Depression in Teenagers is a mental health condition characterized by persistent low mood, loss of interest, and functional impairment in adolescents aged 13‑19. It affects roughly 1 in 7 teens in the United States, according to the National Institute of Mental Health, and often goes unnoticed because symptoms overlap with typical teenage behaviour.
Why Early Detection Matters
When left untreated, teen depression can spiral into academic failure, substance misuse, self‑harm, and even suicide. Early recognition gives families and clinicians a chance to intervene with therapy, medication, or school‑based support before the condition becomes chronic.
Core Warning Signs to Watch
Below are the most common clusters of symptoms. Each cluster is a distinct entity with its own attributes, yet they often intersect, creating a unique warning pattern for each youngster.
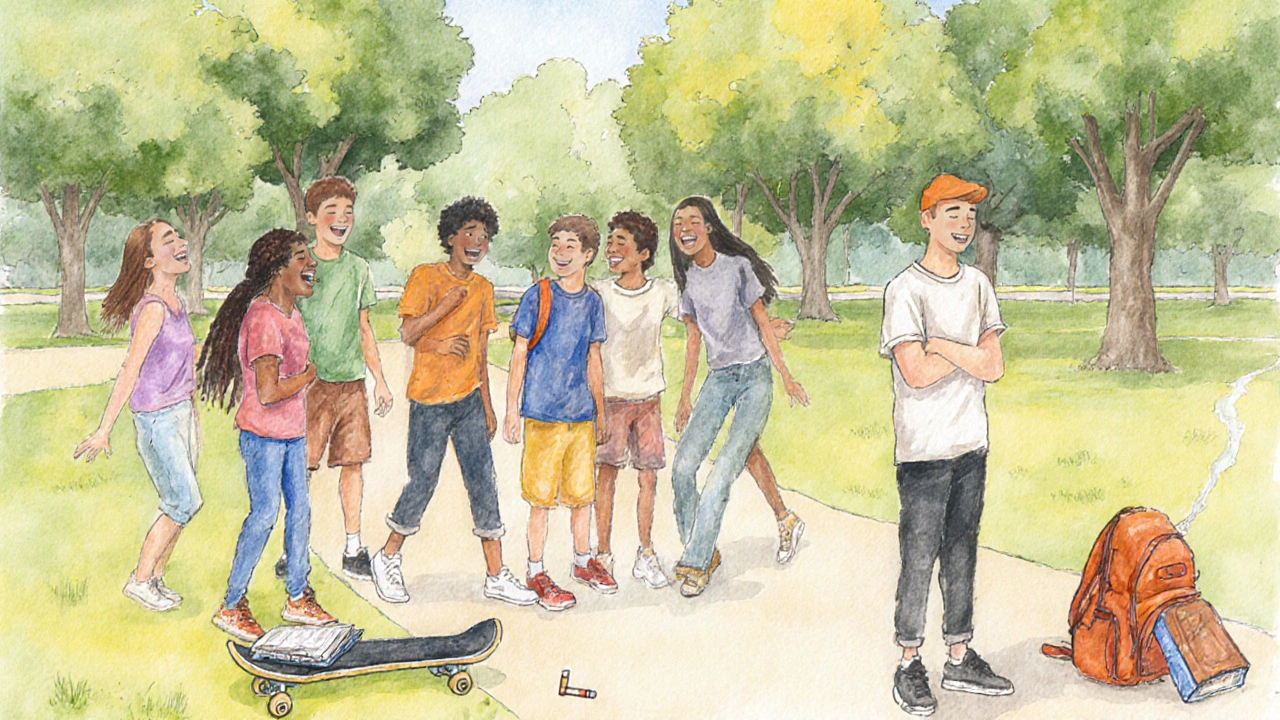
- Anhedonia loss of pleasure in activities once enjoyed - sudden disinterest in sports, music, or hanging out with friends.
- Irritability heightened anger or agitation, often mistaken for typical teenage rebellion - frequent arguments, snapping at family members over minor issues.
- Sleep Disturbance insomnia or oversleeping that disrupts daily routines - staying up all night scrolling, then struggling to get up for school.
- Appetite Changes significant weight loss or gain unrelated to dieting - skipping meals or binge‑eating as a coping mechanism.
- Academic Decline dropping grades, missed assignments, or loss of concentration - suddenly failing subjects that were once strong.
- Social Withdrawal isolating from friends, avoiding social events - declining invites, disappearing from group chats.
- Self‑Harm cutting, burning, or other deliberate injury - hidden bruises, secretive behavior around mirrors.
- Suicidal Ideation talking about death, hopelessness, or making death‑related plans - statements like "I wish I wasn't here" or leaving a note.
Notice that many of these signs overlap with anxiety, substance use, or family conflict. The key is the persistence and intensity: symptoms lasting more than two weeks and interfering with daily life signal a deeper issue.
Comparing Depression with Normal Mood Swings
| Feature | Typical Mood Swings | Clinical Depression |
|---|---|---|
| Duration | Hours‑to‑days | Weeks‑months |
| Intensity | Mild‑moderate, context‑dependent | Severe, pervasive, often without clear trigger |
| Impact on Functioning | Usually temporary; school performance recovers | Marked decline in grades, attendance, and relationships |
| Physical Symptoms | Occasional fatigue | Sleep disturbances, appetite changes, aches |
| Thought Content | Negative thoughts about a specific event | Hopelessness, worthlessness, suicidal thoughts |
The table makes it clear why parents should treat persistent, severe symptoms as more than “just a phase.”
Underlying Factors That Can Trigger Symptoms
Depression seldom appears out of thin air. Several risk factors often converge, shaping the symptom profile.
- Genetics: A family history of mood disorders increases odds by up to 40%.
- Neurochemical Imbalance: Low serotonin or dopamine levels can manifest as irritability and anhedonia.
- Trauma: Bullying, abuse, or the loss of a loved one accelerates depressive episodes.
- Chronic Stress: Academic pressure, social media comparison, or family discord fuels anxiety‑depression cycles.
- Substance Use: Alcohol, cannabis, or prescription misuse can mask or worsen depressive signs.
Understanding these causes helps clinicians tailor interventions-whether it’s cognitive‑behavioral therapy for trauma or medication for neurochemical issues.
How to Approach a Teen Showing Symptoms
Effective communication is the cornerstone. Below is a step‑by‑step guide that parents, teachers, or coaches can follow.
- Choose a calm, private setting. Avoid distractions like phones or TV.
- Start with observations, not accusations. Example: “I’ve noticed you’ve been staying up late and seem more withdrawn lately.”
- Listen without judgment. Validate feelings: “That sounds really tough.”
- Ask direct, open‑ended questions about mood and thoughts of self‑harm. If they say, “I don’t know,” gently probe further.
- Offer concrete help: schedule a visit with a school counselor, a pediatrician, or a teen‑focused mental‑health clinic.
- Follow up regularly. A quick text checking in can reinforce support and catch worsening symptoms early.
When a teen expresses suicidal thoughts, treat it as an emergency. Contact a crisis line, a mental‑health professional, or call emergency services.
Treatment Options and What to Expect
Effective treatment blends psychotherapy, medication, lifestyle adjustments, and community support.
- Cognitive‑Behavioral Therapy (CBT): Teaches skills to reframe negative thoughts; typically 12‑20 weekly sessions.
- Interpersonal Therapy (IPT): Focuses on relationship issues that may fuel depression.
- Medication: Selective serotonin reuptake inhibitors (SSRIs) are first‑line; careful monitoring for side‑effects is crucial.
- Physical Activity: Regular exercise can boost endorphins and improve sleep quality.
- Sleep Hygiene: Consistent bedtime, limited screen time before sleep, and a cool dark room reduce insomnia.
Recovery timelines vary. Some teens feel relief within weeks; others need months of combined therapy. Persistence and a supportive environment are the best predictors of long‑term improvement.
Related Concepts and Next Steps
Beyond immediate symptoms, several adjacent topics deepen understanding of teen mental health:
- Anxiety Disorders often co‑occur with depression and amplify irritability and sleep problems
- Substance Abuse can both mask depressive signs and act as a self‑medication strategy
- Family Therapy addresses systemic issues like conflict or communication breakdowns that contribute to teen depression
- School‑Based Programs such as peer‑support groups and mental‑health curricula, reduce stigma and provide early screening
Readers interested in the broader picture might explore “how anxiety fuels depressive episodes” or “effective school interventions for at‑risk youth.” Those ready to act can locate local mental‑health resources, schedule a pediatric evaluation, or join a support network for parents.
Frequently Asked Questions
What are the first signs that a teen may be depressed?
Early clues include persistent sadness, loss of interest (anhedonia), irritability, changes in sleep or appetite, and withdrawing from friends or activities.
How is teen depression different from a normal teenage ‘mood swing’?
Mood swings are brief, context‑dependent, and usually don’t impair school performance. Depression lasts weeks or months, is intense, and can cause academic decline, self‑harm, or suicidal thoughts.
When should I call emergency services for my teen?
If your teen talks about suicide, shows a plan, or engages in self‑harm, treat it as an emergency. Call 911 or go to the nearest emergency department right away.
Can medication help my teenager?
Selective serotonin reuptake inhibitors (SSRIs) are the most common prescription for teen depression. They can reduce symptoms within 2‑4 weeks, but need close monitoring for side‑effects like increased agitation.
What role does school play in identifying depression?
Teachers and counselors often notice changes in attendance, grades, or social interaction. Many schools now have mental‑health screenings and peer‑support programs that can flag concerns early.

All Comments
Maude Rosièere Laqueille September 27, 2025
Parents often wonder how to differentiate normal teenage mood swings from clinical depression. The key is persistence: symptoms lasting more than two weeks and interfering with daily life are red flags. Look for a combination of anhedonia, irritability, sleep changes, and academic decline. Early intervention can prevent escalation to self‑harm or suicidal thoughts. A calm conversation that validates feelings while noting these patterns is a good first step.
Amanda Joseph September 27, 2025
Oh great, another teen moody drama, like we needed more drama in the house.
Kevin Aniston September 27, 2025
When you sit down with a teenager who is showing signs of depression, the conversation should start in a safe, distraction‑free space. Begin by sharing observable changes without attaching blame, for example, "I've noticed you seem more withdrawn and your sleep pattern has shifted recently." Acknowledging their experience validates their feelings and opens a channel for honesty. It's essential to listen actively, using reflective statements like "That sounds really tough" to show empathy. After they feel heard, gently ask about any thoughts of self‑harm, using non‑threatening language such as "Sometimes when people feel this low, they think about hurting themselves. Have you had any thoughts like that?" If they express any intent or plan, treat it as an emergency and contact crisis services immediately. When the teen is ready, discuss concrete steps for professional help, whether it’s a school counselor, pediatrician, or a specialized teen mental‑health clinic. Explain that therapy, such as cognitive‑behavioral therapy, can equip them with tools to reframe negative thoughts and manage stress. If medication is considered, emphasize the importance of close monitoring for side effects like increased agitation. Encourage lifestyle adjustments too: regular physical activity, consistent sleep hygiene, and reduced screen time before bed can noticeably improve mood. Follow‑up is crucial; a quick text or check‑in after appointments shows ongoing support. Involving the family in therapy sessions can also address systemic issues that may perpetuate the depression. Remember, recovery timelines differ; some teens notice improvement within weeks, others take longer, but persistence and a supportive environment are the best predictors of long‑term improvement. Lastly, remind them that seeking help is a sign of strength, not weakness, and that many resources are available to guide them through this challenging period.
kiran kumar September 27, 2025
People love to label any teen moodiness as depression and rush to medicate it it seems like a trend to over‑diagnose everything no need for all that pharma hype we should be teaching resilience not handing out pills
Brian Johnson September 27, 2025
Observing a teen's daily routine can reveal subtle shifts that point to deeper struggles. A sudden drop in participation in activities they once loved, combined with irregular sleep, often signals more than a phase. Noting these changes early allows parents to approach the conversation with compassion rather than confrontation. Maintaining this gentle observation helps build trust, which is essential for any subsequent intervention.
Jessica Haggard September 27, 2025
It’s vital for parents to set clear, supportive boundaries while encouraging open dialogue. Let your teen know you’re there to listen without judgment and that seeking professional help is a sign of strength. Create a family plan that includes regular check‑ins and concrete steps toward therapy or counseling. This proactive stance empowers the teen and reinforces a safe environment.
Alan Clark September 27, 2025
Hey folks, stay positive! Even when teens feel down, a little optimism and a supportive vibe can make a world of difference. Small wins like a short walk or a hobby can lift mood faster than you think.
Mark Anderson September 27, 2025
Let’s paint a vivid picture: imagine a teen standing at the edge of a stormy sea, the waves of anxiety crashing around them. With the right support-therapy, friendship, a dash of creative expression-they can learn to surf those waves instead of being swept away. Encouragement isn’t just a word; it’s a lifeline that can transform despair into determination.
Shouvik Mukherjee September 27, 2025
Supporting a teen through depression means fostering an inclusive environment where they feel heard and valued. Encourage them to share experiences, and remind them that cultural and community resources are available to aid recovery. Gentle guidance can empower them to seek help without feeling isolated.
Ben Hooper September 27, 2025
Early signs are key, watch for lasting sadness and withdrawal.
Marjory Beatriz Barbosa Honório September 27, 2025
Every small step forward is a victory, even if it feels quiet. Celebrate progress, no matter how modest, and keep the conversation gentle but steady. You’re not alone in this journey; together we can nurture hope.