Prostate Medication Safety Checker
This tool helps you assess your risk of urinary retention when taking anticholinergic medications based on prostate size and symptoms. Please note: This is informational only and not medical advice. Always consult your doctor before changing medications.
Medication Risk Assessment
Why Anticholinergics Can Be Dangerous for Men with Prostate Problems
If you’re a man over 60 and your doctor prescribed an anticholinergic for an overactive bladder, you might not realize you’re putting yourself at serious risk. These drugs - meant to stop sudden urges to pee - can actually lock your bladder shut if you have an enlarged prostate. It’s not a rare side effect. It’s a known, documented danger that happens more often than most doctors admit.
Anticholinergics like oxybutynin, tolterodine, and solifenacin work by blocking the signal that tells your bladder to contract. That sounds helpful if you’re leaking urine from sudden spasms. But if your prostate is enlarged - which affects nearly half of men over 60 - your bladder is already struggling to push urine past the blockage. Adding an anticholinergic is like turning off the engine while you’re stuck in traffic. The result? Complete urinary retention. You can’t pee at all. Your bladder swells, sometimes to over a liter of urine. You end up in the ER with a catheter stuck in you.
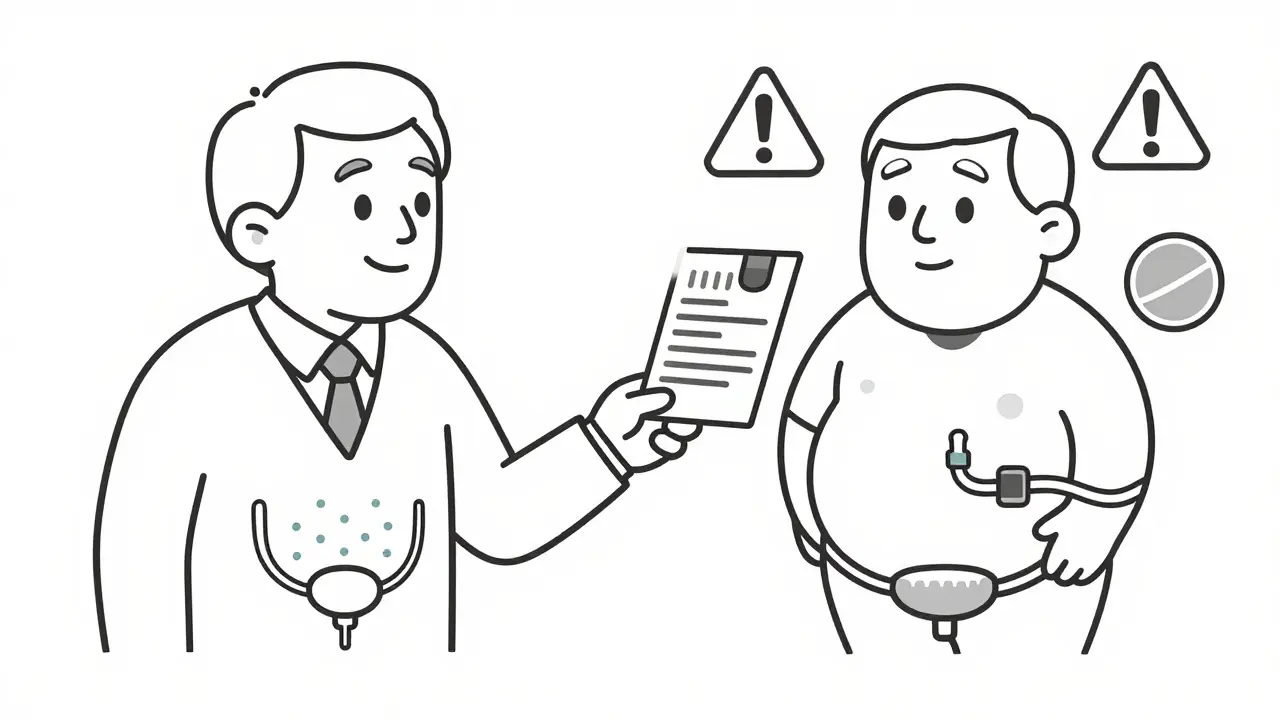
How Anticholinergics Interact with an Enlarged Prostate
Benign prostatic hyperplasia (BPH) isn’t just about a bigger prostate. It’s about your bladder working overtime. The prostate squeezes the urethra, so the bladder muscle (detrusor) has to contract harder just to get urine out. Over time, this muscle gets weak, stretched, or overworked. It’s already at its limit.
Anticholinergics don’t just reduce urgency - they reduce the bladder’s ability to contract at all. When you add these drugs to an already compromised system, you’re not just slowing things down. You’re shutting down the last bit of function the bladder has left. Studies show men with BPH who take anticholinergics are 2.3 times more likely to develop acute urinary retention than those who don’t.
It’s not theoretical. Between 2018 and 2022, over 1,200 cases of urinary retention linked to anticholinergics were reported to the FDA. Sixty-three percent of those cases were in men over 65 with diagnosed BPH. One Reddit user, sharing his experience on r/ProstateHealth, wrote: "I was on Detrol for three weeks. One morning, I couldn’t pee at all. They had to catheterize me. I still have a catheter now. I didn’t know it could do this."
The Real Numbers: How Often Does This Actually Happen?
Doctors often say side effects like dry mouth or constipation are "common." But when it comes to urinary retention, the numbers are alarming:
- 8-15% of patients on anticholinergics report difficulty urinating - that’s 1 in 7 people.
- In men with BPH, the rate of acute retention jumps to 18-28% in unselected populations.
- Only 12% of men with mild BPH and strict monitoring had retention on solifenacin, according to one 2017 study - but that still means 1 in 8.
- By comparison, mirabegron (Gemtesa) and vibegron - newer bladder drugs - have retention rates under 5% in the same group.
And here’s the kicker: anticholinergics only offer a 15% better improvement in symptoms than placebo. That means for every 7 men treated, only one gets one less leak per day. Is that worth a 1 in 5 chance of being unable to pee?
What the Experts Say - And Why They’re Warning Against These Drugs
Dr. Roger Dmochowski, a leading urologist at Vanderbilt, says anticholinergics should be considered contraindicated in men with moderate to severe lower urinary tract symptoms. The American Urological Association’s 2018 guidelines say the same: avoid these drugs if your prostate is over 30 grams or your symptom score is above 20.
Dr. Jerry Blaivas put it bluntly: "The detrusor muscle in men with BPH is already working at maximum capacity to overcome obstruction; adding an anticholinergic is like removing the engine from a car that’s struggling to climb a hill."
There’s one exception some doctors argue for: men with very mild BPH and clear overactive bladder symptoms - not just urgency, but confirmed detrusor overactivity on urodynamics. Even then, they recommend low doses, monthly bladder scans, and immediate discontinuation if retention occurs.
But here’s the problem: most patients don’t get that level of testing. Digital rectal exams? Uroflowmetry? Post-void residual checks? These are rarely done before prescribing. Instead, a man gets a script for oxybutynin because his doctor thinks, "It’s just a bladder pill."
What You Should Do Instead
If you have BPH and overactive bladder symptoms, there are better, safer options:
- Alpha-blockers like tamsulosin (Flomax) or alfuzosin (Uroxatral) relax the prostate and bladder neck. They work fast - within days. Studies show men on alpha-blockers after catheterization are 30-50% more likely to void successfully within 2-3 days.
- 5-alpha reductase inhibitors like finasteride or dutasteride shrink the prostate over time. They take months to work, but reduce the risk of acute retention by 50% over four to six years.
- Beta-3 agonists like mirabegron (Myrbetriq) and vibegron (Gemtesa) stimulate bladder relaxation without blocking contractions. They don’t interfere with the detrusor’s ability to push urine out. Retention rates are under 5% - a fraction of anticholinergic risk.
These aren’t "alternatives." They’re the standard of care for men with BPH. Anticholinergics should be a last resort - and only after urodynamic testing confirms true detrusor overactivity.
What to Ask Your Doctor Before Taking Any Bladder Medication
If you’re being offered an anticholinergic, don’t just say yes. Ask these questions:
- "Have you checked my prostate size?"
- "What’s my peak urine flow rate?"
- "What’s my post-void residual?"
- "Is there a chance this could cause me to completely stop peeing?"
- "What’s the safer alternative?"
If your doctor doesn’t know your uroflowmetry numbers or hasn’t done a digital rectal exam, walk out. This isn’t about being difficult. It’s about avoiding a trip to the ER.
What Happens If You Already Have Retention?
If you’ve had urinary retention - even once - you should never take an anticholinergic again. Once you’ve had it, your risk of it happening again skyrockets.
Acute retention requires immediate catheterization. Studies show you don’t need to drain the bladder slowly. Empty it completely. Then, start an alpha-blocker right away. Without it, 70% of men will have another episode within a week.
The American Geriatrics Society’s Beers Criteria lists anticholinergics as "potentially inappropriate" for older adults with BPH or urinary retention. And yet, 40% of nursing home residents with these conditions are still getting them. That’s not negligence - it’s ignorance.
The Future: Safer Drugs Are Here
The tide is turning. Vibegron (Gemtesa), approved by the FDA in 2020, works differently. It doesn’t block signals - it activates a natural relaxation pathway in the bladder. Clinical trials show it reduces urgency episodes by 92% with almost no retention risk.
Research is also moving toward personalized medicine. The NIDDK is funding studies using prostate MRI and genetic markers to predict who might safely use anticholinergics. But right now, the safest answer is simple: if you have prostate enlargement, avoid these drugs.
Market data shows anticholinergic prescriptions for men over 65 with BPH are already dropping 35% by 2028. Why? Because doctors are finally listening. And patients are speaking up.
Final Takeaway: Don’t Let a "Bladder Pill" Put You in the Hospital
Overactive bladder is frustrating. But urinary retention is terrifying. You don’t need a miracle drug. You need a safe one.
Anticholinergics have a place - but not in men with prostate issues. If you’re on one, talk to your doctor. Ask about your prostate size, your flow rate, and your alternatives. If they brush you off, get a second opinion.
Your bladder doesn’t need to be stronger. It needs to be unblocked. And that’s not what these pills do.
Can anticholinergics cause permanent bladder damage?
Repeated episodes of urinary retention can stretch the bladder muscle beyond its ability to recover. If the bladder stays overdistended for too long, it can lose its ability to contract properly, leading to chronic retention. This may require lifelong catheterization or surgery. While not always permanent, the damage can be long-lasting if not treated quickly.
Is there a safe anticholinergic for men with BPH?
There is no anticholinergic that’s truly safe for men with BPH. Even "selective" ones like solifenacin carry a 12-28% risk of retention in this group. Guidelines from the AUA and European Association of Urology recommend avoiding them entirely. Safer alternatives like mirabegron and alpha-blockers exist and should be tried first.
How do I know if my prostate is enlarged?
Your doctor can assess prostate size with a digital rectal exam (DRE). For a more precise measurement, a prostate ultrasound or MRI can show volume. A prostate over 30 grams is considered enlarged. Symptoms like weak stream, straining to urinate, or frequent nighttime urination also suggest BPH.
What are the signs of urinary retention?
Signs include a strong urge to urinate but being unable to start, feeling like your bladder is full even after trying, lower abdominal pain or pressure, and leakage of small amounts of urine (overflow incontinence). Acute retention often comes on suddenly and is painful. If you can’t pee after 8-12 hours, seek emergency care.
Can I stop anticholinergics cold turkey?
You should never stop these medications suddenly without talking to your doctor. Abruptly stopping can cause rebound bladder spasms or worsen incontinence. But if you’re experiencing urinary symptoms, stop immediately and contact your doctor. They can help you taper safely while switching to a safer alternative.
All Comments
Dan Pearson February 2, 2026
Bro, I was on oxybutynin for three months and woke up one morning like my bladder had become a water balloon. ER. Catheter. Total humiliation. My urologist acted like it was my fault for not reading the tiny print. Newsflash: most people don’t read the 37-page FDA warning. This isn’t a side effect-it’s a trap. And doctors keep prescribing it like it’s Advil.
Bob Hynes February 3, 2026
damn. i had no idea this was a thing. i thought these pills were just for ‘oops i peed a little’ moments. my dad got catheterized last year and they never told him about the prostate thing. he’s still mad he didn’t get a warning. canada’s got the same drugs but no one talks about this. we need better patient education. like, seriously.
Akhona Myeki February 4, 2026
Let me be absolutely clear: this is not a medical issue-it’s a systemic failure. The pharmaceutical industry markets these drugs with glossy brochures and celebrity endorsements while the fine print is buried under seven layers of legalese. In South Africa, we call this ‘medical colonialism’-exporting dangerous treatments to aging populations because the alternative is too expensive to study. Anticholinergics are not ‘bladder pills.’ They are chemical locks on a broken system.
And yet, here we are. Nurses in Johannesburg report the same pattern: elderly men with BPH, prescribed solifenacin, admitted within weeks with urinary retention. The WHO should issue a red alert. This isn’t negligence. It’s profit-driven negligence.
Chinmoy Kumar February 5, 2026
hey i just wanted to say thank you for writing this. my uncle had this happen last year and we thought it was just ‘old age stuff’ until we found out it was the med. now he’s on tamsulosin and its like night and day. he can pee again!! i shared this with my mom and she’s gonna ask her doc about switching from detrol. i think more people need to know this. its not just me being paranoid.
Brett MacDonald February 5, 2026
so if the bladder is a car engine and the prostate is the transmission… and anticholinergics are the ignition key being pulled out while you’re driving uphill… then what’s mirabegron? a hybrid motor? a self-driving system? i’m trying to understand the metaphor here because i feel like i’m missing the point.
Sandeep Kumar February 5, 2026
anticholinergics are for weak men who cant handle their own bladder. real men use alpha blockers and drink less coffee. also why is everyone acting like this is new info? its in every urology textbook since 2010. if you dont know this you shouldnt be prescribing or taking meds. end of story
Gary Mitts February 7, 2026
Been there. Done that. Got the catheter.
Doc said ‘it’s just a pill.’
Turns out it’s a trap.
Don’t be the guy who finds out the hard way.
Anthony Massirman February 7, 2026
bro i saw this post and immediately called my dad’s urologist. he’s been on oxybutynin for two years. we asked for a uroflow test. turns out his post-void residual was 420 mL. like… four cups of pee stuck in there. they switched him to vibegron last week. he says he feels like a 40-year-old again. if you’re on one of these drugs and you’re over 60-ask for the test. it takes 10 minutes. could save you from a catheter.
Vatsal Srivastava February 7, 2026
you think this is bad wait till you hear about how mirabegron is just a placebo with a fancy name and the real reason retention rates are low is because the trials excluded anyone with actual BPH. also alpha blockers cause retrograde ejaculation so you’re trading one problem for another. the real solution is fasting and cold showers. science says so.
Brittany Marioni February 9, 2026
Thank you, thank you, thank you-for writing this with such clarity, compassion, and courage. So many men (and their families) are suffering in silence because they don’t know this is preventable. Please, if you’re reading this and you’re a healthcare provider: listen. Listen to your patients. Ask about prostate size. Do the flow test. Don’t assume. Don’t rush. Don’t prescribe blindly. And if you’re a patient: speak up. You have a right to know. You have a right to safety. You are not ‘just getting older.’ You are a person with a body that deserves to function properly.
phara don February 10, 2026
my grandma was on one of these and ended up in the hospital. she said the doctor just handed her the script like it was a candy. i cried when i saw her with the catheter. i’m sharing this with my whole family. maybe someone else won’t have to go through this. 😢