Switching to generic medications isn’t just about saving money-it’s about getting the same effective treatment at a fraction of the cost. If you’ve ever stared at a pharmacy receipt and wondered why your blood pressure pill costs $4 instead of $130, you’re not alone. Millions of people in the U.S. and beyond make this switch every year, and for good reason. The truth is, generic drugs aren’t cheaper because they’re worse. They’re cheaper because they don’t carry the weight of decades of marketing, patent protection, and R&D costs that brand-name drugs do.
They’re the Same Medicine, Just Without the Brand Name
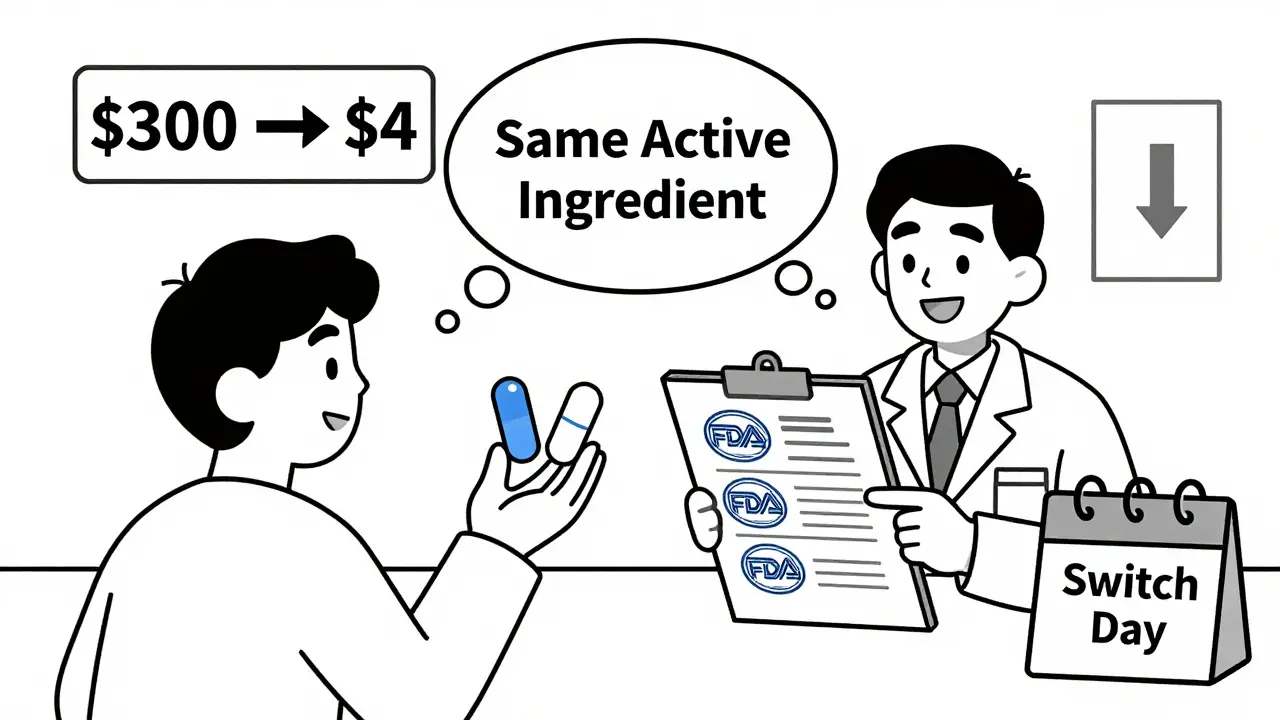
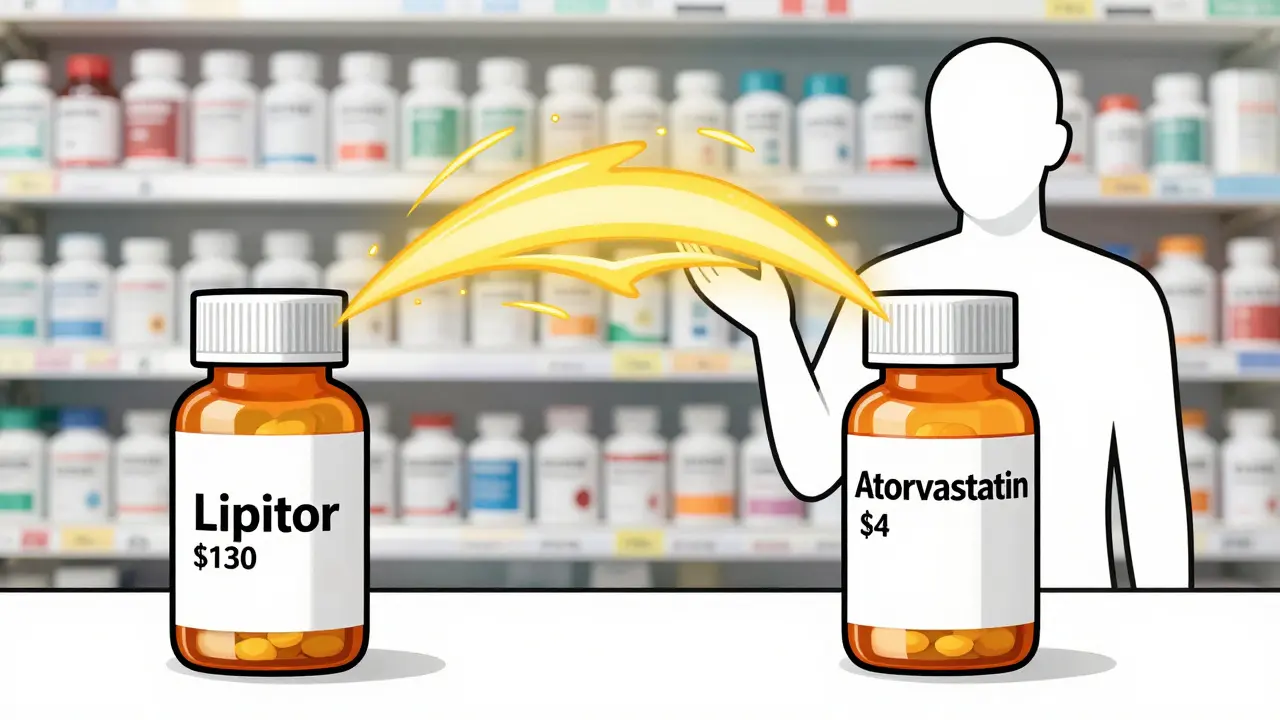
When you take a generic version of a drug like atorvastatin (the generic for Lipitor) or metformin (the generic for Glucophage), you’re getting the exact same active ingredient, in the same strength, and the same way your body absorbs it. The U.S. Food and Drug Administration (FDA) requires generics to prove they’re bioequivalent-meaning they deliver the same amount of medicine into your bloodstream at the same speed as the brand-name version. That’s not a suggestion. It’s a legal requirement.
Think of it like buying a generic battery instead of a name-brand one. Same voltage. Same lifespan. Same performance. The packaging might look different, the color might be off, but it still powers your remote. Generics work the same way. The FDA inspects manufacturing sites worldwide, conducts over 1,200 inspections a year, and only approves generics that meet the same quality standards as the original.
Cost Savings Are Real-Sometimes Life-Changing
The difference in price isn’t just noticeable-it’s dramatic. For example, the brand-name blood thinner Coumadin used to cost over $300 for a 30-day supply. The generic version, warfarin? Around $4. The antihistamine Allegra? $30. Its generic, fexofenadine? $10. And Lipitor? At its peak, $130 a month. Today, the generic version costs as little as $4 at major pharmacies.
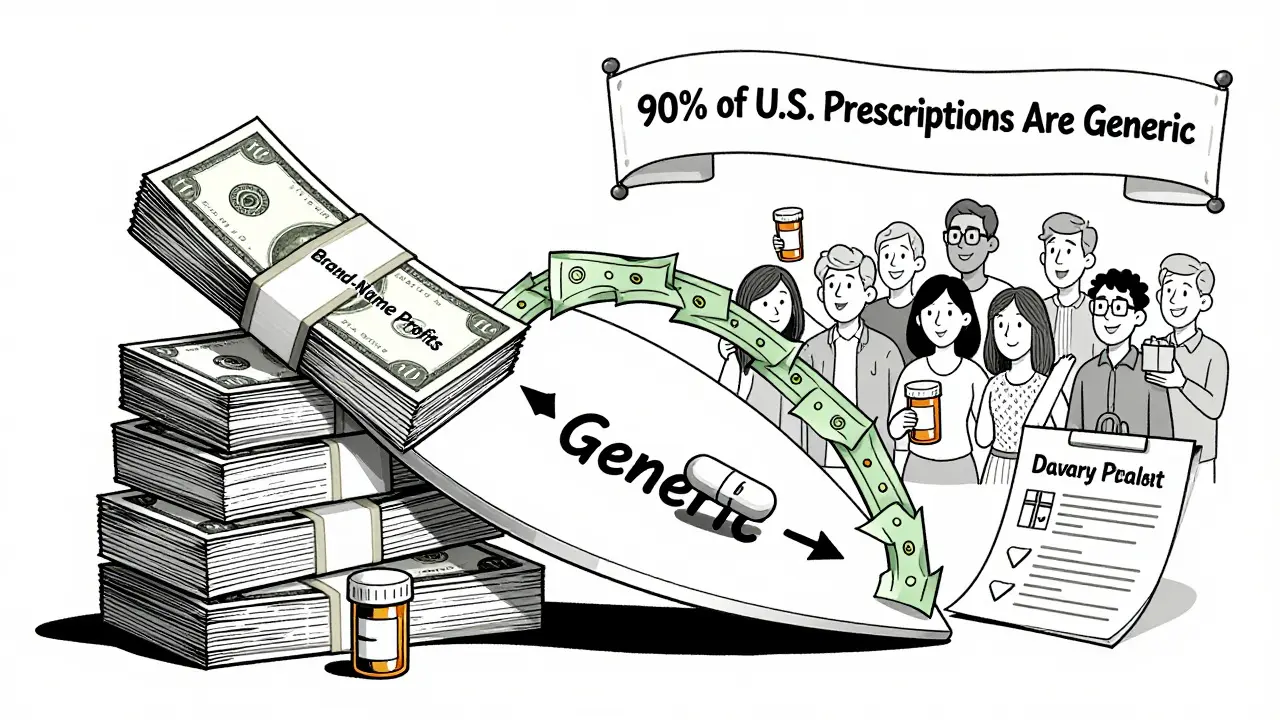
Across the board, generic drugs cost 80% to 85% less than their brand-name counterparts. According to the FDA, generics saved the U.S. healthcare system $1.67 trillion between 2012 and 2022. That’s not a guess. That’s official data. And it’s not just helping big insurers-it’s helping people like you pay for their prescriptions without choosing between medicine and groceries.
A 2023 study found that patients using generics were 68% less likely to skip doses because of cost. That’s huge. Skipping doses because you can’t afford your meds doesn’t just hurt your health-it leads to more hospital visits, more emergency care, and higher overall costs down the line. Generics keep people on their treatment plans.
Doctors and Experts Agree: Generics Work Just as Well
Some people worry that generics might not be as effective. But the science says otherwise. A 2022 study in the Journal of Managed Care & Specialty Pharmacy looked at thousands of patients taking generic vs. brand-name heart medications. No difference in effectiveness. No increase in side effects. No drop in control of blood pressure or cholesterol.
Even in high-stakes areas like cardiovascular care, where consistency matters, generics performed just as well. Dr. Aaron Kesselheim from Harvard Medical School reviewed data from 186,000 patients and concluded: “Our research confirms that generic cardiovascular drugs perform as well as their brand-name counterparts.”
The American Medical Association officially recommends prescribing generics when appropriate-not because they’re cheaper, but because they’re just as safe and effective. The FDA’s former director, Dr. Janet Woodcock, put it plainly: “Generic drugs undergo rigorous review to ensure they are as safe and effective as brand-name drugs.”
What About Those Weird-Looking Pills?
One common concern is that the pill you’ve been taking suddenly looks different. Maybe it’s a different color, shape, or has a different imprint. That doesn’t mean the medicine changed. It means your pharmacy switched to a different generic manufacturer.
Generic manufacturers aren’t required to make their pills look like the brand-name version. That’s why you might get a blue pill one month and a white one the next. But the active ingredient? Still the same. The dose? Still the same. The effect? Still the same.
Some patients feel anxious when this happens-especially older adults or those managing chronic conditions. That’s normal. But it’s not a medical issue. It’s a psychological one. Talk to your pharmacist. Ask them to explain the change. They’re trained to help with this. Most insurance plans even require pharmacists to counsel patients during the switch.
Insurance Plans Push Generics-Because They Save Money
Your insurance company doesn’t just prefer generics-they often require them. Most plans have a tiered system: generics are in Tier 1, with the lowest copay. Brand-name drugs? Tier 3 or 4, with much higher costs. Humana’s 2023 data shows average copays of $1-$10 for generics versus $25-$75 for brand-name drugs.
Medicare Part D beneficiaries pay an average of $1.85 per generic prescription. For brand-name drugs? $33.67. That’s an 88% difference. If you’re on Medicare, switching to generics isn’t just smart-it’s often the only way to stay on your meds without breaking the bank.
Hospitals and pharmacies follow the same logic. Over 99% of hospitals and 98% of retail pharmacies automatically substitute generics when allowed by law. It’s not a conspiracy. It’s basic economics-and it’s working.
What About Complex Drugs? Are There Exceptions?
Most drugs are fine. But there are a few exceptions. Some medications have a narrow therapeutic index (NTI), meaning even tiny changes in blood levels can affect how well they work or increase side effects. Examples include warfarin (blood thinner), levothyroxine (thyroid), and certain seizure medications.
Even here, the FDA says approved generics are safe. But some specialists, like neurologists treating epilepsy, recommend sticking with the same generic manufacturer once you’ve found one that works. Why? Because while all generics meet the same standard, slight differences in inactive ingredients can affect absorption in rare cases. That’s why your doctor might say, “Stick with this brand of generic.” It’s not about the drug being better-it’s about consistency.
If you’re on one of these medications, don’t panic. Just ask your pharmacist: “Is this the same manufacturer as last time?” If it’s not, let your doctor know. They can write “Dispense as written” on the prescription if needed.
Generics Are the Future-And They’re Already Here
The market for generics is growing fast. In 2023, generics made up 90.3% of all prescriptions dispensed in the U.S.-but only 23.1% of total drug spending. That’s the power of competition. When five or more companies start making the same generic, prices drop by nearly 85%.
And it’s not stopping. Biosimilars-generic versions of complex biologic drugs like insulin and rheumatoid arthritis treatments-are now approved by the FDA. As of December 2023, 37 biosimilars are on the market. The Congressional Budget Office estimates they could save $300 billion over the next decade.
The FDA’s 2023 Drug Competition Action Plan is actively removing barriers to generic entry, especially for hard-to-copy drugs like inhalers and topical creams. With new rules cutting review times to 10 months for priority applications, more generics will reach shelves faster.
How to Switch-Step by Step
- Check your prescription. Does it say “Dispense as written”? If not, your doctor already allowed substitution.
- Ask your pharmacist: “Is there a generic version available?” They’ll know instantly.
- Compare prices. Use apps like GoodRx or your pharmacy’s loyalty program to find the lowest cost.
- Ask if your insurance requires a generic. Most do.
- If you’re on a narrow therapeutic index drug, ask your doctor if you should stick with one manufacturer.
- Don’t panic if the pill looks different. Call your pharmacist if you’re unsure.
Switching doesn’t take weeks. It doesn’t require blood tests or adjustments. For most people, it’s as simple as picking up the next refill.
Final Thought: It’s Not a Compromise. It’s a Smart Choice.
Switching to generic medications isn’t settling. It’s not giving up. It’s choosing to get the same medical benefit without paying a premium for branding, advertising, and corporate profits. You’re not sacrificing safety. You’re not sacrificing effectiveness. You’re just saving money-sometimes hundreds of dollars a month.
If your doctor says a generic is right for you, trust them. If your pharmacist says it’s the same, believe them. And if your wallet thanks you, don’t second-guess it.
Are generic medications as safe as brand-name drugs?
Yes. The FDA requires generic drugs to meet the same strict standards for safety, strength, quality, and performance as brand-name drugs. They must prove bioequivalence-meaning they deliver the same active ingredient at the same rate and amount into your bloodstream. Adverse event reports for generics are proportional to their usage, showing no higher risk than brand-name versions.
Why do generic pills look different?
Generic manufacturers aren’t required to copy the appearance of brand-name drugs. Differences in color, shape, or imprint are due to different inactive ingredients or manufacturing choices. These changes don’t affect how the medicine works. If you’re concerned, ask your pharmacist to confirm it’s the same medication.
Can I switch to a generic anytime?
In most cases, yes. Your doctor usually allows substitution unless they specifically write “Dispense as written.” Pharmacists can switch you to a generic at refill time unless you or your doctor object. If you’re on a narrow therapeutic index drug (like warfarin or levothyroxine), your doctor may recommend sticking with one manufacturer for consistency.
Do insurance plans cover generics?
Yes-and they often require it. Most insurance plans have lower copays for generics, sometimes as low as $1-$10, compared to $25-$75 for brand-name drugs. Medicare Part D beneficiaries pay an average of $1.85 per generic prescription versus $33.67 for brand-name drugs.
Are there any drugs where generics aren’t recommended?
For most drugs, generics are equally effective. But for medications with a narrow therapeutic index-like certain seizure drugs, blood thinners, or thyroid medications-some doctors recommend sticking with one manufacturer once you’ve found a version that works well for you. This isn’t because generics are unsafe, but because small differences in absorption can matter in these cases. Always discuss this with your doctor.
All Comments
Priya Patel January 10, 2026
Just switched my mom to generic levothyroxine last month and she’s been fine-no weird symptoms, no crashes. She even said the pills are easier to swallow now. Who knew saving $80 a month could feel this good?
Sean Feng January 11, 2026
Generics are a scam. I’ve had mine switch to a different brand and my anxiety spiked. They’re not the same. The FDA doesn’t know what they’re doing.
Priscilla Kraft January 13, 2026
Hey Sean, I get your concern-but have you talked to your pharmacist about the specific manufacturer? Sometimes it’s just the filler that throws people off. I had the same issue with my blood pressure med until I stuck with the same generic brand. Now it’s smooth sailing 😊
Alfred Schmidt January 14, 2026
Oh wow, another one of those ‘trust the system’ fairy tales. You think the FDA is some saintly watchdog? They’re underfunded, overworked, and pressured by Big Pharma to greenlight generics before they’re ready. I’ve seen people have seizures after switching. No one talks about that.
Michael Patterson January 14, 2026
Look, I’m not anti-generic, but let’s be real here-when you’re talking about drugs with a narrow therapeutic index, like warfarin or phenytoin, you’re playing Russian roulette with your life. One manufacturer uses a different binder, the dissolution profile shifts by 5%, and suddenly your INR is 8.5 and you’re in the ER. The FDA says it’s ‘bioequivalent,’ but bioequivalent doesn’t mean identical, and for some of us, that 5% difference is the difference between life and death. So yeah, I stick with the brand. I’d rather pay $130 than end up in a hospital bed because someone at a pharmacy thought ‘close enough’ was good enough.
Matthew Miller January 15, 2026
Michael, you’re not special. You’re just scared of saving money. Your ‘life-or-death’ story is anecdotal nonsense. If generics were that dangerous, hospitals wouldn’t use them for 99% of prescriptions. You’re not protecting your health-you’re protecting your ego.
Jennifer Littler January 17, 2026
From a clinical pharmacy perspective: the data is overwhelming. A 2023 meta-analysis of 57 studies on NTI drugs showed no significant difference in clinical outcomes between branded and generic formulations when patients were stabilized on a single generic. The real issue? Polypharmacy and inconsistent switching. When patients get switched back and forth between manufacturers, that’s when variability creeps in-not because generics are inferior, but because we’re not managing transitions properly. Pharmacist counseling is key. If your provider doesn’t offer it, ask for it.
Jason Shriner January 17, 2026
So let me get this straight… you’re telling me I can get the same drug for $4… but the pill is a different color? And that’s supposed to be comforting? Next they’ll tell me my Tesla is just a Honda with a sticker.
Vincent Clarizio January 18, 2026
Let’s go deeper. The real tragedy isn’t that generics are underused-it’s that we’ve been conditioned to equate price with quality. We’ve been sold the myth that expensive = better for decades. That’s not medicine. That’s marketing. And now we’re paying for it-in our wallets, our health, and our future. The fact that a $4 pill can keep someone alive while a $130 pill sits on a shelf because they can’t afford it? That’s not a healthcare system. That’s a moral failure dressed in white coats. Generics aren’t a workaround. They’re the only ethical choice.
Sam Davies January 19, 2026
Ah yes, the American healthcare system-where the cheapest option is also the most scientifically validated. How quaint. In the UK, we just get the NHS to sort it out. No drama. No panic. Just a bloody good pill at £1.20. You lot really do love a good crisis, don’t you?
Alex Smith January 19, 2026
Sam, you’re right about the UK-no one there loses sleep over pill color. But here? We’re trained to distrust anything that doesn’t come in a fancy box. I switched my dad to generic statins last year. He was terrified. Now he jokes that his ‘blue pill’ is his new best friend. The real win? He’s not skipping doses anymore. That’s the point. It’s not about branding. It’s about access.