Beta‑Tubulin Binding: Quick Guide for Patients and Professionals
Ever wonder why some chemotherapy drugs are called "tubulin inhibitors"? It all comes down to beta‑tubulin binding. When a drug latches onto beta‑tubulin, it can either stop cells from dividing or cause them to die. That sounds scary, but it’s also the reason many life‑saving treatments work.
What is beta‑tubulin binding?
Beta‑tubulin is one half of the tubulin protein that makes up micro‑tubules – the tiny scaffolding that helps cells keep their shape, move, and split during division. Some medicines fit like a key into a specific spot on the beta‑tubulin subunit. When they bind, they change how the micro‑tubule grows or shrinks. Taxanes (like paclitaxel) lock the micro‑tubule in place, while vinca alkaloids (like vincristine) prevent it from forming at all.
Because cancer cells divide faster than normal cells, they’re more vulnerable to this disruption. That’s why beta‑tubulin binding is a powerful way to attack tumors. But it also means healthy cells—especially those in the gut lining, hair follicles, and bone marrow—can get hit too, leading to side effects.
Why does beta‑tubulin binding matter for drug safety?
If a drug binds strongly to beta‑tubulin, it may have a higher chance of causing neuropathy, nausea, or hair loss. Knowing the binding profile helps doctors pick the right dose and manage side effects. Some newer agents are designed to target specific beta‑tubulin isoforms that are more common in cancer cells, aiming to spare normal tissue.
Safety isn’t just about side effects. Interactions with other meds can change how much of the drug reaches beta‑tubulin. For example, certain antifungals can boost levels of taxanes, increasing toxicity. Always tell your prescriber about every product you use – from over‑the‑counter painkillers to herbal supplements.
On the upside, understanding beta‑tubulin binding lets researchers create better drugs. By tweaking the molecule, they can improve how tightly it latches onto cancer‑specific beta‑tubulin while reducing the grip on normal cells. This is the science behind next‑generation chemotherapy and some experimental treatments for neurodegenerative diseases.
If you’re reading about a drug and see "beta‑tubulin binding" mentioned, ask yourself:
- Is the medication meant for cancer, or is it being studied for another use?
- What side effects are linked to its binding strength?
- Do I need extra monitoring or dose adjustments?
Our tag page gathers all the latest posts where beta‑tubulin binding comes up. Check out these articles for deeper insight:
- BPH Symptoms and Mental Health – while not about tubulin, it shows how side effects can impact wellbeing.
- Herbal Remedies for Bladder Pain – a reminder that even natural products can interfere with drug metabolism.
- How and Where to Buy Haldol Online Safely in the UK (2025 Guide) – safety tips for antipsychotics that also affect neurotransmission.
- Megalis (Tadalafil): What It Is, Safe Dosage, Side Effects, and UK‑Friendly Alternatives – illustrates dose‑checking, a habit you’ll need for tubulin‑targeting drugs.
- Luvox (Fluvoxamine) for OCD – shows drug‑interaction awareness, essential when you’re on complex chemotherapy.
Got questions about a specific medication’s beta‑tubulin binding? Use our search bar or drop us a line. We’ll break down the science, the risks, and what you can do to stay safe while getting the most out of your treatment.
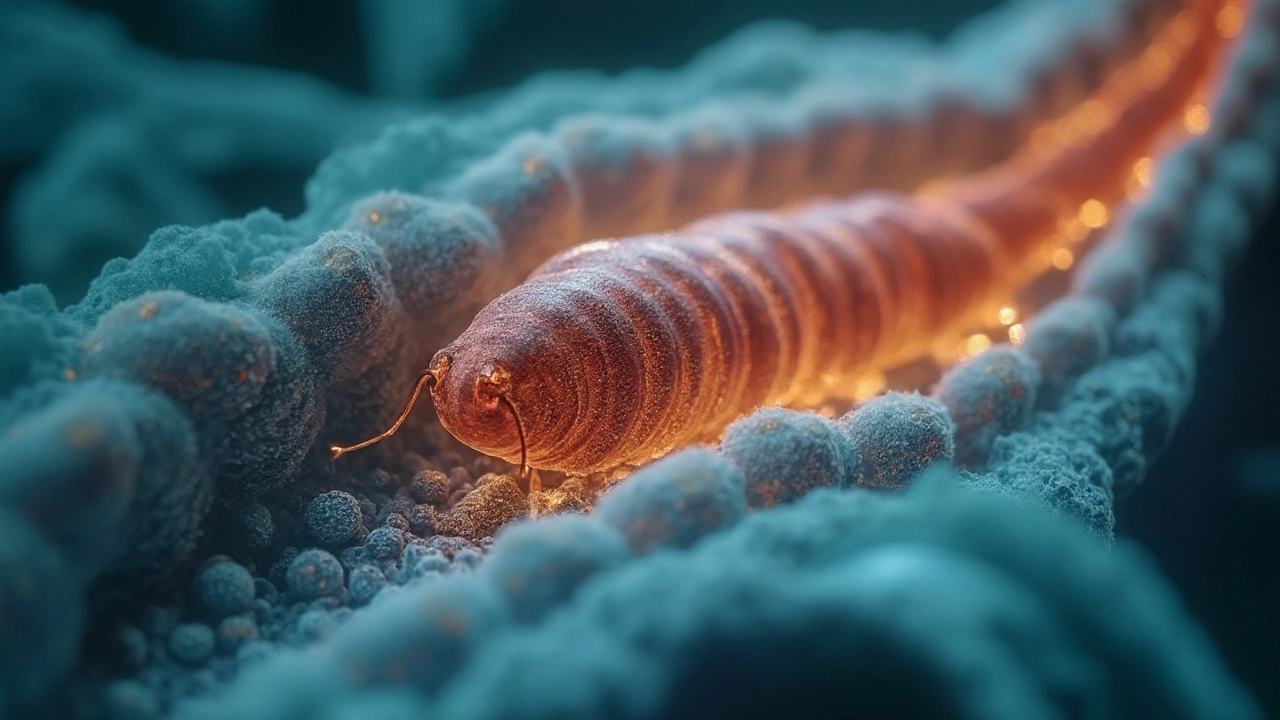
Albendazole Mechanism of Action Explained: How It Kills Parasites and Stays Safe for Humans
- Cheryl Moran
- September 5, 2025
- 8 Comments
Clear, practical explainer on how albendazole works: microtubule disruption, energy starvation, selectivity, resistance, food effects, and real-world tips for 2025.
read more