy. I’m just the only one who’s reading.
Shelby Ume December 16, 2025
As a clinical pharmacist with over 18 years in anticoagulation management, I can confirm the data presented is accurate and well-sourced. However, the real challenge lies in implementation. In community settings, especially outside academic centers, providers rarely have access to pharmacokinetic modeling tools or real-time therapeutic drug monitoring. The recommendation to ‘switch to heparin’ assumes availability, training, and patient compliance-all of which are variable. We need standardized clinical decision support embedded in EHRs, not just guidelines in journals. Until then, we are asking clinicians to perform high-risk pharmacology without tools. This is not a patient issue. It is a systems issue.
Jade Hovet December 16, 2025
OMG I JUST SAW THIS AND HAD TO COMMENT!! 😱 My dad’s on rivaroxaban for AFib and got rifampin for TB last year-scared the crap outta us. But we called his pharmacy’s med line and they hooked us up with a clinical pharmacist who adjusted his dose and set up daily INR checks with a portable device. We did it! He’s fine now. 🙌
Just please, if you’re on meds, don’t Google and panic. CALL YOUR PHARMACIST. They’re like superhero doctors without capes. And yes, rifabutin exists-ask for it! Also, I spelled ‘rifampin’ wrong 3 times while typing this. 😅
nithin Kuntumadugu December 17, 2025
Typical western medicine nonsense. You think you’re smart because you know CYP3A4? Pathetic. Rifampin is a NATURAL remedy that cleanses the liver. The DOACs? Synthetic poison from corporate labs. They’re scared because rifampin costs $2 and works better than their $500 pills. And now they want to ban it? HA. They don’t want you healthy-they want you dependent. I’ve been on both since 2019. My INR? Stable. My liver? Cleaner than yours. You think science knows everything? You’re still using antibiotics like cavemen. #RifampinIsTheTruth