Breast Cancer Treatment Decision Tool
Personalized Treatment Recommendation
Answer a few questions about your situation to get a recommendation for the most appropriate breast cancer treatment option based on current guidelines.
When doctors treat estrogen‑receptor‑positive (ER+) breast cancer, Tamoxifen is often the first drug they reach for. Tamoxifen citrate is a selective estrogen receptor modulator (SERM) that blocks estrogen from binding to tumor cells, slowing their growth. It has been the backbone of endocrine therapy for over four decades, but newer options now sit alongside it. This guide walks you through how Tamoxifen stacks up against its main alternatives, helping patients and clinicians see where each drug shines or falls short.
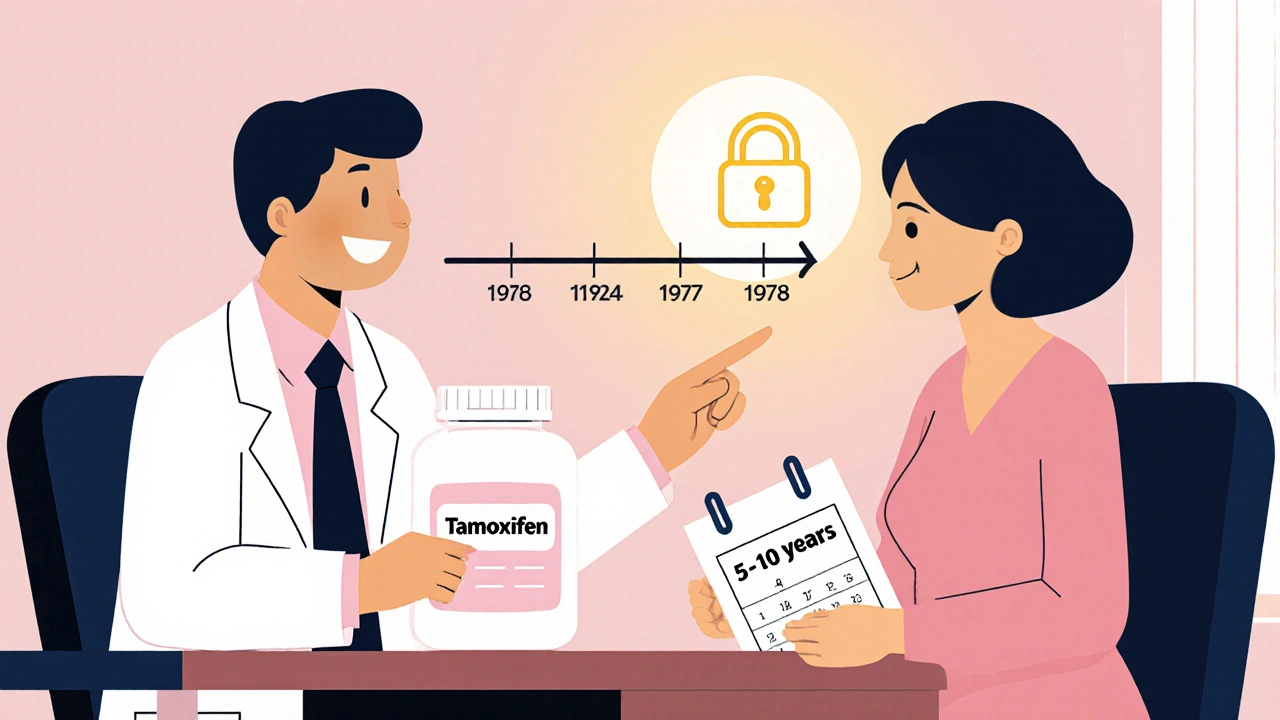
Why Tamoxifen Became a Standard
Tamoxifen was approved in the UK in 1977 and the US in 1978. Its oral form makes it easy to take daily for 5‑10 years, and it works for pre‑menopausal women as well as post‑menopausal patients. The drug reduces recurrence risk by roughly 40 % and improves overall survival. Side‑effects like hot flashes, night sweats, and a small increase in blood‑clot risk are well‑documented, but most patients can manage them with lifestyle tweaks or short‑term medication.
Key Alternatives on the Market
In recent years, doctors have added several other endocrine agents to the toolbox. The biggest groups are aromatase inhibitors (AIs) and newer SERMs or selective estrogen receptor degraders (SERDs). Below are the most common alternatives:
- Aromatase inhibitors - block estrogen production in post‑menopausal women.
- Anastrozole - a non‑steroidal AI used daily.
- Letrozole - another non‑steroidal AI, often chosen for its slightly longer half‑life.
- Exemestane - a steroidal AI that irreversibly disables the aromatase enzyme.
- Fulvestrant - a SERD injected monthly, used when tumors become resistant to other endocrine drugs.
- Raloxifene - a SERM mainly for osteoporosis, but with some breast‑cancer preventive power.
- Clomifene - an older SERM rarely used now for cancer, more for fertility.
Side‑Effect Profiles at a Glance
Every drug has trade‑offs. Understanding the most common adverse events helps patients weigh comfort against efficacy. Here’s a quick snapshot:
- Tamoxifen: hot flashes, vaginal dryness, menstrual irregularities, ↑ risk of deep‑vein thrombosis, rare endometrial cancer.
- Aromatase inhibitors: joint pain, bone loss, cholesterol changes, occasional liver‑enzyme elevation.
- Fulvestrant: injection‑site pain, nausea, fatigue, sometimes liver‑enzyme rise.
- Raloxifene: similar to Tamoxifen but lower endometrial risk; still can cause hot flashes.
Choosing the right drug often means balancing these effects with a patient’s age, bone health, and personal preferences.
Direct Comparison Table
| Drug | Class | FDA/UK Approval Year | Typical Duration | Key Side‑Effects |
|---|---|---|---|---|
| Tamoxifen | SERM | 1977 (UK), 1978 (US) | 5-10 years (adjuvant) | Hot flashes, blood clots, endometrial changes |
| Anastrozole | Aromatase Inhibitor | 1995 (UK), 1997 (US) | 5-10 years | Joint pain, osteoporosis risk, cholesterol shift |
| Letrozole | Aromatase Inhibitor | 1997 (UK), 1998 (US) | 5-10 years | Bone loss, hot flashes, fatigue |
| Exemestane | Steroidal Aromatase Inhibitor | 1999 (UK), 1999 (US) | 5-10 years | Joint stiffness, weight gain, liver‑enzyme rise |
| Fulvestrant | SERD | 2002 (UK), 2002 (US) | Until progression | Injection site pain, nausea, liver‑enzyme rise |
| Raloxifene | SERM (osteoporosis) | 2000 (UK), 2000 (US) | 3-5 years (prevention) | Hot flashes, leg cramps, rare DVT |
When to Stick With Tamoxifen
If you’re a pre‑menopausal woman, Tamoxifen remains the go‑to choice because aromatase inhibitors need post‑menopausal estrogen levels to work. It’s also preferred when bone density is a concern-AIs can accelerate osteoporosis. In patients with a history of blood‑clot issues, however, clinicians may tilt toward an AI after careful risk assessment.
When Alternatives Might Be Better
For post‑menopausal patients who experience severe hot flashes or who have a uterus with atypical hyperplasia, swapping to an AI like Anastrozole often improves quality of life and reduces the rare endometrial cancer risk tied to Tamoxifen. If a tumor becomes resistant after several years of Tamoxifen, doctors often switch to Fulvestrant or add a CDK4/6 inhibitor (e.g., Palbociclib) to regain control.
Practical Decision Checklist
- Is the patient pre‑ or post‑menopausal?
- Does the patient have osteoporosis or low bone density?
- Is there a history of deep‑vein thrombosis or endometrial abnormalities?
- How tolerable are hot flashes and other estrogen‑related symptoms?
- Has the tumor shown any sign of endocrine resistance?
Answering these questions helps you or your oncologist pick the drug that fits best. The right choice is rarely a one‑size‑fits‑all; it’s a balance of effectiveness, side‑effects, and personal health goals.
Future Directions in Hormone Therapy
Researchers are testing oral SERDs that could one‑day replace both Tamoxifen and Fulvestrant. Early trials of drugs like Elacestrant show promise for patients whose cancers no longer respond to traditional SERMs or AIs. Until those agents get regulatory approval, the current lineup-Tamoxifen, AIs, and SERDs-will continue to dominate treatment plans.
Bottom Line: Picking the Right Tool
Both Tamoxifen and its alternatives have solid data behind them. If you need a quick, cheap, and well‑understood pill, Tamoxifen stays hard to beat, especially for younger women. For those who can tolerate a few more pills or an injection and want to avoid certain side‑effects, an aromatase inhibitor or Fulvestrant might feel like a better fit. Discuss these points with your care team, weigh the pros and cons, and remember that adjustments are common as treatment progresses.
Frequently Asked Questions
Can I switch from Tamoxifen to an aromatase inhibitor after a few years?
Yes. Many oncologists move patients to an AI after 2‑3 years of Tamoxifen, especially if hot flashes become bothersome or if bone health is stable. The switch is usually safe, but your doctor will monitor cholesterol and joint symptoms closely.
Is Tamoxifen effective for metastatic breast cancer?
Tamoxifen can still slow disease spread in ER+ metastatic cases, but newer agents like Fulvestrant, CDK4/6 inhibitors, or combination AI therapy often give better control. Choice depends on prior treatments and side‑effect tolerance.
Do aromatase inhibitors increase the risk of heart disease?
AIs may raise cholesterol slightly, but large studies show no major rise in heart‑attack rates compared with Tamoxifen. Still, patients with existing heart risk factors should have lipid panels monitored regularly.
Why does Tamoxifen sometimes cause blood clots?
Tamoxifen has a mild estrogen‑like effect on liver proteins that help clotting. This raises the chance of deep‑vein thrombosis by about 1‑2 %. The risk stays low, but doctors advise staying active and reporting leg swelling promptly.
Can I take Tamoxifen while on hormone replacement therapy?
Combining Tamoxifen with estrogen‑based hormone replacement is not recommended because the added estrogen can counteract Tamoxifen’s blocking action. If menopausal symptoms are severe, non‑hormonal options like SSRIs are usually suggested.
All Comments
Rajesh Singh October 18, 2025
It’s astonishing how the medical community can champion a drug like Tamoxifen while glossing over the darker side‑effects that haunt many patients. The hot flashes and clot risk aren’t just minor inconveniences; they are vivid reminders that we trade comfort for survival. We ought to demand transparent counseling, not just a prescription and a hopeful smile. Ultimately, the choice should be guided by conscience as much as by chemistry.
Albert Fernàndez Chacón October 19, 2025
From a practical standpoint, Tamoxifen remains a solid first‑line option for ER+ patients, especially when you consider its long‑term safety profile. The drug’s oral administration makes adherence easier, and the side‑effect spectrum is well documented. While aromatase inhibitors offer bone‑health trade‑offs, many clinicians start with Tamoxifen to gauge tolerance before switching. It’s a balanced approach that respects both efficacy and patient comfort.
Drew Waggoner October 20, 2025
The constant buzz of hot flashes feels like an unwelcome soundtrack that never stops, draining energy and morale. Even when the statistics look good on paper, the lived experience can be a relentless tide of discomfort that few truly acknowledge.
Mike Hamilton October 22, 2025
One could argue that choosing a hormone therapy is less about chemistry and more about navigating the human condition. If we view the body as a narrative, Tamoxifen writes a chapter of resistance against estrogen's plot. Yet, the plot twists-like clot risk-remind us that no story is without conflict. In many cultures, the balance between treatment and quality of life is a dance we must all learn.
Matthew Miller October 23, 2025
Alright, let’s cut to the chase-Tamoxifen is the tried‑and‑true workhorse, but the new AI crew brings some serious firepower! If bone health is a concern, swapping to an aromatase inhibitor can be a game‑changer. And for those who can handle a monthly injection, Fulvestrant packs a punch when resistance shows up. Bottom line: there’s a toolbox full of options, so grab the right hammer for the job!
Liberty Moneybomb October 24, 2025
But what they won’t tell you is that the pharma giants are pushing these “new” drugs to keep the cash flowing, fearing Tamoxifen’s cheapness might topple their empire. The silent agenda behind the glossy brochures is as unsettling as a phantom limb.
Alex Lineses October 25, 2025
As a supportive coach, I’d recommend mapping out the patient’s risk profile using a comprehensive toxicity index before making a switch. Leveraging pharmacogenomic data can also pinpoint which endocrine agent aligns best with individual metabolism. This evidence‑based stratification ensures you’re not just guessing, but delivering personalized oncology care.
Brian Van Horne October 26, 2025
In short, Tamoxifen still holds its ground.
Norman Adams October 27, 2025
Oh, absolutely-because nothing screams cutting‑edge science like a pill from the 1970s.
Margaret pope October 28, 2025
Totally understand how overwhelming all these options can feel many patients just need a steady hand and clear guidance you’re doing a great job
Karla Johnson October 29, 2025
The comparative analysis of Tamoxifen versus the newer aromatic inhibitors is more than a mere list of side‑effects; it is a strategic roadmap for survivorship.
First, the pharmacodynamics of a SERM like Tamoxifen versus an AI such as Letrozole differ fundamentally in how they modulate estrogen pathways.
Tamoxifen’s partial agonist activity in uterine tissue creates a unique risk profile that demands vigilant gynecologic monitoring.
In contrast, aromatase inhibitors achieve systemic estrogen depletion, which can accelerate bone demineralization if not countered with bisphosphonates.
Moreover, the selection algorithm must weigh menopausal status, as pre‑menopausal physiology renders AI therapy ineffective without ovarian suppression.
Clinical trials have repeatedly shown that overall survival benefits between Tamoxifen and AIs converge after long‑term follow‑up, yet quality‑of‑life metrics diverge sharply.
Patients plagued by relentless hot flashes often report higher adherence to AI regimens despite the joint pain they may endure.
Conversely, individuals with a prior history of thromboembolic events find the clot‑risk associated with Tamoxifen intolerable.
The economic dimension cannot be ignored either; generic Tamoxifen represents a cost‑effective backbone for health systems with limited resources.
Still, the newer oral SERDs promise to simplify administration while targeting resistant disease, potentially reshaping the treatment paradigm.
From a health‑policy perspective, the decision matrix should incorporate both direct drug costs and indirect expenses linked to managing adverse events.
Physicians must also consider the psychosocial impact of daily pill burden versus monthly injections, as patient preference heavily influences compliance.
In practice, a sequential approach-starting with Tamoxifen and transitioning to an AI after two to three years-has become a widely accepted compromise.
However, this strategy should be individualized; there is no one‑size‑fits‑all prescription in oncology.
Ultimately, the clinician’s role is to synthesize pharmacologic data, patient comorbidities, and personal values into a coherent, patient‑centered plan.
Ignoring any of these variables would be a disservice to the very individuals we aim to heal.