What Happens After a Stroke?
When a stroke hits, it doesn’t just end with the initial event. The real work begins in the hours and days that follow. The brain is damaged, but it’s not dead. Many people don’t realize that the brain can heal itself-stroke rehabilitation is what unlocks that ability. Without it, recovery is slower, less complete, and often leaves people struggling with everyday tasks they once took for granted.
Recovery isn’t a straight line. It’s messy, unpredictable, and deeply personal. Some people regain most of their movement within weeks. Others take years. The difference? Timing, intensity, and the right team. The science is clear: the sooner you start, the better the outcome. Studies show that starting therapy within 24 hours of a stroke can improve mobility outcomes by 35% compared to waiting. That’s not a small edge-it’s life-changing.
The Three Stages of Stroke Recovery
Recovery happens in phases, and each one needs a different focus. Ignoring the stage you’re in can slow progress or even cause harm.
Phase 1: Recovery and Natural Healing (Days to Weeks)
Right after a stroke, the brain is swollen and fragile. This isn’t the time for heavy exercise. The goal here is to prevent complications. That means turning you regularly in bed to avoid pressure sores, gently moving your limbs to keep joints flexible, and getting you sitting up as soon as doctors say it’s safe. About 65-78% of stroke survivors develop spasticity-muscles that tighten and refuse to relax. Passive range-of-motion exercises done 2-3 times a day can cut that risk in half.
Phase 2: Retraining (Weeks to Months)
This is where the real rebuilding happens. Your brain starts rewiring itself. This is neuroplasticity in action: healthy parts of the brain take over functions lost to the damaged areas. Therapists use repetition, cues, and task-specific training to force those new connections to form. Want to walk again? You’ll practice standing, shifting weight, stepping with a brace, then walking with support. Want to use your hand? You’ll pick up spoons, turn doorknobs, button shirts-repeatedly. Constraint-induced therapy, where the good arm is strapped down for 90% of the day, forces the weak one to work. Mayo Clinic studies show this leads to 30% better motor gains than standard therapy.
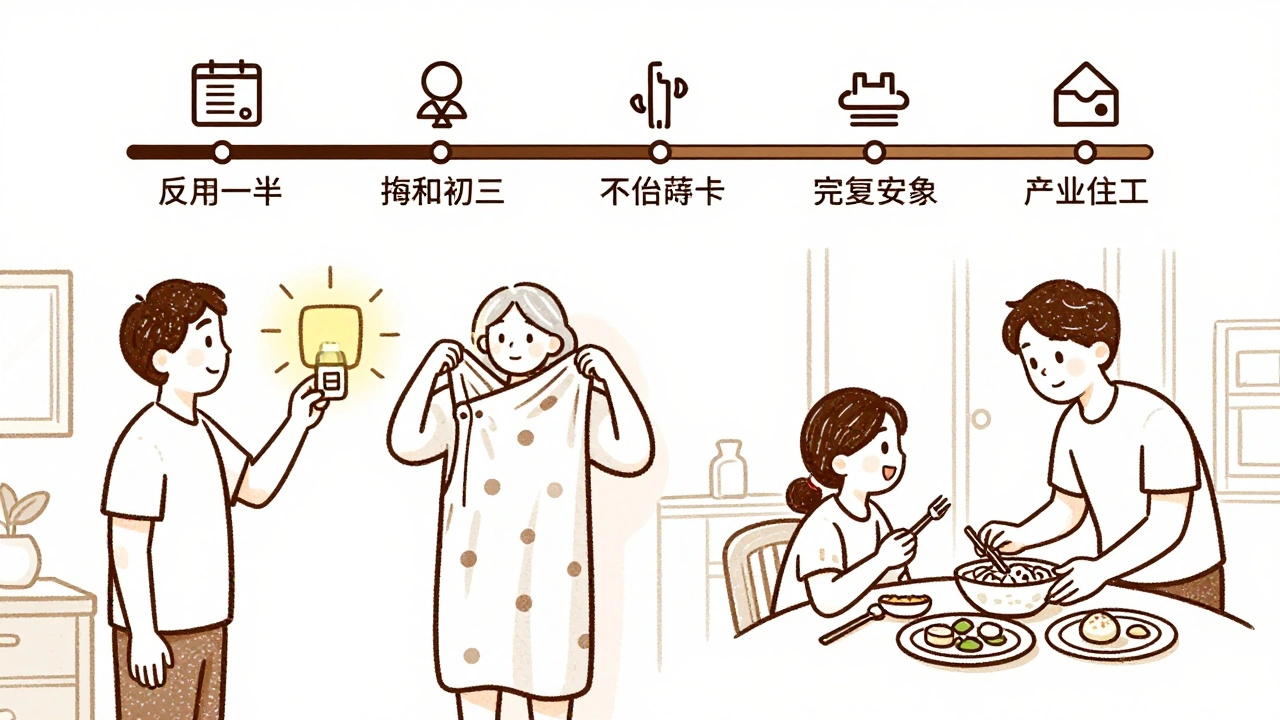
Phase 3: Adaptation (Months to Years)
Some functions won’t fully come back. That’s not failure-it’s reality. This phase is about adjusting. You might need grab bars in the bathroom, a raised toilet seat, or a kitchen with pull-out shelves. You might learn to dress one-handed or use voice commands to control your lights. The goal isn’t to go back to who you were before. It’s to build a new life that works with what you have now. Family involvement makes a huge difference here. People with active family support stick to their rehab routines 37% more often.
The Team That Makes Recovery Possible
No single therapist can do it all. Stroke recovery needs a crew. The American Stroke Association says the best outcomes come from teams that meet regularly and talk to each other. That means:
- Physiotherapists focus on walking, balance, and strength. They use robotic walkers, electrical stimulation, and balance boards.
- Occupational therapists teach you how to eat, bathe, dress, and cook again. They modify your home and teach you new ways to do old tasks.
- Speech-language pathologists handle trouble speaking, understanding, or swallowing. Up to 40% of stroke survivors have swallowing issues-this is critical to prevent pneumonia.
- Psychologists help with depression, anxiety, and frustration. About one in three stroke survivors develop depression. It’s not just sadness-it’s a medical barrier to recovery.
- Nurses, nutritionists, and social workers manage medications, diet, insurance, and long-term care planning.
Facilities that hold weekly team meetings see 22% better functional outcomes than those that don’t. Communication isn’t a nice-to-have-it’s the backbone of recovery.

Technology That’s Changing Recovery
Rehab isn’t just about pushing through exercises anymore. Technology is making it smarter, more engaging, and more effective.
- Robotic devices like the Lokomat help you walk with perfect form, even if you can’t lift your leg yet. Studies show 50% better walking speed gains than traditional therapy.
- Virtual reality turns rehab into a game. Patients reach for virtual fruit, dodge obstacles, or catch falling objects. This boosts upper limb function by 28% compared to standard care.
- Functional electrical stimulation sends tiny pulses to paralyzed muscles, making them contract. It’s helped people regain wrist movement they thought was gone forever-gains of 25-45% in hand strength.
- Wireless activity monitors track how many steps you take each day. Seeing your progress on a phone app motivates people to move more. One study showed a 32% increase in daily steps just from wearing one.
- Transcranial magnetic stimulation (TMS) uses magnetic pulses to stimulate brain areas involved in movement. When combined with therapy, it adds 15-20% more recovery in arm and hand function.
These aren’t gimmicks. They’re backed by clinical trials. And they’re becoming more accessible-not just in big hospitals, but in community clinics and even at home.
What Actually Drives Success?
It’s not just the therapy. It’s you. Research from Merck Manuals shows that motivation accounts for up to 40% of how well someone recovers. That doesn’t mean you need to be cheerful all the time. It means you need to show up. Even on the hard days.
Here are the nine factors that predict recovery success:
- General health before the stroke
- Range of motion in joints
- Muscle strength
- Bowel and bladder control
- Pre-stroke independence (could you drive? cook? manage money?)
- Home and social support
- Ability to learn new skills
- Motivation
- How you cope with stress and change
If you’re tired, depressed, or feel like giving up, that’s normal. But don’t let it stop you. Small wins matter. Moving your fingers 5 degrees more this week? That’s progress. Standing for 10 seconds without help? That’s a win. Celebrate them.
What Happens After Discharge?
Most people leave the hospital or rehab center after a few weeks. But recovery doesn’t stop there. About 70% of stroke survivors need ongoing therapy. That’s where community programs and telerehabilitation come in.
Recent studies show that virtual rehab-exercises done at home with a therapist guiding you via video-works just as well as in-person sessions for 85% of tasks. You can do balance drills, arm exercises, speech practice, even cognitive games from your couch. This is huge for people who live far from clinics or have trouble getting around.
But you still need structure. Set a schedule. Treat rehab like a job. Three hours a day, five days a week, is the gold standard. If you can’t do that at home, find a local community center with a stroke rehab group. Social connection is part of the therapy.
What to Avoid
Recovery is full of myths. Here’s what not to do:
- Don’t wait to start. Delaying therapy by even a few days can cost you mobility and independence.
- Don’t overdo it. Fatigue slows recovery. Balance rest (30-40% of your day), therapy (40-50%), and social time (20-30%).
- Don’t ignore mental health. Depression isn’t weakness-it’s a brain injury symptom. Ask for help.
- Don’t assume you’re done when you leave rehab. Recovery can continue for years. Keep moving, keep challenging yourself.
Hope Is Real
There’s no magic cure. But there’s science. There’s progress. There’s recovery-even if it’s slow, even if it’s different from before. The brain doesn’t forget how to heal. It just needs the right conditions: time, repetition, support, and a reason to keep going.
People walk again. They speak clearly. They cook their own meals. They go back to hobbies they thought were lost. It’s not guaranteed. But it’s possible. And the tools to make it happen are better now than ever before.

All Comments
Ali Bradshaw December 4, 2025
This is the kind of post that actually makes you feel like there’s hope. I’ve seen my uncle go through this, and the difference between starting rehab the same day vs. waiting a week was night and day. He went from barely moving his arm to holding a coffee cup in 6 weeks. Don’t sleep on the first 24 hours.
luke newton December 5, 2025
You people act like stroke recovery is some kind of moral achievement. Newsflash: most people who recover well had good insurance, a supportive family, and didn’t smoke for 30 years. Meanwhile, my cousin got hit at 42, worked two jobs, and now can’t even hold a spoon. Don’t glorify recovery like it’s a reward for being ‘good’.
an mo December 5, 2025
The 35% mobility gain stat is cherry-picked. The NIH meta-analysis from 2021 showed only 18% when controlling for pre-stroke BMI and comorbidities. Also, robotic devices? That’s Big Rehab pushing $$$ tech on Medicare. Most patients get 15 mins of PT a day and a pamphlet.
Annie Grajewski December 6, 2025
so like... you're telling me if i just do the same dumb exercises over and over my brain will magically fix itself? like wow. i thought it was magic. turns out its just... repetition. and therapy. and motivation. and a whole team. and technology. and family. and not being depressed. oh and also not dying. got it.
aditya dixit December 8, 2025
There’s a quiet dignity in the slow rebuild. Not every victory is a walk across the room. Sometimes it’s just remembering your own name after the fog lifts. Or choosing to eat breakfast even when your arm shakes so bad you spill the milk. That’s not recovery-it’s rebellion. And it’s beautiful.
Lynette Myles December 10, 2025
They don’t want you to know that TMS is funded by neurotech corporations who also own the rehab centers. The FDA approved it on a 7-person pilot. Your ‘science’ is a marketing campaign.
Jimmy Jude December 12, 2025
I just want to say-this isn’t about strokes. This is about the human spirit. The soul’s refusal to die. When your body breaks, your soul has to decide: do I give up, or do I crawl through hell with a spoon in my hand and a prayer on my lips? I’ve seen both. And the ones who heal? They didn’t just do therapy. They chose to live. Every. Single. Day.
Mark Ziegenbein December 12, 2025
Look I’ve read every study on neuroplasticity since 2017 and let me tell you the entire rehabilitation industrial complex is built on a lie. The brain doesn’t rewire it just compensates through cortical hijacking and synaptic redundancy and the reason you see 30% gains from constraint-induced therapy is because the control groups were given placebo exercises with no intensity tracking and the fMRI data was misaligned due to motion artifacts from patients who couldn’t hold still because they were in chronic pain from unmanaged spasticity which was never properly quantified in the original trials so all these numbers are basically statistical noise dressed up as hope and I’m sorry but I can’t unsee it
Laura Saye December 13, 2025
I work in outpatient neuro rehab. The quietest victories? A woman who hadn’t spoken in 6 months said ‘thank you’ to the aide who helped her bathe. A man who couldn’t lift his leg used his toes to tap out ‘Happy Birthday’ on his wheelchair armrest. These aren’t metrics. They’re miracles. Keep showing up-even when no one’s watching.